Definition
Breast milk or breastfeeding jaundice occurs when a newborn develops jaundice related to breastfeeding. Jaundice is characterized by a yellowish discoloration of the skin and the white part of the eyes due to increased bilirubin levels in the blood. This condition often occurs in the early weeks of life, especially premature babies.
During the first few days of life, it is normal for a newborn to appear slightly yellow, typically between days 1 and 5, with the yellowish color becoming most noticeable around days 3 or 4.
Increased bilirubin levels in newborns occur for several reasons:
- Newborns have a higher rate of bilirubin production because of the shorter lifespan of their red blood cells and a higher concentration of red blood cells than adults.
- The liver function of newborns is immature, leading to slower bilirubin metabolism.
- Some newborns may experience delayed passage of the first stool (meconium), which can result in increased reabsorption of bilirubin in the intestines.
In most newborns, jaundice is referred to as physiological jaundice and is usually harmless.
Causes
Breastfeeding jaundice typically occurs during the first week of life when breastfeeding begins. In some cases, newborns may not receive adequate breast milk intake, leading to increased bilirubin levels due to the reabsorption of bilirubin in the intestines.
Insufficient milk intake can also delay the passage of a baby's first stool, which contains a significant amount of bilirubin. This reabsorbed bilirubin can then re-enter the baby's bloodstream. However, it's important to note that breastfeeding should and can be continued in most cases. Increasing the frequency and duration of breastfeeding sessions can help reduce the risk of jaundice.
Breast milk jaundice, on the other hand, commonly occurs in the second week of life or later and may persist for several weeks. While the exact mechanism behind breast milk jaundice is not fully understood, it is believed that certain substances in breast milk may inhibit the baby's liver's ability to process bilirubin.
Risk factor
Breastfeeding jaundice is more common in newborns who are premature (less than 37 weeks of gestation). Premature babies may have difficulty breastfeeding effectively, resulting in reduced breast milk intake.
Moreover, following a strict breastfeeding schedule (e.g., feeding every 3 hours for 10 minutes) or using a pacifier when the baby shows hunger cues can also heighten the risk of breastfeeding jaundice.
On the other hand, breast milk jaundice is believed to have a genetic predisposition. This condition affects approximately one-third of all newborns who exclusively receive breast milk.
Symptoms
When jaundiced, the skin and the white part of the eye (sclera) take on a yellowish appearance.
Diagnosis
Laboratory tests that can be performed include:
- Bilirubin levels (total and direct)
- Blood smear examination to observe the shape and size of blood cells
- Blood type test
- Complete blood count (CBC)
- Reticulocyte count (number of immature red blood cells)
Sometimes, a blood test to assess the glucose-6-phosphate dehydrogenase (G6PD) enzyme may be conducted. G6PD is a protein crucial for the proper functioning of red blood cells. This test helps ensure there are no other more serious causes of jaundice.
Another consideration is temporarily discontinuing breastfeeding and providing formula milk for 12 to 24 hours. This is done to observe if the bilirubin levels decrease. However, it's important to note that this test is not always necessary.
Management
The management will depend on:
- Your baby's bilirubin levels, which typically increase during the first week of life
- The rate at which the bilirubin levels are rising
- Whether your baby was born prematurely
- Your baby's breastfeeding history
- Your baby's age
Newborns normally have higher levels of bilirubin than older children or adults. However, therapy is not always needed; strict observation may be sufficient.
