Definisi
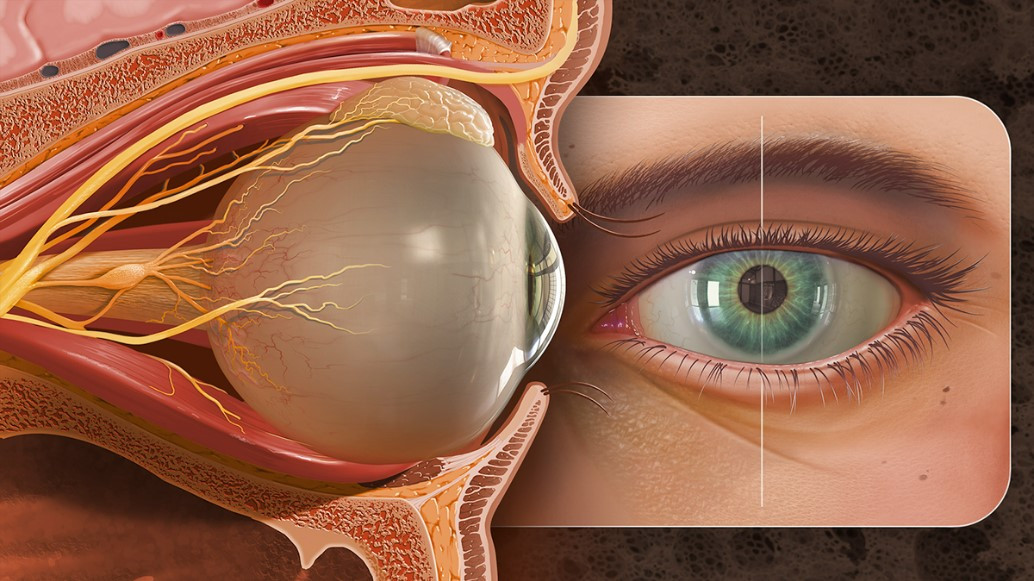
Tumor konjungtiva dalah tumor yang tumbuh di bagian konjungtiva mata. Konjungtiva adalah lapisan yang menempel pada kelopak mata dan bagian depan dari bola mata. Lapisan ini berfungsi untuk mencegah mata kering. Tumor konjungtiva bervariasi dari jinak hingga ganas. Lima tumor konjungtiva yang paling umum adalah Nevus, Ocular Surface Squamous Neoplasia (OSSN), Primary Acquired Melanosis (PAM), melanoma dan limfoma.
Tumor konjungtiva lebih sering ditemukan di Asia bagian Barat dibandingkan dengan Asia Tenggara. Penelitian menunjukkan bahwa pada ras Asia, tumor konjungtiva muncul di usia yang lebih muda dan lebih berisiko untuk bermetastasis dibandingkan dengan ras Kaukasia. Penelitian ini juga menunjukkan bahwa kasus yang ditemukan di Asia Tenggara lebih banyak dialami oleh perempuan dibandingkan laki-laki dengan rasio 3:2.
Penyebab
Tumor Okular Surface Skuamosa (OSSN) merupakan salah satu tumor terbanyak pada mata dengan angka kekambuhan dan kesakitan yang tinggi. Penyebab terbentuknya OSSN adalah paparan sinar matahari yang dapat berasal dari aktivitas diluar seperti berlayar, pekerjaan bangunan ataupun kegiatan beternak. Penyakit penyerta seperti Human Immunodeficiency Virus (HIV) dan Human Papilloma Virus (HPV) dapat menyebabkan seseorang lebih rentan untuk terkena OSSN.
Primary Acquired Melanosis (PAM) dan melanoma berada dalam satu kategori dari tumor konjungtiva, yaitu tumor yang memiliki pigmen. Istilah PAM saat ini digunakan sebagai diagnosis pada kasus melanoma pada mata sebelum ditegakkan diagnosis secara histologi. Hingga saat ini diperkirakan bahwa kasus terjadinya PAM memiliki kaitan yang erat dengan paparan sinar matahari.
Limfoma merupakan kelainan yang ditandai dengan jumlah sel imun yang bertambah. Limfoma dapat terjadi di seluruh tubuh, dimana klasifikasi limfoma pada mata dapat dibagi menjadi limfoma Hodgkin, limfoma non-Hodgkin, limfoma non-Hodgkin sistem saraf pusat, limfoma vitreoretinal primer, dan limfoma uveal. Penyebab utama dari limfoma adalah sistem imun seseorang yang tidak bekerja dengan baik, hal ini dapat disebabkan oleh infeksi ataupun kelainan imun yang diturunkan secara genetik.
Faktor Risiko
Beberapa faktor risiko yang telah diketahui dapat menyebabkan seseorang mengalami tumor konjungtiva dalam hal ini OSSN dan PAM adalah:
- Paparan sinar matahari, terutama paparan sinar UVB.
- Paparan asap rokok.
- Kekurangan vitamin A.
- Cedera pada mata.
- Adanya penyakit penyerta seperti HIV, HPV, Hepatitis B dan Hepatitis C.
