Definition
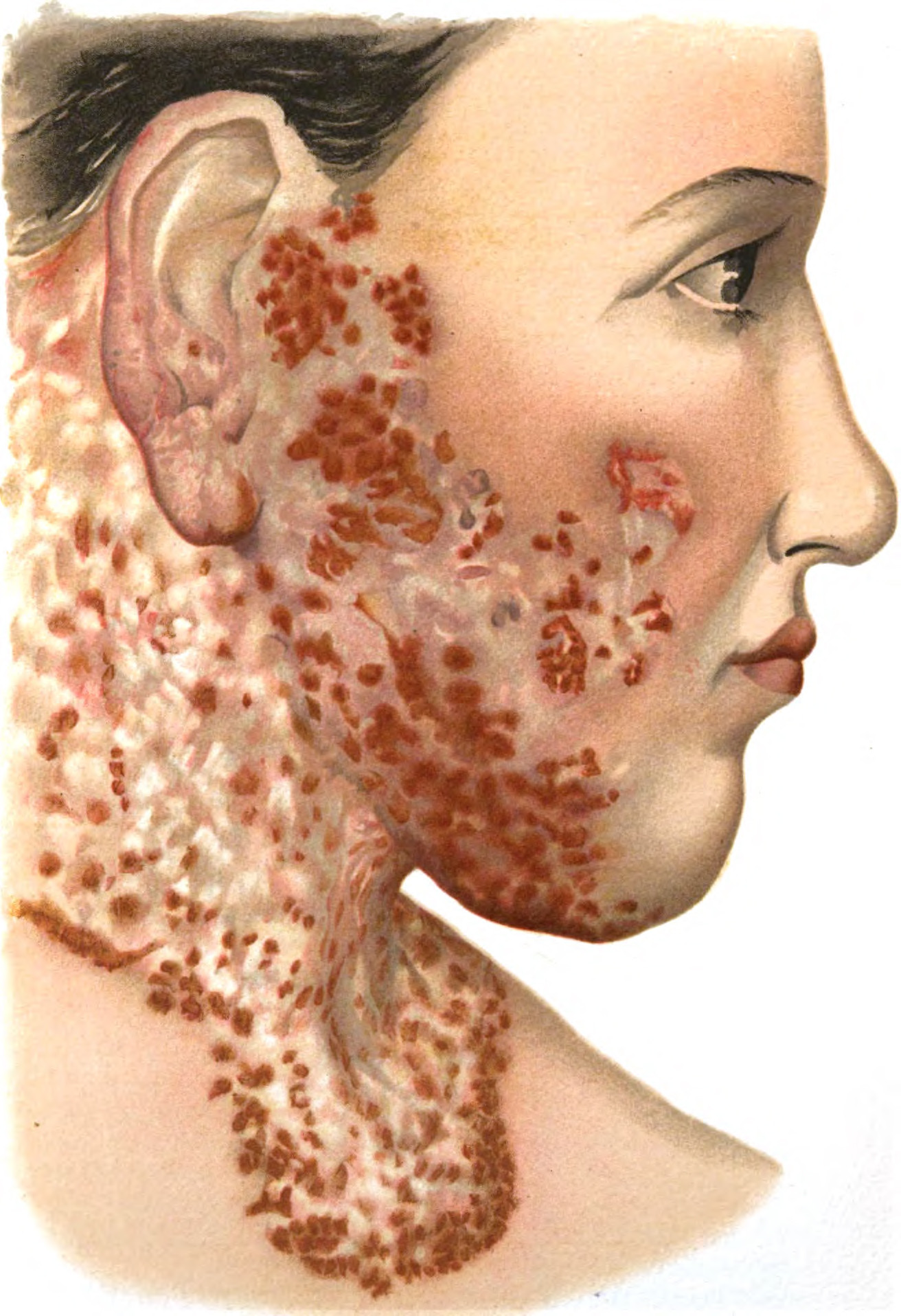
Scleroderma refers to a group of rare diseases that cause thickening or hardening of the skin. The term "scleroderma" is derived from the Greek word "sclero," which means hard, and the Latin word "derma," which means skin. The manifestations of this disease can vary widely among individuals. Scleroderma is neither contagious nor malignant. While the disease primarily affects the skin, it can also cause complications in the blood vessels, internal organs, and digestive system.
Scleroderma is classified as an autoimmune disorder, in which the immune system mistakenly attacks the body's tissues. The disease is relatively uncommon, with an estimated 75,000 to 100,000 people affected in the United States, most of whom are women between the ages of 30 and 50.
Causes
Scleroderma arises from the overproduction and buildup of collagen in the body's tissues. Collagen is a protein that forms the connective tissues, including the skin. The exact cause of scleroderma is not fully understood, but it is believed to involve a combination of factors such as immune system dysfunction, genetic predisposition, and environmental triggers. Ongoing research aims to clarify the relationship between scleroderma and the immune system.
Risk Factor
While anyone can develop scleroderma, it is more common in women than in men, with a 4:1 ratio. The condition typically manifests between the ages of 25 and 55, although it can affect individuals of any age, from children to the elderly. Several factors may increase the likelihood of developing scleroderma, including:
Genetic factors
Although most individuals with scleroderma do not have relatives or children who also suffer from the disease, some familial cases exist. Research has identified gene variations that may raise the risk of scleroderma, though genetics alone do not cause the condition.
Environmental factors
Evidence suggests that scleroderma may be triggered in some individuals by exposure to certain viruses or medications. Repeated exposure to harmful chemicals, such as those found in factory environments, may also elevate the risk. However, not everyone with environmental exposure develops the disease.