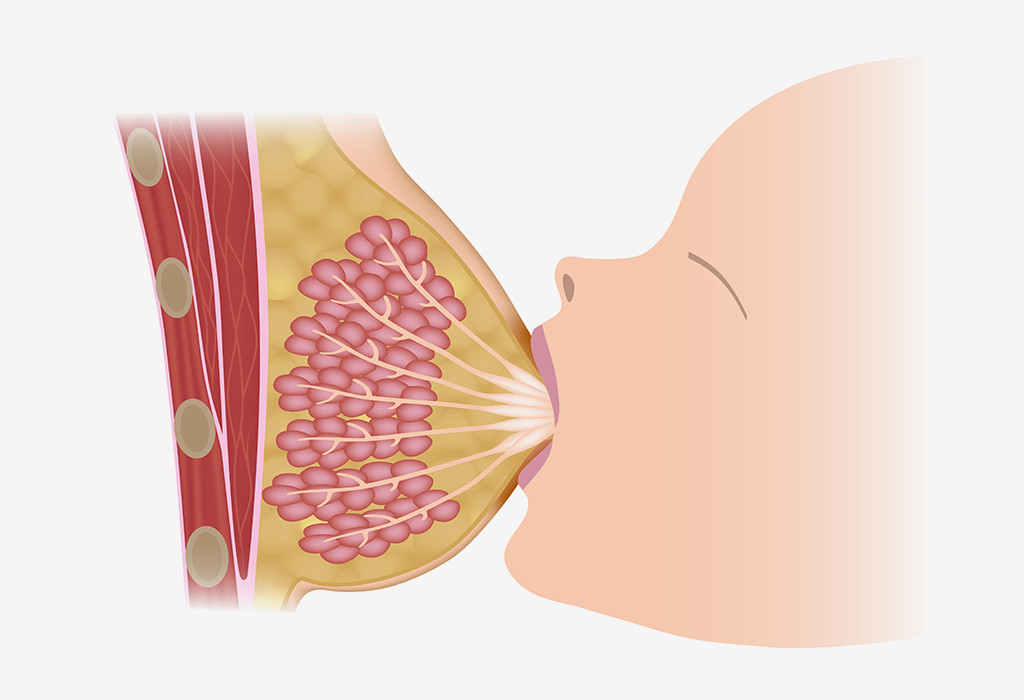
Most newborns with jaundice can continue breastfeeding. Frequent breastfeeding can stimulate the mother's milk supply, increase the baby's calorie and fluid intake, and reduce bilirubin levels. In cases where the baby cannot breastfeed effectively, fluids may be administered intravenously to increase hydration and lower bilirubin levels.
Phototherapy, where the baby is placed under a special blue light, may help break down excess bilirubin. With proper monitoring and therapy, babies typically recover fully from jaundice, which should resolve by 12 weeks of age.
Complications
In true breast milk jaundice, most cases do not experience complications. However, if babies with very high bilirubin levels do not receive appropriate medical treatment, they may face serious complications, including permanent brain damage.
Prevention
To prevent jaundice caused by insufficient breast milk intake, ensure your baby receives enough milk by following these steps:
- Breastfeed your baby approximately 10 to 12 times daily, starting from the first day of life. Feed your baby whenever they show signs of hunger, such as sucking on their fingers or playing with their lips, as this is how babies communicate hunger cues.
- Avoid waiting until your baby starts crying to initiate breastfeeding, as this may disrupt the feeding process.
- Allow your baby adequate time on each breast as long as they are actively sucking and swallowing. A well-fed baby will exhibit signs of satisfaction, such as relaxing, opening their fists, and slowly falling asleep.
If breastfeeding is challenging, promptly seek a lactation consultant or doctor's assistance. Babies born before 37 or 38 weeks of gestation often require additional support. Mothers may need to express or pump breast milk to ensure an adequate supply while mastering breastfeeding.
Increasing breastfeeding or pumping frequency (up to 12 times a day) can boost the amount of breast milk your baby receives, lowering bilirubin levels.
Consult your doctor before introducing formula milk to your newborn. Continuing breastfeeding is ideal, as babies benefit from their mother's breast milk. While formula-fed babies may appear calmer, supplementing with formula can diminish breast milk production.
If your breast milk supply is low due to low demand from your baby (e.g., premature babies), temporary formula milk use may be necessary. Continue pumping breast milk to stimulate production until your baby's condition improves and they can breastfeed effectively.
Skin-to-skin contact is beneficial for both babies and mothers. It promotes better breastfeeding and enhances breast milk production.
When to see a doctor?
If you are breastfeeding and notice your baby's skin or eyes turning yellow, contact your doctor immediately. Your baby should undergo a prompt bilirubin-level examination. If the bilirubin level is high, it's important to rule out any other medical issues.
- dr. Lukita Tarigan
Breast feeding jaundice. Breastfeeding Jaundice and Breast Milk Jaundice. (n.d.). Retrieved March 23, 2023, from https://www.birthinjuryhelpcenter.org/jaundice-breastfeeding.html
Breast milk jaundice. Mount Sinai Health System. (n.d.). Retrieved March 23, 2023, from https://www.mountsinai.org/health-library/diseases-conditions/breast-milk-jaundice
Centers for Disease Control and Prevention. (2021, November 16). Jaundice. Centers for Disease Control and Prevention. Retrieved March 23, 2023, from https://www.cdc.gov/breastfeeding/breastfeeding-special-circumstances/maternal-or-infant-illnesses/jaundice.html