Definition
Chronic Lymphocytic Leukemia (CLL) is a type of blood cancer and the most common form in adults. It occurs when healthy white blood cells (lymphocytes) in the bone marrow mutate or change into cancer cells that replicate and disrupt the production of healthy platelets or thrombocytes.
CLL typically affects people aged 65 and older but can also occur in individuals as young as 30 years old. It is possible to have CLL without experiencing symptoms, and many people only discover they have it through blood tests as part of routine physical examinations.
At present, healthcare providers do not have standard treatments to cure chronic lymphocytic leukemia. However, over the past decade, treatments have been developed to induce remission in CLL, meaning patients experience no symptoms or signs of the disease. These treatments have significantly extended the lifespan of CLL patients.
CLL can develop in both types of lymphocytes:
- B lymphocytes (B cells), which produce antibodies targeting viruses, bacteria, and cancer cells.
- T lymphocytes (T cells), which regulate the body's immune system response and directly attack abnormal cells, including cancer cells.
Nearly all people with CLL have the B-cell form of chronic lymphocytic leukemia. There is a related condition affecting T cells called T-cell prolymphocytic leukemia (T-PLL), which progresses more rapidly than B-cell CLL.
Chronic lymphocytic leukemia ranks among the most common types of leukemia in adults. For example, it affects approximately 5 out of every 100,000 people in the United States. The American Cancer Society estimates that around 18,700 people will be diagnosed with CLL in 2023. By comparison, over 238,000 people will receive a lung cancer diagnosis in 2023, making it one of the most common cancers overall.
Causes
The exact causes of chronic lymphocytic leukemia (CLL) remain uncertain. However, certain factors are known to lead to mutations in the DNA of blood-producing cells. These cells contain instructions that govern their behavior, and the mutations trigger signals that cause blood cells to produce abnormal and ineffective lymphocytes.
In addition to their ineffectiveness, these abnormal lymphocytes have a prolonged lifespan and continue to multiply, unlike healthy lymphocytes that would naturally die. Consequently, they accumulate in the blood and specific organs, resulting in complications. They may overcrowd healthy cells in the bone marrow, disrupting the production of blood cells.
Doctors and researchers are actively engaged in unraveling the precise mechanisms underlying chronic lymphocytic leukemia.
Risk factor
Several risk factors contribute to the development of CLL, including:
- Family history: Research suggests that individuals with close relatives such as parents, siblings, or children diagnosed with CLL are two to four times more likely to develop the condition.
- Age: The average age at diagnosis is 71 years old.
- Gender: Men are at a higher risk of developing CLL compared to women.
- Exposure to Agent Orange: Studies have indicated a correlation between CLL and exposure to Agent Orange, a chemical utilized during the Vietnam War.
- Monoclonal B-cell lymphocytosis: This condition involves a higher-than-normal number of identical B cells in the blood. Individuals with monoclonal B-cell lymphocytosis have a slight risk of developing CLL.
Symptoms
You can suffer from chronic lympho-symptomatic symptoms. It may take months to years before you realize the symptoms of LLK. Common symptoms include:
- LLK affects red blood cells, causing anemia. Fatigue is a common symptom of anemia
- Fever is a sign of infection. LLK affects healthy white blood cells, increasing the risk of infection
- Swelling of lymph nodes in the neck, armpits, groin or stomach
- Night sweat
- Unexplainable weight loss
- Pain or fullness under the ribs. LLK can affect the liver or runoff
Diagnosis
CLL diagnosis involves a medical interview, physical examination, and diagnostic tests. The doctor may inquire about the patient's primary complaints, accompanying symptoms, medical history, family medical history, medications, and daily activities to diagnose CLL.
During the physical examination, vital signs are checked, including blood pressure, body temperature, respiratory rate, and pulse. Following this, a comprehensive head-to-toe examination is conducted to assess internal organs.
Diagnostic tests for CLL may include:
- Complete blood count with differential: This test measures the levels of red blood cells, white blood cells, and platelets in the blood. It also evaluates the amount of hemoglobin present in red blood cells.
- Peripheral blood smear: A pathologist examines blood cells under a microscope to identify any cancerous blood cells.
