Definisi
Dislokasi sendi temporomandibular adalah suatu kondisi terjadinya pergesaran sendi yang menghubungkan struktur kondilus mandibula (tonjolan tulang dagu) dengan fossa temporal (permukaan tempurung kepala). Kondisi ini dapat terjadi pada satu sendi atau kedua sendi.
Normalnya, kondilus mandibula dan fossa temporal berada pada satu posisi membentuk suatu sendi yang dikenal dengan sendi temporomandibular. Kedua tulang ini membentuk sendi yang dihubungkan oleh jaringat ikat elastis (ligamen), tendon (jaringan tebal otot) dan otot. Keberadaan jaringan ini membuat sendi temporodomandibular tetap berada pada posisinya dan dapat bergerak fleksibel sesuai dengan fungsinya. Dislokasi (pergeseran) sendi temporomandibular terjadi saat komponen penunjangnya yaitu ligamen, tendon dan otot mengalami kelemahan atau kerusakan. Sehingga tidak ada struktur yang menahan hubungan sendi kondilus mandibula dengan fossa temporal.
Dislokasi sendi temporomandibular sering terjadi yaitu sekitar 7% dari seluruh populasi. Dislokasi juga dapat terjadi pada semua kelompok usia terutama pada rentang usia 20-40 tahun. Dislokasi pada kedua sendi lebih sering terjadi dibandingkan pada satu sendi. Kejadian dislokasi dapat bersifat akut atau bahkan berulang dari sebelumnya. Trauma pada wajah menjadi penyebab paling sering terjadinya dislokasi.
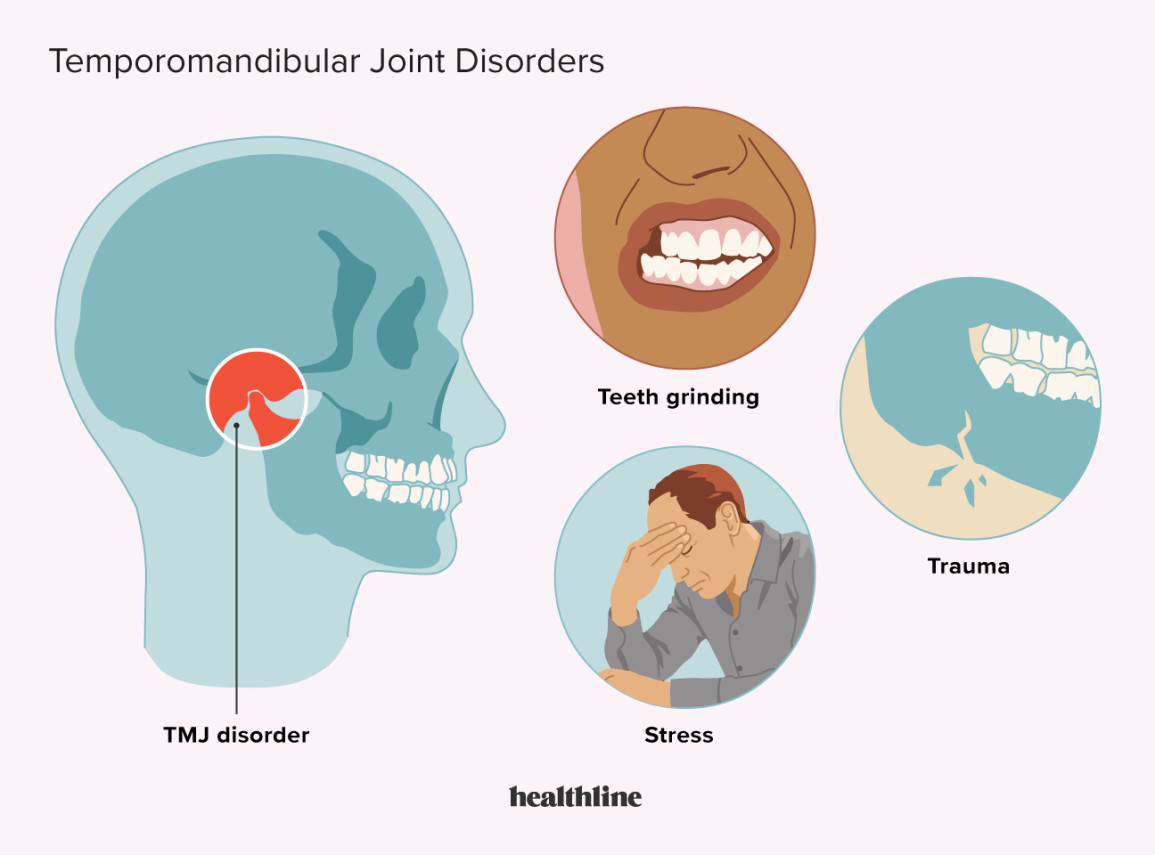
Penyebab
Penyebab dislokasi sendi temporomandibular dapat bersifat non-trauma (bukan trauma) atau trauma.
