Definition
A lacrimal duct laceration is damage to the tear drainage system caused by sudden physical trauma, either directly or indirectly, which can also affect the eyelid (palpebral laceration). Various types of facial trauma can result in damage to the tear duct system.
Causes
Lacrimal duct lacerations can result from both direct and indirect trauma. Direct trauma, such as injuries caused by glass, coat hangers, knives, dog bites, cat scratches, fingernails, or other sharp objects, can directly impact the lacrimal system. Indirect trauma is caused by blunt forces impacting the area around the eyes, such as blows to the face, blunt weapons, or other blunt objects.
Risk Factor
These injuries are most common in children and young adults. Patients under the age of 4 are particularly susceptible to dog bite injuries on the face. Sharp and blunt weapon injuries, as well as trauma from various objects, tend to occur more frequently in young adults. Gender is also a risk factor, with men more often exposed to lacrimal duct trauma than women. Boys are more likely to experience dog bite wounds on the face than girls, and young men are more often involved in physical altercations than young women.
Environmental factors, such as exposure to certain activities, animals, or objects, can increase the risk of trauma. Occupations involving objects that can enter the eye, like boxing, are common causes of lacrimal duct trauma. In some cases, birth trauma can also be a risk factor for lacrimal duct laceration.
Symptoms
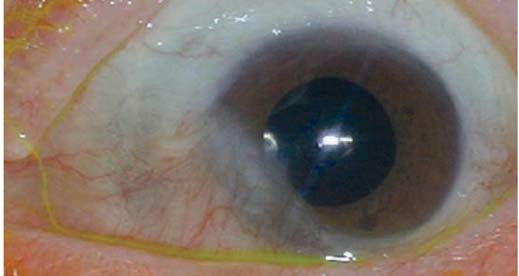
Determining the clinical picture involves understanding the extent of the injury, evaluating potential damage to the eyeball, assessing contamination levels, and considering the risk of foreign objects entering the eyeball. The mechanism of the injury, the trajectory of objects from the wound, and the possibility of intracranial injury should be evaluated. Immediate treatment is crucial for eyeball rupture and other ocular trauma, ideally within 48 hours. Symptoms may include redness in the white part of the eye, bleeding, visible wounds, reduced vision, and a decreased field of view.
Diagnosis
Establishing a diagnosis begins with a thorough interview to understand the mechanism of trauma, whether it was blunt or sharp, the strength of the injury, and the presence of foreign objects (especially common in children). The interview should also consider any head injuries, maxillofacial bone fractures, or orbital fractures.
Comprehensive diagnostic tests are necessary to help finding the diagnosis, including field examination, slit lamp evaluation, and funduscopy to check for eye damage. Children may require general anesthesia for these procedures. If there are penetrating wounds, even if small, careful observation for potential eyeball penetration is required. Assessing the wound on the eyelids is crucial, as it influences the surgical approach. Evaluating the degree of the wound and any missing tissue is also important. Anel test helps determine the patency of the lacrimal duct; a leak in the injected fluid suggests a lacrimal duct laceration.
Other diagnostic examinations, such as ocular X-rays and CT scans, are performed if fractures or foreign objects are suspected. Proper documentation of the wound and damage to both the eyelids and eyeballs is essential.
Management
Repair of lacrimal duct lacerations should be performed promptly, ideally within 48 hours. The treatment approach includes both medication and surgical intervention. Tetanus prophylaxis is recommended if contamination is suspected. For lacerations resulting from dog bites, rabies prevention through active or passive immunization may be necessary. Antibiotics are typically administered following surgery.
Surgical intervention is indicated for cooperative patients. Depending on the severity of the wound and the extent of tissue damage, either local or general anesthesia may be used. General anesthesia is often required for large wounds with extensive tissue damage or involvement of the bone. Surgical techniques vary based on the injury’s extent and the affected structures. The primary goals are to protect the eye, restore its function, and ensure cosmetic outcomes. Reconstruction techniques are often combined to achieve optimal results. The healing process depends on the laceration's area, location, and tissue thickness.
Complications
Potential complications from lacrimal duct lacerations include bacterial conjunctivitis, recurrent corneal abrasion, entropion or ectropion, chronic epiphora (excessive tearing), and keratitis (corneal infection). Poor surgical technique can lead to scarring, fibrosis, eyelid deformities, and issues related to wound healing, such as infections or damage to the nasolacrimal system.
Prevention
Preventing lacrimal duct lacerations involves using eye protection during high-risk activities or work environments, particularly when handling objects prone to causing trauma. Close supervision of young children, especially under the age of 4, is crucial to avoid dog bites or other injuries. Additionally, sharp objects should be kept out of reach of small children.
When to See a Doctor?
Seek immediate medical attention from an eye specialist if experiencing sudden vision changes, redness, pain, excessive tearing, bleeding, foreign objects in the eye, or wounds around the eyes.
Looking for more information about other diseases? Click here!
- dr Ayu Munawaroh, MKK
Canalicular Laceration (Trauma) - EyeWiki [Internet]. Eyewiki.aao.org. 2021
Sadiq MA, Corkin F, Mantagos IS. Eyelid Lacerations Due to Dog Bite in Children. J Pediatr Ophthalmol Strabismus. 2015. 9:1-4
Ho, Thomas, and Vickie Lee. "National survey on the management of lacrimal canalicular injury in the United Kingdom." Clinical & experimental ophthalmology 34.1 (2006): 39-43.
Ann P. Murchison P. A Practical Approach to Canalicular Lacerations. Reviewofophthalmology.com. 2021