Pada kasus limfoma, seseorang akan lebih berisiko mengalami limfoma pada mata jika:
- Memiliki penyakit autoimun, seperti rheumatoid arthritis.
- Memiliki kelainan atau penyakit lain yang menganggu sistem imun.
- Mengalami Acquired Immunodeficiency Syndrome (AIDS).
- Sedang dalam pengobatan yang menekan imun atau imunosupresan seperti pengobatan setelah melakukan transplantasi organ.
Gejala
Pada pasien dengan OSSN, gejala pada mata yang dapat ditemui adalah adanya benjolan di bagian permukaan mata berbentuk bulat dengan adanya pembuluh darah di sekitar. Namun, seringkali gejala tidak dirasakan oleh pasien pada tahap awal. Lokasi timbulnya benjolan atau massa adalah pada lokasi yang sering terkena sinar matahari yaitu pada bagian tepi mata yang dekat dengan hidung atau pada tepi luar. Benjolan jarang menjalar ke bagian lain di luar bola mata.
Pada pasien dengan PAM, ditemukan adanya daerah yang tampak berpigmen atau berwarna lebih gelap dibandingkan dengan daerah disekitarnya, bisa ditemukan pada satu atau kedua mata. Usia rata-rata ditemukannya PAM adalah 56 tahun. Gejala lain yang dapat dirasakan oleh pasien adalah terdapat sensasi seperti terdapat debu halus atau benda melayang pada lapang pandang (floaters). Kelainan ini dapat bervariasi dalam berbagai ukuran hingga dapat menggeser bagian pupil.
Pada pasien yang mengalami limfoma mata, gejala yang dapat dirasakan adalah tampak debu halus atau benda melayang pada lapang pandang (floaters), gangguan pada penglihatan, mata merah dan penglihatan ganda. Jika tumor mengenai bagian sistem saraf pusat, dapat muncul gejala seperti nyeri kepala, mual, kelemahan pada salah satu bagian badan hingga kejang.
Diagnosis
Pada pasien dengan OSSN, diagnosis dibuat dengan beberapa pemeriksaan:
- Pewarnaan luka menggunakan fluorescein, lisamine green atau rose bengal untuk menilai besar dan luas luka.
- Pemeriksaan menggunakan slit lamp untuk melihat permukaan bola mata dengan lebih dekat dan jelas.
- Optical Coherence Tomography (OCT): Merupakan pemeriksaan non-invasif yang digunakan untuk melihat bagian dari retina secara jelas. Dari pemeriksaan ini dapat dinilai ketebalan retina pada setiap lapisan dan digunakan untuk menilai keadaan ataupun kelainan yang ada pada retina.
- Mikroskop konfokal: Adalah mikroskop yang menggunakan teknologi laser untuk membentuk gambaran tiga dimensi dari sampel yang akan dilihat. Dengan menggunakan mikroskop ini dokter akan mendapatkan gambaran yang lebih jelas dan dapat membantu dalam pemilihan pengobatan.
- Ultrasonografi Frekuensi Tinggi: Pemeriksaan ini digunakan untuk mengetahui seberapa luas kerusakan yang terbentuk oleh tumor.
Pada pasien dengan PAM, terdapat beberapa pemeriksaan yang dapat dilakukan untuk membantu diagnosis, antara lain:
- Analisis immunohistokimia: Analsis ini dilakukan dengan teknik biopsi. Biopsi adalah teknik pemeriksaan dengan mengambil jaringan dalam jumlah yang kecil pada daerah yang dicurigai tumor atau memiliki kelainan. Jaringan yang telah diambil akan diperiksa dibawah mikroskop.
- Pemeriksaan fisik. Pada kasus PAM, penting untuk menilai keterlibatan kelopak mata. Hal ini dilakukan dengan melipat kelopak mata dan memeriksa permukaan kelopak bagian dalam atau dinamakan dengan eversi kelopak mata. Jika ditemukan permukaan yang berbentuk benjolan, maka diagnosis akan mengarah ke melanoma.
Pada pasien dengan limfoma, pemeriksaan yang dapat dilakukan adalah:
- Optical Coherence Tomography (OCT): Merupakan pemeriksaan yang dilakukan untuk memeriksa bagian retina.
- Ultrasonografi (USG): Pemeriksaan ini dilakukan untuk melihat luka yang terletak di belakang retina, derajat pelepasan retina dan menilai penebalan dari saraf mata.
- Sitologi: Pemeriksaan sitologi dilakukan dengan cara memeriksa jaringan yang diambil dari lapisan vitreus atau retina.
- Imunohistokimia: Pemeriksaan menggunakan zat pewarna kimia yang diberikan pada jaringan limfoma.
- Magnetic Resonance Imaging (MRI): Merupakan pemeriksaan yang dilakukan untuk memberikan gambaran yang lebih detail terhadap jaringan lunak pada mata dan sekitarnya.
