Definition
Keratoconus, derived from the Greek words "kerato" (cornea) and "konos" (cone), is an eye condition that progressively alters the structure of the cornea, resulting in impaired vision. Normally, the cornea has a clear, dome-like structure that focuses light entering the eye. In keratoconus, the corneal layer thins and gradually protrudes into a cone shape, causing blurred vision, double vision, nearsightedness, and irregular astigmatism. This condition typically begins at puberty and can progress into the mid-20s, developing slowly over 10 years or more.
Causes
The exact cause of keratoconus remains unknown, but it is believed to result from a combination of genetic, environmental, and hormonal factors. One theory suggests that a decrease in antioxidants, which protect the cornea from harmful substances and maintain collagen integrity, leads to keratoconus. Collagen fibers in the cornea help maintain its shape. When antioxidant levels drop, collagen fibers are damaged, causing the cornea to weaken and protrude in a cone-like shape.
Risk Factor
Risk factors for keratoconus include family history. Individuals with a family history of keratoconus should have their children's eyes checked regularly. Age is also a risk factor, the condition often appears during adolescence but can begin as early as age 10. While less common, it can also develop in adults aged 30 to 40.
Other conditions associated with keratoconus include atopic diseases (such as allergic dermatitis, allergic rhinitis, and asthma), Down syndrome, and connective tissue disorders (like Ehlers-Danlos syndrome and osteogenesis imperfecta) are linked to keratoconus. Habits such as frequent and prolonged eye rubbing is also a risk factor.
Symptoms
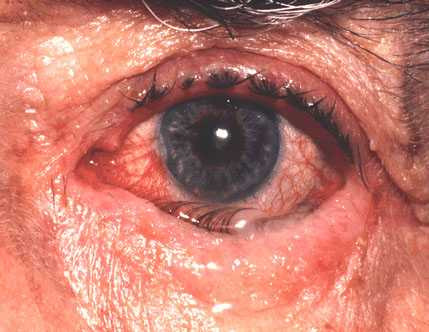
Early symptoms of keratoconus include blurred vision and increased light sensitivity. Initially, these symptoms can be mistaken for refractive eye disorders. As the condition progresses, vision deteriorates further, often accompanied by irregular astigmatism. Keratoconus usually affects both eyes, but one eye may exhibit more rapid progression. Additional symptoms include persistent eye irritation, eye pain, double vision, eye strain, and difficulty seeing at night. Refractive issues such as nearsightedness, astigmatism, and farsightedness can also be indicative of keratoconus.
Diagnosis
Diagnosing keratoconus involves an in-depth discussion with patients to know about the main complaint, vision issues, and family history of eye diseases.
Subsequently, eye physical examination is conducted to assess visual acuity. This can be done using a Snellen chart. Measuring the curvature of the cornea can be done by keratometry, the doctor would direct a circular light to the cornea and measure the shadow to know the shape of the cornea. The reflection is analyzed to detect irregular astigmatism in keratoconus. Slit-lamp examination is conducted to evaluate the shape of the cornea. Another test is corneal topography, mapping the cornea's curvature and thickness using a special computer to diagnose keratoconus.
Management
The treatment for keratoconus varies based on the severity and progression of the condition, encompassing both surgical and non-surgical approaches. Non-surgical methods typically involve the use of glasses or soft contact lenses to improve blurred vision and correct mild astigmatism. As the condition worsens, rigid contact lenses may replace the initial corrective lenses.
For surgical interventions, corneal transplantation is a viable option, particularly for the 11% to 27% of cases where vision correction with glasses or contact lenses becomes ineffective. The cornea's lack of direct blood flow allows for donor corneas without matching blood types. Another surgical alternative is corneal ring implantation, where a ring is inserted into the cornea to flatten its conical shape. Corneal collagen cross-linking is a newer surgical procedure aimed at strengthening the cornea.
Radial keratotomy, a surgical procedure that creates incisions in the cornea to reshape it. This procedure was once used for treating nearsightedness but is now more commonly replaced by LASIK for farsightedness. However, LASIK is contraindicated for individuals with corneal thinning, such as those with keratoconus.
Complications
Complications from keratoconus typically arise after significant changes in the cornea's shape. These complications include corneal swelling, scarring, and a substantial decrease in vision. Severe keratoconus can lead to corneal hydrops, characterized by sudden corneal cloudiness due to edema from a tear in the weakened corneal layer, resulting in painful symptoms and vision loss. Additional complications include infection, poor wound healing, transplant rejection reactions, irregular astigmatism, and severe refractive errors.
Prevention
Preventing the progression of keratoconus involves early detection through regular eye examinations, especially for individuals over 10 with a family history of the condition. Avoiding excessive eye rubbing, particularly for those with atopic conditions or allergies causing eye itching, is also crucial. A diet rich in collagen, antioxidants, and vitamins A, C, E, and zinc can support eye health.
When to See a Doctor?
Consult an ophthalmologist immediately if your vision suddenly becomes blurry or worsens. Additionally, individuals with keratoconus or a family history of the condition should have regular eye examinations if they begin experiencing symptoms such as eye irritation or blurred vision.
Looking for more information about other diseases? Click here!
- dr Ayu Munawaroh, MKK
WebMD. What is keratoconus? (2020). Available from: https://www.webmd.com/eye-health/eye-health-keratoconus.
MayoClinic. Keratoconus. Available from: https://www.mayoclinic.org/diseases-conditions/keratoconus/symptoms-causes/syc-20351352.
John Hopkins Medicine. Keratoconus. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/keratoconus.
Boyd K, Huffman J. What is keratoconus? (2020). Available from: https://www.aao.org/eye-health/diseases/what-is-keratoconus.