Definition
Portal hypertension is the increase in pressure inside the portal venous system. The portal vein is responsible for transporting blood from the stomach, pancreas, and other digestive organs to the liver. This vessel differs from other veins that return blood to the heart.
The liver plays a crucial role in blood circulation by filtering toxins and metabolic by-products produced in the digestive tract. When blood pressure becomes excessively high, it is termed portal hypertension.
Portal hypertension can pose a serious threat, even though it may be detected before reaching a critical stage. Elevated pressure arises due to blockages or constriction in the veins, requiring increased pressure for blood to pass through. Prolonged high pressure can lead to tissue damage.
Regrettably, this medical condition is not easily detected and diagnosed early. Typically, portal hypertension manifests symptoms before its discovery. In Western countries, the most common causes are liver cirrhosis or the development of scar tissue hindering liver function. In other regions, such as Africa, portal hypertension is commonly caused by schistosomiasis, a worm infection endemic to the continent.
Causes
Several conditions can cause portal hypertension, which can be grouped into three categories:
- intrahepatic (originating from the liver)
- Schistosomiasis (Schistosoma infection)
- Liver cirrhosis (formation of scar tissue)
- Chronic liver inflammation
- Cholangitis (bile duct inflammation)
- Toxic exposure to substances like arsenic, vinyl chloride, or copper,
- Vitamin A poisoning
- Increased pressure or blockage in the blood circulation of the portal vein,
- Enlargement of the lymph nodes
- Artery-vein malformations (abnormal blood vessel formation)
- Tumors exert pressure on the vein
- Blood clotting in the lymph or portal vein.
- Post-hepatic
- Inflammation of the heart's surface layer
- Tumors
- Strictures of the inferior vena cava under the right atrium of the heart.
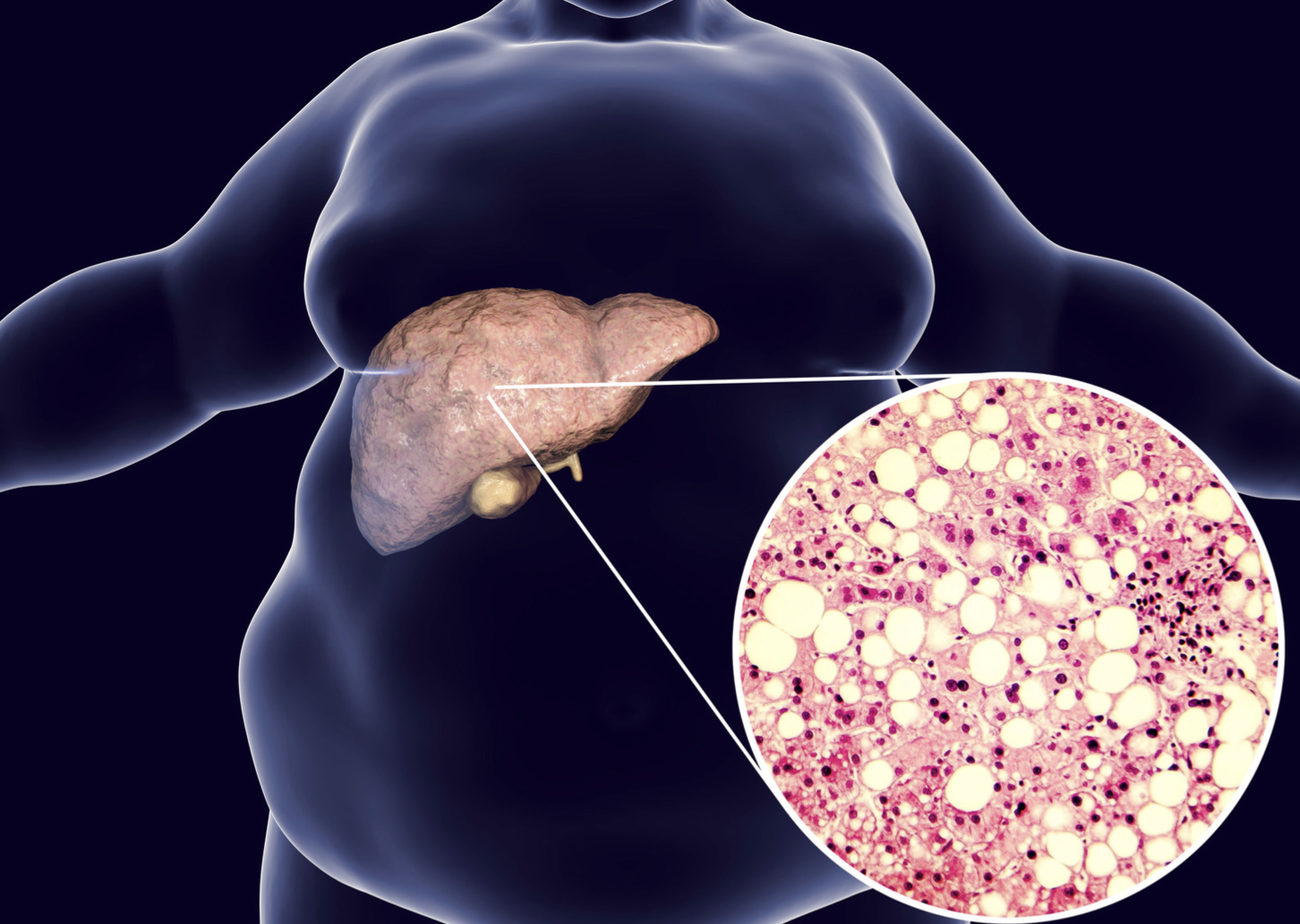
The liver has a remarkable ability to heal itself when injured, resulting in the formation of scar tissue. However, excessive scar tissue can impair liver function. The primary cause of portal hypertension is liver cirrhosis, which occurs when scar tissues develop on the liver.