Tata Laksana
Sebelum terapi dan pengobatan dimulai, dokter akan menanyakan beberapa hal, diantaranya kapan dimulainya gejala, apakah luka cendrung berulang dan terapi yang telah didapat sebelumnya. Pada beberapa pasien dapat diberikan pengobatan topikal menggunakan obat yang mengandung Interferon-alfa2b, mitomycin C dan fluorouracil.
Pada pasien yang dicurigai mengalami PAM, biopsi selalu dilakukan untuk mengetahui jenis dan derajat keparahan tumor. Teknik pengambilan bisa menggunakan biopsi eksisi dan biopsi insisi. Selain biopsi, tindakan yang dapat dilakukan adalah krioterapi untuk bagian yang dicurigai mengalami PAM. Jika PAM sudah mencapai jaringan kornea maka diberikan terapi tambahan menggunakan mitomycin C dan pengangkatan jaringan menggunakan bantuan alkohol. Semua tindakan yang dilakukan harus dengan pengawasan dan atas saran dokter.
Pada kasus limfoma, pengobatan yang dapat dilakukan adalah kemoterapi dan radioterapi. Kemoterapi dilakukan dengan cara menyuntikkan atau memberikan obat secara langsung pada mata yang terkena limfoma. Terapi radiasi menggunakan energi radiasi yang tinggi untuk menghancurkan sel limfoma sesuai dengan lokasi dimana tumor berada. Terapi limfoma pada setiap orang berbeda, tergantung dari tingkat keparahan dan keadaan pada saat didiagnosa. Konsultasikan terapi yang akan Anda pilih dengan dokter.
Komplikasi
Komplikasi yang paling umum terjadi pada pasien dengan tumor konjungtiva adalah kasus yang berulang. Dari setengah kasus tumor konjungtiva yang ada dapat mengalami kasus yang sama dalam beberapa tahun kedepan. Kasus yang berulang cenderung memiliki karakteristik yang lebih ganas dibandingkan dengan kasus awal. Komplikasi lain yang dapat dialami adalah gangguan atau kehilangan penglihatan pada satu atau kedua mata. Lapang pandang bagian tepi juga dapat terganggu. Glaukoma atau peningkatan tekanan pada bola mata juga dapat terjadi akibat dari pertumbuhan tumor di konjungtiva. Pada kasus tumor yang lebih lanjut, tumor dapat menyebar ke bagian lain selain mata seperti tulang, paru-paru atau hati.
Limfoma pada mata dapat menyebabkan gangguan pada sistem saraf pusat seperti kejang dan kelemahan tubuh. Massa yang menyebar hingga sistem saraf pusat juga dapat memberikan gangguan pada lapang pandang.
Pencegahan
Dalam mencegah terjadinya tumor pada konjungtiva mata, beberapa hal yang dapat dilakukan adalah:
- Cegah terjadinya cedera pada mata dengan menggunakan pelindung mata saat berkendara dengan sepeda motor atau bekerja dengan benda-benda yang berpotensi dapat melukai mata.
- Gunakan kacamata hitam dapat menangkal sinar UV, terutama saat Anda melakukan aktivitas atau bekerja di luar ruangan.
- Berhenti merokok.
Kapan Harus ke Dokter?
Beberapa tanda bahaya yang harus diperhatikan jika Anda mengalami keluhan pada mata atau curiga mengalami tumor pada konjungtiva adalah:
- Terdapat gangguan penglihatan pada satu atau kedua mata.
- Gangguan pada sistem saraf pusat seperti nyeri kepala, muntah, kejang dan kelemahan pada salah satu bagian tubuh.
- Nyeri pada satu atau kedua mata yang disertai dengan nyeri kepala dan muntah.
- Benjolan atau bintik yang berwarna lebih gelap disertai dengan penambahan ukuran atau menyebabkan keluhan lain seperti kemerahan pada mata.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Nadia Opmalina
Shields, C., Chien, J., Surakiatchanukul, T., Sioufi, K., & Lally, S. (2017). Conjunctival Tumors: Review of Clinical Features, Risks, Biomarkers, and Outcomes—The 2017 J. Donald M. Gass Lecture. Asia-Pacific Journal Of Ophthalmology. https://doi.org/10.22608/apo.201710
Boyd, K. (2021). What Is Eye Lymphoma?. American Academy of Ophthalmology. Optical Coherence Tomography | Department of Ophthalmology. Ophthalmology.med.ubc.ca. (2021). Chang, V., Bunya, V., & Gurnani, B. (2021). Ocular Surface Squamous Neoplasia - EyeWiki. Eyewiki.aao.org.
Tan, L., Hong, J., Goh, W., Chang, E., Yang, V., & Poon, E. et al. (2020). Clinical features and survival outcomes of ocular melanoma in a multi-ethnic Asian cohort. Scientific Reports, 10(1). https://doi.org/10.1038/s41598-020-73534-x
Kanski, J. J. (2020). Clinical diagnosis in ophthalmology. Elsevier Mosby.
Eye melanoma - Symptoms and causes. Mayo Clinic. (2021).
Can Eye Cancer Be Prevented?. Cancer.org. (2021).