Definisi
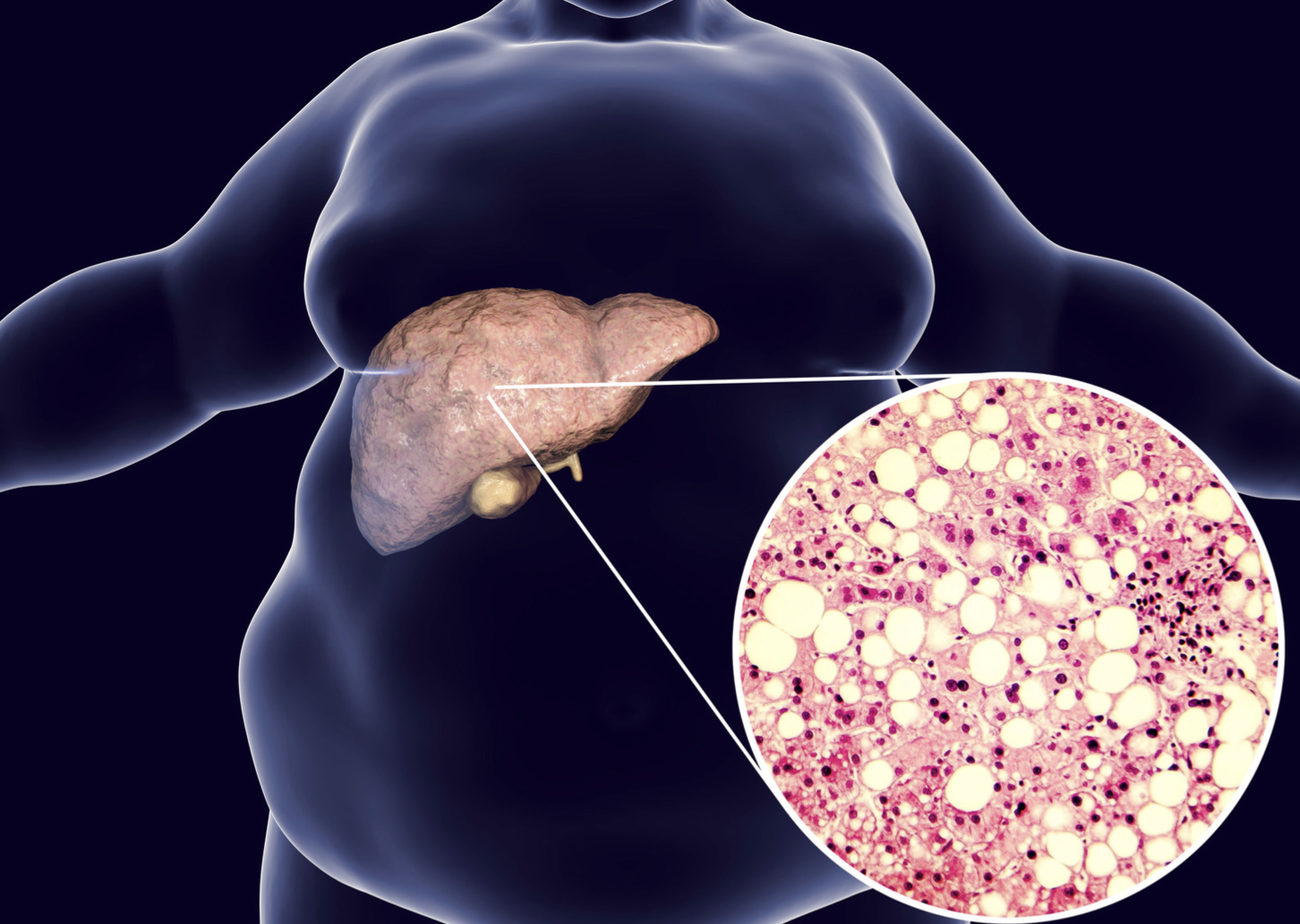
Perlemakan hati (fatty liver disease, hepatic steatosis) adalah akumulasi lemak berlebih pada hati. Terdapat dua jenis perlemakan hati, yaitu:
- Nonalcoholic Fatty Liver Disease (NAFLD), yaitu perlemakan hati yang dialami individu yang tidak mengonsumsi alkohol. NAFLD dibagi menjadi simple fatty liver dan Nonalcoholic Steatohepatitis (NASH).
