Definisi
Luka pascaoperasi merupakan luka sayatan pada kulit yang dibentuk oleh pisau bedah saat melakukan pembedahan. Luka pascaoperasi dapat terinfeksi apabila tidak dirawat dengan baik. Luka pascaoperasi yang terinfeksi dapat menyebabkan masalah hingga kematian. Infeksi luka pascaoperasi juga termasuk di dalam infeksi akibat pelayanan di rumah sakit.
Penyebab
Infeksi luka pascaoperasi disebabkan oleh bakteri. Bakteri yang paling sering menjadi penyebab infeksi adalah Staphylococcus, Streptococcus, dan Pseudomonas. Bakteri dapat menginfeksi luka pascaoperasi akibat kontak yang bermacam-macam, misalnya kontak dengan tangan pengurus pasien (caregiver) yang kotor, kontak dengan alat-alat bedah, bakteri di udara, atau bakteri yang sudah ada pada tubuh dan menyebar ke luka tersebut.
Luka pascaoperasi terbagi atas empat kategori berdasarkan kebersihan luka, risiko infeksi, dan lokasi luka, yaitu:
- Kelas I: Luka pascaoperasi ini merupakan luka bersih. Luka ini tidak menunjukkan tanda-tanda infeksi maupun peradangan. Luka ini dapat melibatkan mata, kulit, dan sistem peredaran darah
- Kelas II: Luka pascaoperasi ini bersih-terkontaminasi. Meskipun luka tidak menunjukkan tanda-tanda infeksi, namun risiko infeksinya tinggi karena lokasinya. Misalnya, luka pascaoperasi pada saluran pencernaan sangat rentan terinfeksi
- Kelas III: Luka pascaoperasi ini sudah mengalami kontak dengan benda luar, sehingga memiliki risiko sangat tinggi untuk terinfeksi, dan sudah dianggap terkontaminasi. Misalnya, luka tembak dapat mengotori kulit sekitar tempat pembedahan
- Kelas IV: Luka pascaoperasi ini dianggap kotor-terkontaminasi. Luka yang sudah terpapar tinja termasuk dalam golongan ini
Faktor Risiko
Faktor risiko infeksi luka pascaoperasi terbagi atas faktor pasien dan faktor terkait prosedur. Faktor risiko pasien mengalami infeksi luka pascaoperasi adalah usia tua, gizi buruk, volume darah yang kurang (hipovolemia), obesitas, penggunaan obat steroid, diabetes, penggunaan obat yang menurunkan kekebalan tubuh, merokok, dan adanya infeksi di bagian tubuh lainnya.
Sementara itu, faktor risiko infeksi luka pascaoperasi terkait prosedur adalah sebagai berikut:
- Adanya darah yang mengumpul di dekat tempat pembedahan (hematoma)
- Penggunaan alat seperti drain (yang berfungsi untuk mengalirkan cairan keluar)
- Penyisaan ruang kosong akibat kehilangan jaringan
- Lama cuci tangan (scrub) sebelum pembedahan
- Pencukuran rambut pasien sebelum pembedahan
- Pembedahan yang dilaksanakan lama
- Kontaminasi ruang operasi
- Rawat inap di rumah sakit yang terlalu lama
Gejala
Setiap luka yang terinfeksi akan menimbulkan gejala seperti merah, sulit sembuh, demam, nyeri, hangat, dan bengkak. Suatu luka yang terinfeksi dapat dikategorikan sebagai infeksi luka pascaoperasi jika memenuhi kriteria berikut:
- Terjadi dalam 30 hari pascaoperasi (pada pembedahan yang melibatkan benda yang dimasukkan ke dalam tubuh, infeksi dapat terjadi hingga 1 tahun pascaoperasi)
- Hanya melibatkan kulit, jaringan di bawah kulit, jaringan ikat dalam, jaringan ikat dalam, atau organ yang jauh
- Keluar nanah atau ada kuman yang ditemukan dan diisolasi dari luka
Klasifikasi infeksi luka pascaoperasi adalah sebagai berikut:
- Superfisial insisional. Infeksi tipe ini menghasilkan nanah dari luka pascaoperasi. Nanah ini kemudian dapat diambil dan dikultur untuk mengetahui kuman penyebab infeksi
- Insisional dalam. Infeksi tipe ini juga dapat menghasilkan nanah. Luka juga dapat terbuka sendirinya, atau dokter bedah dapat membuka luka kembali dan menemukan nanah
- Infeksi organ/ruang. Infeksi tipe ini dapat menghasilkan nanah dari drain yang mengalirkan cairan dari organ/ruang keluar kulit. Nanah ini dapat berkumpul di suatu ruang yang dikelilingi jaringan mati atau terinfeksi, yang disebut sebagai abses
Diagnosis
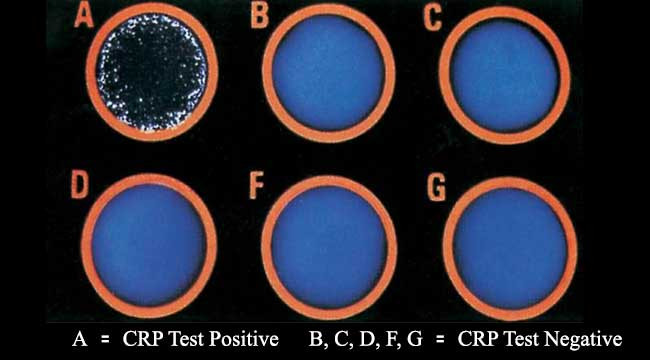
Diagnosis infeksi luka pascaoperasi ditegakkan melalui keluhan, riwayat, dan pemeriksaan. Dokter biasanya juga akan mengambil sebagian nanah untuk dikirim ke laboratorium dan dikultur. Kultur merupakan pengembangbiakkan kuman di wadah tertutup untuk mengetahui penyebab infeksi dan keampuhan antibiotik dalam melawan kuman tersebut. Jika infeksi cukup dalam, dokter dapat melakukan pencitraan seperti ultrasonografi (pemeriksaan dengan gelombang suara), computed tomography scan (CT scan), atau magnetic resonance imaging (MRI).