Penyebab non-trauma seperti di bawah ini:
- Membuka rahang terlalu kuat dan berlebihan seperti tertawa, menguap, bernyanyi dan membuka mulut terlalu lebar. Kondisi ini menyebakan peregangan terlalu jauh pada jaringan penunjang sendi sehingga menyebabkan sendi bergeser dari posisinya.
- Kejang
- Mengunyah berulang-ulang
- Adanya kelemahan pada ligamen
- Penyakit gangguan jaringan ikat
- Otot kaku seperti pada pasien penderita penyakit tetanus
- Efek samping obat
- Pasca menjalani suatu prosedur yang mengakibatkan peregangan sendi terlalu jauh seperti perawatan gigi, intubasi (memasukkan selang nafas ke mulut) dan bronkoskopi (pemeriksaan saluran napas).
Selain itu, penyebab paling sering adalah trauma akut pada wajah akibat kecelakaan atau terjatuh. Kondisi ini dapat menyebabkan kerusakan pada ligamen, otot dan tulang dagu patah. Adanya kerusakan secara langsung pada sendi temporomandibular menimbulkan terjadinya pergesaran pada sendi.
Baca selengkapnya mengenai cedera ligamen, di sini: Cedera Ligamen - Definisi, Penyebab, Gejala dan Pengobatannya
Faktor Risiko
Faktor risiko terjadinya dislokasi sendi temporomandibular adalah sebagai berikut:
- Pernah mengalami dislokasi sebelumnya
- Adanya kelainan bentuk struktur tulang
- Mengalami penyakit gangguan jaringan ikat yang memengaruhi keutuhan sendi
- Bertambahnya usia
- Menderita penyakit gangguan saraf
- Adanya perubahan pada susunan gigi
- Melakukan kebiasaan menggertakkan gigi dan mengunyah makanan yang keras
- Menderita penyakit peradangan pada sendi seperti osteoartritis atau reumatoid artritis
- Kerusakan pada rahang dan wajah
- Masalah psikologis seperti stres
- Gigitan yang tidak segaris
Gejala
Keluhan atau gejala yang sering ditemui dari dislokasi temporomandibular adalah nyeri bersifat akut pada bagian depan telinga. Nyeri akan semakin bertambah saat melakukan pergerakan pada rahang seperti mengunyah, membuka mulut, berbicara dan tertawa. Selain itu, terdapat beberapa gejala lain yang dapat dirasakan oleh pasien seperti di bawah ini:
- Adanya perubahan gigitan seperti gigi bagian atas dan bawah tidak sejajar
- Mengalami kesulitan saat berbicara dan menelan
- Rahang terlalu menonjol ke depan
- Kesulitan dalam menggerakkan rahang dan menutup mulut
- Air liur menetes
- Kaku saat rahang digerakkan
- Nyeri pada bagian wajah dan rahang
- Sisi wajah yang tidak simetris (sama)
Diagnosis
Dalam menegakkan diagnosis dari dislokasi sendi temporomandibular, dokter akan megumpulkan data yang diperoleh dari keluhan pasien dan pemeriksaan.
Wawancara Medis
Wawancara yang dilakukan antar dokter dan pasien. Dokter akan bertanya mengenai:
- Gejala yang dialami saat ini
- Riwayat kesehatan
- Riwayat konsumsi obat rutin
- Riwayat penyakit di keluarga
Pemeriksaan Fisik
Setelah melakukan wawancara medis, dokter akan melakukan pemeriksaan fisik umum dan khusus. Pemeriksaan fisik umum meliputi pengukuran tekanan darah, laju pernapasan, denyut nadi dan suhu tubuh. Selanjutnya, dokter melakukan pemeriksaan fisik khusus inpeksi dan palpasi pada bagian sendi temporomandibular.
Pada pemeriksaan inspeksi (mengamati) bagian depan telinga, dokter menilai adanya tonjolan atau lekukan kulit. Dokter juga menilai adanya ketidaksimetrisan pada wajah atau tidak serta pertemuan gigi atas dan bawah. Sedangkan pada pemeriksaan palpasi (meraba), dokter melakukan perabaan untuk mengetahui adanya nyeri tekan, lekukan dan tonjolan pada area sendi temporomandibular. Adanya dislokasi pada satu atau kedua sendi juga dinilai oleh dokter. Melalui wawancara medis dan pemeriksaan fisik, dislokasi sendi temporomandibular sudah bisa ditentukan.
Pemeriksaan Penunjang
Namun untuk mengetahui lebih jelas dapat dilakukan pemeriksaan penunjang radiologi seperti:
- Rontgen X-ray : untuk melihat adanya dislokasi atau tidak
- CT-Scan : biasanya dilakukan jika terdapat tumpang tindih antara dislokasi sendi dan patah tulang
- MRI (Magnetic Resonance Imaging) : untuk menilai jaringan penyusun sendi seperti ligamen atau otot. Dislokasi sendi temporomandibular yang berulang dapat dievaluasi dengan pemeriksaan MRI untuk mengetahui penyebabnya.