Immune system disorders
Scleroderma is considered an autoimmune disease, wherein the body's immune system attacks healthy connective tissue. Individuals with scleroderma may also have other autoimmune diseases, such as rheumatoid arthritis or lupus.
Symptoms
Scleroderma is a chronic condition affecting connective tissue, with symptoms that vary significantly between individuals, ranging from mild to potentially life-threatening. Symptoms can be evident if the skin is involved but may be more subtle when internal organs are affected. Scleroderma can present in various parts of the body, including the eyes, mouth, hands, joints, kidneys, heart, lungs, brain, or digestive system.
Symptoms depend on the affected organ or tissue and may include:
- Thickening and swelling of the skin
- Finger swelling, particularly noticeable upon waking, often an early symptom
- Tightness of the facial skin
- Difficulty in moving the lips and mouth
- Sjögren's syndrome (experienced by 20% of scleroderma patients), causing dry mouth and eyes, difficulty speaking and swallowing, and reduced taste
- Raynaud's phenomenon, characterized by abnormal narrowing of small blood vessels in the fingers and toes, leading to pale, bluish, or red fingers, numbness, or pain
- Joint warmth, pain, or swelling
- Muscle weakness or pain
- Heartburn or a burning sensation in the chest
- Diarrhea or constipation
- Swallowing difficulty
- Shortness of breath and persistent coughing
- High blood pressure, headaches, vision issues, chest pain, and other symptoms
Diagnosis
Diagnosing scleroderma can be challenging due to its wide range of symptoms and the different organs it may affect. After a physical examination, a doctor may recommend additional tests if symptoms suggest a more complex condition requiring further investigation.
A blood test is typically conducted to check for the presence of autoantibodies, proteins created by the immune system that attack healthy tissues. The diagnostic process often involves consultation with specialists such as rheumatologists or dermatologists, depending on the organs affected.
Additional tests may help to:
- Confirm the diagnosis
- Assess the risk of complications
- Monitor inflammation and autoantibody levels
- Track disease progression and determine the extent of organ damage
Management
At present, there is no definitive cure for scleroderma. While numerous therapies are available to manage symptoms, no drug has been proven to halt or reverse the disease. Treatment focuses on addressing the symptoms that appear, preventing complications, and enhancing the patient’s quality of life. In some cases of mild symptoms, therapy may not be necessary, or it may be discontinued when the disease becomes inactive. Some treatments also aim to suppress the immune system’s activity.
The selection of drugs varies based on the part of the body affected. Typically, medications are prescribed to:
- Dilate blood vessels to alleviate symptoms of Raynaud’s phenomenon.
- Suppress the immune system to slow the progression of scleroderma, such as skin thickening or lung damage.
- Manage digestive symptoms, including drugs to reduce stomach acid as well as medications and antibiotics to aid digestion and relieve bloating, diarrhea, and constipation.
- Prevent infections, particularly in the lungs, which are vulnerable due to scleroderma.
- Relieve pain.
In addition to medication, physical therapy or rehabilitation can improve strength and mobility, enabling patients to remain as active as possible. For severe cases that do not respond to standard treatment, stem cell transplantation may be an option. In cases of significant lung or kidney damage, organ transplantation can be considered.
Complications
Scleroderma can lead to a range of complications, from mild to severe, affecting various parts of the body:
1. Fingers
Raynaud’s phenomenon may become so severe that blood flow is blocked, leading to permanent tissue damage and skin ulcers. In extreme cases, the tissue in the fingertips may die.
2. Lungs
Lung damage can impair breathing and reduce physical mobility. Pulmonary hypertension may also develop.
3. Kidney
Serious kidney complications may arise, marked by a sudden rise in blood pressure and rapid kidney failure. Immediate treatment is necessary to preserve kidney function.
4. Heart
Thickening of heart tissue can result in arrhythmias and heart failure. Scleroderma may also cause inflammation of the membrane surrounding the heart.
5. Teeth
Severe thickening of the facial skin can narrow the mouth, making it difficult to clean teeth. Additionally, many individuals with scleroderma suffer from reduced saliva production, increasing the risk of tooth decay.
6. Digestive Tract
Digestive issues linked to scleroderma may include heartburn, difficulty swallowing, stomach cramps, bloating, constipation, or diarrhea. Some people may also experience nutrient absorption issues due to abnormal bacterial growth in the intestines.
7. Joints
The skin over the joints can thicken, restricting movement, particularly in the hands.
Prevention
Since the exact cause of scleroderma is unknown, there is no specific way to prevent the disease. Scleroderma may be triggered by a combination of genetic, environmental, and immune system factors. If a family member has scleroderma, genetic screening might be beneficial. Avoiding exposure to harmful chemicals and using personal protective equipment in certain workplaces can also reduce the risk.
When to See a Doctor?
If you develop symptoms of scleroderma, it is important to consult a doctor for early and appropriate treatment.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Scleroderma - Diagnosis and treatment - Mayo Clinic. Mayoclinic.org. (2022). Retrieved 19 May 2022, from https://www.mayoclinic.org/diseases-conditions/scleroderma/diagnosis-treatment/drc-20351957.
Scleroderma. Rheumatology.org. (2022). Retrieved 19 May 2022, from https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Scleroderma.
Understanding Scleroderma - National Scleroderma Foundation. National Scleroderma Foundation. (2022). Retrieved 19 May 2022, from https://scleroderma.org/understanding-scleroderma/.