Tata Laksana
Sebagian besar infeksi luka pascaoperasi dapat ditangani dengan antibiotik. Namun, dokter dapat memutuskan untuk melakukan pembedahan atau prosedur tambahan apabila diperlukan. Pembedahan atau prosedur tambahan ini dapat berupa debridement, yaitu membuka kembali luka pascaoperasi untuk membersihkannya di ruang operasi. Selain itu, apabila pembedahan mengharuskan adanya benda yang ditinggalkan di dalam tubuh (implan, logam, dan sebagainya), dokter akan mempertimbangkan untuk mengambil kembali benda tersebut, karena bakteri dapat membentuk koloni pada benda tersebut. Namun, pertimbangan dokter ini akan melibatkan pertimbangan mengenai keuntungan dan kerugian bagi Anda sebagai pasien.
Komplikasi
Komplikasi infeksi luka pascaoperasi terbagi atas komplikasi lokal dan sistemik (seluruh tubuh). Komplikasi lokal dapat berupa waktu penyembuhan luka yang lebih lama, luka yang tidak sembuh, selulitis, pembentukan abses, osteomielitis, serta luka terbuka kembali. Sementara itu, komplikasi yang melibatkan seluruh tubuh atau sistemik dapat berupa adanya bakteri di dalam darah (bakteremia), kemungkinan menyebarnya infeksi ke organ yang jauh, dan sepsis (reaksi kekebalan tubuh yang berlebih akibat infeksi).
Pencegahan
Pencegahan infeksi luka pascaoperasi dapat dilakukan sebelum dan sesudah pembedahan. Sebelum pembedahan, Anda dapat melakukan hal sebagai berikut:
- Mandi dengan pembersih antiseptik yang diberikan dokter sebelum pembedahan
- Jangan mencukur, karena pencukuran dapat mengiritasi kulit dan menyebabkan infeksi pada kulit
- Berhenti merokok sebelum pembedahan, karena perokok memiliki risiko yang lebih tinggi untuk mengalami infeksi luka pascaoperasi. Berhenti merokok memang sangat sulit, namun dapat dilakukan. Anda dapat berkonsultasi kepada dokter terkait rencana berhenti merokok
Setelah pembedahan selesai, Anda dan keluarga dapat melakukan hal sebagai berikut:
- Menjaga penutup luka steril yang dipasang dokter bedah hingga 48 jam
- Mengonsumsi antibiotik pencegahan, jika diresepkan
- Memastikan Anda dan keluarga mengerti cara merawat luka. Anda dapat bertanya kepada dokter atau perawat terkait cara merawat luka yang benar
- Selalu mencuci tangan dengan sabun dan air mengalir sebelum menyentuh luka dan memastikan orang yang mengurus Anda juga melakukan hal tersebut
- Aktif selama perawatan di rumah sakit, misalnya dengan memerhatikan seberapa sering penutup luka diganti, pembersihan dan sterilisasi ruangan, dan apabila orang yang mengurus Anda telah mencuci tangan dan menggunakan sarung tangan bersih ketika menangani luka Anda
Kapan Harus ke Dokter?
Anda perlu ke IGD terdekat apabila Anda menemukan tanda atau gejala infeksi. Tanda dan gejala infeksi luka pascaoperasi dapat berupa:
- Nyeri yang semakin parah
- Merah atau bengkak
- Darah atau nanah yang mengalir
- Cairan yang keluar dari luka bertambah (dapat pula semakin tebal, coklat, hijau, atau kuning)
- Bau tidak sedap
- Luka tampak lebih besar, lebih dalam, terlalu kering, atau tampak gelap
- Demam lebih dari 37,5 derajat Celsius selama lebih dari 4 jam
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Anita Larasati Priyono
Surgical Site Infections. (2022). Retrieved 20 May 2022, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/surgical-site-infections
Watson, K. (2018). Signs of Infection After Surgery. Retrieved 20 May 2022, from https://www.healthline.com/health/signs-of-infection-after-surgery
Zabaglo, M., & Sharman, T. (2021). Postoperative Wound Infection. Retrieved 20 May 2022, from https://www.ncbi.nlm.nih.gov/books/NBK560533/