- Simple fatty liver adalah kondisi perlemakan hati tanpa cedera pada sel
- NASH adalah kondisi perlemakan hati yang disertai dengan cedera pada sel. Sekitar 5–12% individu dengan NASH mengalami perburukan menjadi sirosis (rusaknya organ hati)
- Alcohol-related Fatty Liver Disease (AFLD), yaitu perlemakan hati yang berhubungan dengan konsumsi alkohol berlebih
Penyebab
Perlemakan hati disebabkan oleh tingginya asam lemak bebas pada hati. Pada NAFLD, kumpulan asam lemak bebas ini terjadi akibat:
- Masukan asam lemak berlebihan, contohnya pada kondisi obesitas, penurunan berat badan dengan cepat, atau overfeeding
- Gangguan oksidasi asam lemak bebas, contohnya pada defisiensi (kekurangan) vitamin B5
- Resistensi insulin, yaitu ketika sel tubuh tidak dapat merespon terhadap hormon insulin sehingga gula tidak dapat diambil oleh sel
- Gula darah tinggi (hiperglikemia), seperti pada diabetes tipe 2 atau prediabetes
Kombinasi dari hal-hal di atas dapat meningkatkan deposit lemak pada hati. Kumpulan lemak yang berlebih dapat merusak sel hati, sehingga menyebabkan peradangan dan perubahan jaringan menjadi jaringan parut. Hal ini dapat mengganggu fungsi hati.
Konsumsi alkohol secara berlebihan dapat menyebabkan gangguan oksidasi asam lemak dan peningkatan produksi lemak, sehingga menyebabkan AFLD. Pada awalnya, respon hati terhadap konsumsi alkohol adalah pembentukan steatosis, yaitu adanya lemak pada sel-sel hati. Steatosis terjadi pada 90% individu yang mengonsumsi alkohol sebanyak 4–5 porsi dalam sehari selama beberapa tahun. Steatosis dapat berkembang menjadi steatohepatitis, ketika perlemakan hati tersebut menyebabkan peradangan. Peradangan yang berkelanjutan dapat mengubah struktur hati menjadi jaringan ikat yang disebut fibrosis. Fibrosis yang berlangsung terus menerus dapat menyebabkan perubahan sel hati secara menyeluruh, disebut sirosis.
Faktor Risiko
Banyak hal yang dapat meningkatkan risiko mengalami NAFLD, antara lain:
- Kolesterol tinggi
- Trigliserida tinggi
- Mengalami sindrom metabolik
- Obesitas, terutama jika obesitas terjadi secara sentral (di sekitar perut)
- Mengalami sleep apnea (gangguan tidur)
- Mengalami diabetes tipe 2
Sedangkan NASH lebih sering terjadi pada:
- Usia lebih tua
- Mengalami diabetes
- Memiliki obesitas sentral
Pada AFLD, faktor risiko yang berperan adalah konsumsi alkohol lebih dari 10–80g/hari (moderat). Konsumsi alkohol lebih dari 60 g pada laki-laki dan 20 g pada perempuan per hari meningkatkan risiko sirosis secara signifikan. Jenis alkohol berupa bir dapat meningkatkan risiko AFLD dibandingkan minuman anggur. Perempuan yang mengonsumsi alkohol lebih sering mengalami AFLD dibandingkan laki-laki. Konsumsi alkohol dalam jumlah banyak, walaupun hanya beberapa hari, dapat meningkatkan risiko terjadinya perlemakan hati.
Gejala
NAFLD dan AFLD umumnya tidak menunjukkan gejala tertentu. Jika terdapat gejala, gejala tersebut tidak khas dan hanya terlihat seperti kelelahan atau nyeri pada perut kanan atas.
Jika Anda sudah mengalami sirosis atau NASH, gejala yang ditunjukkan antara lain:
- Pembengkakan perut (asites)
- Pelebaran pembuluh darah di bawah kulit
- Pembesaran limpa
- Telapak tangan berwarna merah
- Kulit dan bagian putih mata (sklera) berwarna kuning (jaundice)
Diagnosis
Karena kondisi NAFLD dan AFLD tidak menunjukkan gejala pada sebagian besar kasus, diagnosis umumnya baru dapat ditegakkan setelah melakukan pemeriksaan lanjutan atau telah terjadi gejala yang mengarah pada kerusakan hati. Pemeriksaan yang dapat dilakukan untuk menilai fungsi hati antara lain:
- Pemeriksaan darah, yaitu dengan pemeriksaan darah lengkap, pemeriksaan fungsi hati dan enzim hati, pemeriksaan serologi hepatitis, pemeriksaan gula darah sewaktu, HbA1c, dan profil lipid (kolesterol dan trigliserida).
- Peningkatan enzim hati merupakan salah satu tanda awal dari adanya peradangan hati.
- Pemeriksaan pencitraan, meliputi USG abdomen, CT scan atau MRI. Umumnya, tes awal yang dilakukan adalah USG abdomen.
- Pemeriksaan biopsi liver. Jika pemeriksaan lain tidak memberikan cukup hasil, dokter Anda dapat mengambil sampel jaringan dari hati (biopsi). Jaringan akan diperiksa di laboratorium untuk mencari adanya peradangan pada sel tersebut.
