Definition
Juvenile Idiopathic Arthritis (JIA), previously referred to as juvenile rheumatoid arthritis, is the most common type of arthritis in children under the age of 16.
Causes
JIA occurs when the immune system attacks its own tissue and cells. The exact cause is not fully understood, but both hereditary and environmental factors appear to play a role.
Risk factor
According to the definition, JIA occurs in children and adolescents under the age of 16. Most types of JIA are more common in girls. JIA can affect individuals of any race and ethnicity.
While JIA is rarely seen in more than one family member, children with a family history of chronic arthritis, including JIA, have a slightly increased risk of developing the condition. Additionally, a family history of psoriasis is a risk factor for the occurrence of psoriatic JIA.
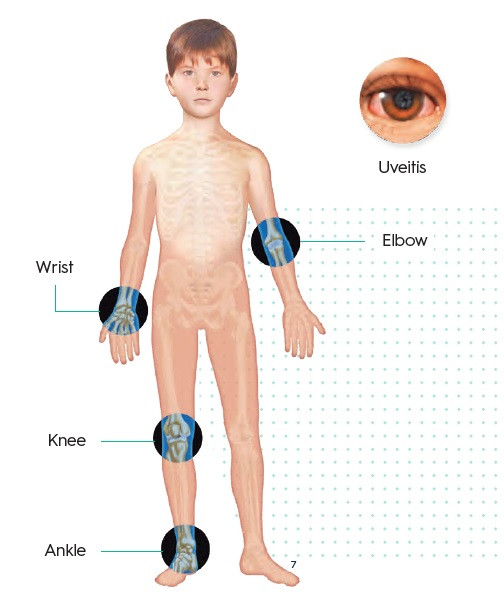
Symptoms
The signs and symptoms of JIA that commonly occur include:
- Pain: Your child may exhibit joint pain, although they may not verbalize it. They might walk with a limp, especially in the morning or after waking from a nap.
- Swelling: Joint swelling, typically affecting large joints like the knees, is common.
- Stiffness: Your child may appear clumsier, particularly in the morning or after a nap.
- Fever, swollen lymph nodes, and rash: Some cases of JIA may present with high fever, swollen lymph nodes, or a rash on the trunk, often worsening at night.
JIA can affect one or multiple joints. The main types of JIA include systemic JIA, oligoarticular JIA, and polyarticular JIA. The specific type experienced by your child depends on their symptoms, the number of joints involved, and whether prominent fever and rash symptoms are present.
Similar to other forms of arthritis, JIA exhibits characteristic symptom flare-ups and remissions patterns.
Diagnosis
Diagnosing JIA can be challenging because knee pain can stem from various conditions. No test can confirm the diagnosis, but certain tests can help rule out other conditions with similar symptoms.
Blood tests are commonly performed for suspected cases of JIA. These may include:
- Erythrocyte sedimentation rate (ESR): This measures the rate at which red blood cells settle in a tube of blood, indicating inflammation levels.
- C-reactive protein (CRP): This test also measures inflammation levels but on a different scale than ESR.
- Antinuclear antibody (ANA): ANA is a protein associated with autoimmune diseases like arthritis and indicates increased risk of inflammation.
- Rheumatoid factor: These antibodies, sometimes present in JIA, suggest a higher risk of arthritis-related damage.
- Cyclic citrullinated peptide (CCP): Like rheumatoid factor, CCP antibodies can indicate increased risk of damage in JIA.
However, it's important to note that most children with JIA do not show significant abnormalities in blood tests.
Imaging examinations such as X-rays or MRI scans may be conducted to rule out other conditions, such as fractures, tumors, infections, or congenital abnormalities. These exams are also used periodically to monitor bone development and detect joint damage after the diagnosis is confirmed.
Management
Treatment for JIA aims to help children maintain normal physical and social activity. Combination therapy often reduces pain and swelling, maintains movement and strength, and prevents complications.
Medications commonly used to help children with JIA include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen and naproxen sodium, reduce pain and swelling. Side effects may include stomach pain and, less commonly, kidney and liver disorders.
- Disease-modifying antirheumatic drugs (DMARDs) like methotrexate used when NSAIDs alone are insufficient or when there is a high risk of joint damage. Methotrexate can be taken alongside NSAIDs to slow JIA progression, with side effects such as nausea, liver impairment, and increased infection risk.
- Biologic agents, including tumor necrosis factor (TNF) blockers like etanercept, adalimumab, golimumab, and infliximab, reduce inflammation and prevent joint damage. Other biological agents such as abatacept, rituximab, anakinra, and tocilizumab suppress the immune system differently. All biological agents carry an increased infection risk.
- Corticosteroids like prednisone may be used temporarily to control symptoms or treat inflammation outside the joints. Because their side effects can include growth impairment and increased infection susceptibility, they are typically used short-term.
Additionally, physiotherapy may be recommended to maintain joint flexibility, normal range of motion, and muscle tone. Joint supports or splints may also be suggested to protect joints and maintain functionality.
In severe cases, surgery may be necessary to improve joint function.
Complications
Serious complications can arise from JIA, but closely monitoring your child's condition and seeking appropriate medical help can significantly reduce these risks.
Complications of JIA may include:
- Eye disorders: Certain forms of JIA can lead to eye inflammation. Without treatment, this inflammation may progress to cataracts, glaucoma, and blindness. Since eye inflammation can occur without obvious symptoms, regular eye examinations by an ophthalmologist are crucial for children with JIA.
- Growth disturbances: JIA can impact bone growth and development in children. Some medications used in JIA treatment, particularly corticosteroids, may impede growth. Regular monitoring and treatment adjustments can help mitigate these effects.
Prevention
Preventing JIA is challenging. In children with genetic predispositions, efforts can be made to modulate the immune system through breastfeeding, probiotics (beneficial bacteria found in yogurt), avoiding tobacco, and minimizing unnecessary antibiotic use.
When to see a doctor?
If your child experiences joint pain, swelling, or stiffness for more than one week, especially alongside a fever, take them to the doctor.
Looking for more information about other diseases? Click here!
- dr. Monica Salim
Juvenile idiopathic arthritis (2022) Mayo Clinic. Mayo Foundation for Medical Education and Research. Available at: https://www.mayoclinic.org/diseases-conditions/juvenile-idiopathic-arthritis/symptoms-causes/syc-20374082 (Accessed: March 9, 2023).
MD, A.G. (2019) Juvenile idiopathic arthritis: Diagnosis, treatment and prevention via drgreene.com, Juvenile Idiopathic Arthritis: Diagnosis, Treatment and Prevention via DrGreene.com. Available at: https://www.drgreene.com/articles/juvenile-idiopathic-arthritis (Accessed: March 9, 2023).
Juvenile idiopathic arthritis (JIA) (2021) National Institute of Arthritis and Musculoskeletal and Skin Diseases. U.S. Department of Health and Human Services. Available at: https://www.niams.nih.gov/health-topics/juvenile-arthritis (Accessed: March 9, 2023).