- Flow cytometry: This laboratory test provides detailed information about blood cells. In CLL diagnosis, flow cytometry is used to detect the presence of CLL cells in white blood cells.
- Genetic testing: Tests such as fluorescent in situ hybridization (FISH) and immunoglobulin heavy chain (IGHV) analysis are employed to study chromosomes and genes. Understanding genetic mutations aids in determining appropriate CLL therapy.
Management
Treatment options for chronic lymphocytic leukemia (CLL) are determined by various factors, including the cancer stage, experienced signs and symptoms, overall health history, and preferred therapy options.
If CLL is asymptomatic and not progressing, immediate treatment may not be necessary. Studies have indicated that early treatment does not extend the lifespan of individuals with early-stage CLL.
Some treatment options for chronic lymphocytic leukemia (CLL) include:
- Chemotherapy : utilizes drugs to target and kill rapidly dividing cells, including cancer cells. Chemotherapy can be administered intravenously or taken orally in pill form.
- Targeted therapy: Targeted drug therapy focuses on specific abnormalities in cancer cells. By blocking these abnormalities, targeted therapy can induce cancer cell death.
- Immunotherapy: Immunotherapy harnesses the body's immune system to combat cancer. Cancer cells often evade immune system detection by producing proteins that inhibit immune response. Immunotherapy disrupts this process, enabling the immune system to recognize and attack cancer cells.
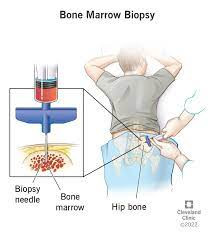
- Bone marrow transplantation (Stem cell transplantation): This procedure involves high-dose chemotherapy to eradicate abnormal stem cells in the bone marrow, followed by the infusion of healthy adult stem cells from a donor. These transplanted stem cells travel to the bone marrow, regenerating healthy blood cells.
As new and more effective drug combinations have emerged, the use of bone marrow transplantation in treating chronic lymphocytic leukemia has declined. However, in specific circumstances, it remains a viable treatment option.
Moreover, supportive care plays a crucial role in CLL management. Regular consultations with healthcare providers facilitate monitoring potential complications and the implementation of measures to prevent or alleviate signs and symptoms.
Supportive care measures may encompass:
- Cancer screening protocols
- Vaccination strategies aimed at preventing infections
- Ongoing monitoring for any additional health concerns
Complications
Chronic lymphocytic leukemia impacts red blood cells, white blood cells, and platelets, each serving crucial bodily functions. Red blood cells transport oxygen, white blood cells defend against infections, and platelets aid blood clotting.
In the absence of healthy blood cells and platelets, individuals with CLL may encounter the following complications:
- Lymphoma: Approximately 2% to 10% of CLL patients develop lymphoma.
- Increased risk of other cancers: CLL compromises the immune system's ability to combat cancer cells, elevating the risk of skin, lung, or colorectal cancer.
- Anemia: Insufficient red blood cells can lead to oxygen deficiency.
- Thrombocytopenia: CLL can diminish the platelet count, impairing the blood clotting process.
- Heightened susceptibility to infections: Inadequate levels of healthy white blood cells increase vulnerability to bacterial, fungal, or viral infections.
- Autoimmune diseases: Some individuals with CLL may experience autoimmune hemolytic anemia, where the immune system attacks its red blood cells.
Prevention
Currently, no specific methods exist to prevent chronic lymphocytic leukemia (CLL).
When to see a doctor?
Visit a doctor if you experience any of the symptoms of CLL listed above.
Looking for more information about other diseases? Click here!
- dr. Monica Salim
Cleveland Clinic - Chronic Lymphocytic Leukemia (2023). Retrieved 4 April 2023, from https://my.clevelandclinic.org/health/diseases/6210-chronic-lymphocytic-leukemia
Mayo Clinic - Chronic Lymphocytic Leukemia (2021). Retrieved 4 April 2023, from https://www.mayoclinic.org/diseases-conditions/chronic-lymphocytic-leukemia/diagnosis-treatment/drc-20352433
Medscape - Chronic Lymphocytic LEukemia (2023) Retrieved 4 April 2023, from https://www.mayoclinic.org/diseases-conditions/chronic-lymphocytic-leukemia/diagnosis-treatment/drc-20352433