Dokter Anda dapat mencurigai adanya AFLD jika Anda memiliki riwayat konsumsi alkohol lebih dari 210 g/minggu pada laki-laki dan 140g/minggu pada perempuan selama 2 tahun atau terdapat hasil pemeriksaan fungsi hati yang tidak normal.
Tata Laksana
Perlemakan hati pada tahap awal, baik NAFLD pada fase simple fatty liver dan AFLD, bersifat reversibel atau dapat dikembalikan seperti semula dengan modifikasi gaya hidup.
- Penurunan berat badan. Mengurangi 3–5% dari berat badan awal Anda dapat mengurangi risiko mengalami NAFLD. Target penurunan berat badan umumnya adalah 10% dari berat badan awal. Penurunan berat badan dilakukan dengan mengurangi konsumsi kalori 500-1000 kkal dari konsumsi sehari-hari. Konsultasikan menu diet dan metode ini dengan dokter dan ahli gizi Anda.
- Mengurangi konsumsi makanan tinggi lemak dan tinggi karbohidrat.
- Melakukan aktivitas fisik 150-200 menit/hari dengan intensitas sedang dan bersifat aerobik.
- Menghentikan konsumsi alkohol. Konsultasikan langkah-langkah untuk membantu Anda mengurangi konsumsi alkohol dengan dokter Anda.
Saat ini belum ada obat-obatan yang secara spesifik mengobati perlemakan hati.
Pada tahap kerusakan hati yang lebih lanjut, seperti NASH hingga sirosis, tata laksana utama yang dapat dilakukan adalah transplantasi hati. Transplantasi hati adalah pilihan terakhir jika seseorang tidak merespon terhadap modifikasi gaya hidup.
Komplikasi
Komplikasi utama dari perlemakan hepar, baik NAFLD maupun AFLD, adalah sirosis. Sirosis merupakan stadium akhir dari perlukaan pada hati. Sirosis terjadi akibat iritasi berulang pada hati. Seiring dengan usaha hati untuk menanggulangi iritasi, beberapa jaringan hati akan berubah menjadi jaringan parut (fibrosis). Jika iritasi berlanjut, fibrosis akan menyebar ke seluruh bagian hati. Hal ini dapat menyebabkan:
- Penumpukan cairan pada abdomen (perut), yaitu asites
- Pembengkakan pada esofagus (varises esofagus) yang dapat robek dan berdarah
- Penurunan kesadaran, kebingungan dan bicara melantur (ensefalopati hepatikum)
- Kanker hati
- Gagal hati, yaitu kondisi hati tidak lagi berfungsi
Pencegahan
Pencegahan penting untuk mengurangi risiko perlemakan hati, mengembalikan kondisi hati seperti semula, dan mencegah perburukan. Untuk itu, Anda dapat melakukan hal-hal di bawah ini:
- Menurunkan berat badan hingga mencapai berat badan ideal. Lakukan penurunan berat badan secara bertahap dengan metode yang sesuai dengan anjuran.
- Mengonsumsi makanan yang seimbang. Diet mediterania umumnya direkomendasikan oleh dokter pada kondisi perlemakan hati. Konsultasikan hal ini dengan dokter Anda.
- Melakukan aktivitas fisik.
- Mengurangi konsumsi alkohol atau berhenti konsumsi alkohol. Konsumsi alkohol yang dianjurkan adalah di bawah 14 unit per minggu. Satu unit alkohol sama dengan 25 ml spirit.
Kapan Harus ke Dokter?
Jika Anda mengalami gejala di atas, periksakan kondisi Anda ke fasilitas kesehatan terdekat untuk dilakukan pemeriksaan lebih lanjut. Segera kunjungi fasilitas kesehatan jika Anda mengalami mata atau kulit yang menguning, kebingungan atau penurunan kesadaran dan muntah darah.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Nadia Opmalina
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018; 67(1):328-57.
Vozzo CF, et al. (2020). Alcoholic liver disease. Cleveland Clinic. Available at: https://my.clevelandclinic.org/departments/digestive/medical-professionals/hepatology/alcoholic-liver-disease
Osna, N. A., Donohue, T. M., Jr, & Kharbanda, K. K. (2017). Alcoholic Liver Disease: Pathogenesis and Current Management. Alcohol research : current reviews, 38(2), 147–161.
Mayo Clinic Staff. (2021). Nonalcoholic fatty liver disease. MayoClinic. Available at: https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/symptoms-causes/syc-20354567
National Health Service. (2018). Alcohol-related liver disease. NHS UK. Available at: https://www.nhs.uk/conditions/alcohol-related-liver-disease-arld/