Tata Lksana
Dalam penatalaksanan dislokasi sendi temporomandibular, dokter akan menilai terlebih dahulu kestabilan kondisi pasien secara umum untuk mengetahui adanya kondisi kegawatdarutan yang dapat mengancam nyawa pasien. Komponen yang dapat dinilai berupa adanya sumbatan jalan nafas atau tidak, pernapasan pasien dan kecukupan suplai oksigen ke seluruh tubuh.
Selanjutnya, dokter memberikan obat antinyeri untuk meredakan nyeri karena pada dislokasi sendi temporomandibular pasien dapat merasakan nyeri mulai dari derajat ringan-berat. Obat relaksan (pelemas otot) juga diberikan untuk meredakan kaku otot akibat pergeseran sendi. Selain itu, dokter melakukan fiksasi (mempertahankan) sendi dengan menggunakan perban elastik pada bagian sendi temporomandibular supaya tidak terjadi pergeseran yang terlalu jauh.
Tujuan utama dari tata laksana dislokasi temporomandibular adalah mengembalikan sendi yang sudah mengalami pergeseran kembali ke posisi normalnya. Langkah ini dapat dilakukan oleh dokter dengan memposisikan ulang menggunakan teknik tertentu. Apabila melalui prosedur tersebut tidak berhasil maka dapat dilakukan tindakan operasi terutama pada kasus dislokasi yang disertai dengan patah tulang. Prosedur operasi juga dilakukan pada kondisi dislokasi sendi temporomandibular disebabkan karena adanya kelemahan pada ligamen penunjang sendi. Tujuan dari prosedur operasi ini yaitu menguatkan dan menstabilkan ligamen.
Komplikasi
Dislokasi sendi temporomandibular dapat bersifat akut atau kronik. Pada dislokasi yang terjadi secara berulang dan kronik dapat menimbulkan beberapa komplikasi yaitu adanya kerusakan ligamen dan jaringan penunjang sendi lainnya. Kerusakan dalam jangka waktu lama dapat menyebabkan terjadinya penyakit sendi. Selain itu, pada dislokasi sendi bagian atas dapat menimbulkan kerusakan pada saluran pendengaran bagian luar hingga mengalami gangguan pendengaran. Saraf pada wajah dan pendengaran juga dapat mengalami kerusakan. Cedera pada pembuluh darah diketahui juga dapat terjadi pada kasus dislokasi temporomandibular.
Pencegahan
Tedapat beberapa bentuk pencegahan yang dapat Anda lakukan untuk mencegah terjadinya dislokasi sendi temporomandibular, yaitu sebagai berikut:
- Tidak membuka mulut terlalu lebar saat menguap
- Anda dapat meletakkan kepalan tangan di bawah dagu untuk mencegah mulut terbuka lebar ketika menguap
- Menggunakan pelindung mulut ketika berolahraga dan berekreasi
- Saat berkendara selalu menggunakan helm
Kapan Harus Ke Dokter?
Apabila Anda mengalami keluhan nyeri pada bagian depan telinga disertai kesulitan saat berbicara, membuka mulut dan mengunyah. Sebaiknya Anda segera ke dokter gigi spesialis bedah mulut terdekat untuk mengetahui penyebabnya.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr. Monica Salim
Hilam J, Isom B. Mandible Dislocation – StatPearls. (2022). Retrieved 5 November 2022, from https://www.ncbi.nlm.nih.gov/books/NBK549809/
Roth E. What Is A Broken or Dislocated Jaw? – Heathline. (2022). Retrieved 5 November 2022, from https://www.healthline.com/health/broken-or-dislocated-jaw#recovery-and-outlook
Temporomandibular Joint (TMJ) Dislocation: Symptoms, Treatment & Prevention – Sherwoodparkdental. (2022). Retrieved 5 November 2022, from https://sherwoodparkdental.ca/dislocation-of-the-temporomandibular-joint-tmj/
Jabaz F. Temporomandibular Joint Dislocation – Radiopedia. (2022). Retrieved 5 November 2022, from https://radiopaedia.org/articles/temporomandibular-joint-dislocation
Jaw Dislocation – Heathdirect. (2022). Retrieved 5 November 2022, from https://www.healthdirect.gov.au/jaw-dislocation#prevented
Kandola R. Is my jaw broken or dislocated? – MedicalNewsToday. (2022). Retrieved 5 November 2022, from https://www.medicalnewstoday.com/articles/324412
Jaw Dislocation – drugs.com. (2022). Retrieved 5 November 2022, from https://www.drugs.com/cg/jaw-dislocation.html
Risk Factor for Temporomandibular Joint – WhincesterHospital. (2022). Retrieved 5 November 2022, from https://www.winchesterhospital.org/health-library/article?id=20232