Cirrhosis can lead to uneven walls in the portal vein, causing increased pressure on the blood flow passing through it. This heightened pressure can result in the enlargement of the vein, leading to the formation of fragile varices. Varices can occur along the digestive tract, from the esophagus into the stomach, and are prone to easy bleeding.
Risk factors
Individuals at a high risk of developing liver cirrhosis are also susceptible to portal hypertension. Factors that elevate the risk of hepatitis, subsequently increasing blood pressure in the portal vein, include:
- Excessive alcohol consumption.
- Liver infections or inflammation.
- Sharing needles for illegal drug injections.
- Use of unsterilized tattoo and piercing tools.
- Occupation in healthcare facilities with a high likelihood of contact with infected needles or blood.
- Pregnancy in women with hepatitis.
- Engaging in sexual activities with multiple partners.
Symptoms
The primary symptoms that may manifest in portal hypertension include:
- Digestive tract bleeding: Evidenced by red or black feces.
- Vomiting blood: Resulting from the rupture of enlarged veins.
- Ascites: The accumulation of fluid in the abdominal space.
- Encephalopathy: A condition that can lead to brain damage, with one manifestation being unconsciousness.
If left unaddressed, ascites can exacerbate, causing abdominal enlargement. This progression may lead to a stiff and bloated abdomen, ultimately resulting in breathing difficulties.
Diagnosis
History taking
The diagnosis of portal vein hypertension involves a comprehensive approach, encompassing history-taking, physical examination, and supplementary tests such as laboratory work and imaging studies. During history-taking, the doctor inquires about symptoms and complaints. It's noteworthy that patients often lack noticeable symptoms before complications arise, with blood vomit and black stool being the most common indicators. The doctor also delves into the patient's past illnesses, medical history, prior medications, and family medical history to establish a comprehensive understanding.
Physical examination
A thorough physical examination covers the entire body, with the observed signs dependent on the underlying cause of portal hypertension. If cirrhosis is the causative factor, the doctor may identify the following manifestations:
- Jaundice: Yellowing of the skin or sclera.
- Ascites: Accumulation of fluid in the abdominal space.
- Spider nevi: Spider-web-like veins on the skin.
- Palmar erythema: Redness of the palms.
- Swelling of breast tissue in males.
Laboratory and Imaging
Examinations that can support the diagnosis include:
- Laboratory Exams:
- Complete blood test
- Glucose test
- Liver function
- Renal function
- Bilirubin levels
- Blood protein assessment
- Electrolyte levels
- Blood coagulation studies
- Radiology or Imaging:
- Doppler ultrasonography
- Endoscopy
- CT-Scan
Management
The management of portal hypertension depends on the underlying cause and associated complications. Doctors may prescribe medications to lower blood pressure and relax blood vessels, particularly the portal vein. These medications can also reduce the risk of internal organ bleeding.
In cases of fluid accumulation, medications to facilitate fluid removal from the body may be prescribed. Additionally, patients may be advised to limit their salt intake to mitigate fluid accumulation.
Procedures such as sclerotherapy or vessel ligation may be considered. Sclerotherapy, performed by a digestive doctor, involves injecting fluid into bleeding varices to control or prevent the risk of bleeding. Vessel ligation employs a medical band to halt the blood supply to enlarged vessels.
Lifestyle and dietary changes are often recommended to safeguard liver function. This may include:
- Consuming a balanced meal and adopting a low-salt diet.
- Abstaining from alcohol consumption.
- Regular exercise.
- Quitting or avoiding smoking.
Complications
Complications associated with portal vein hypertension include:
- Decreased Platelet Count (Thrombocytopenia): A reduction in the number of platelets.
- Bleeding from Enlarged Veins in the Esophagus: This can lead to significant gastrointestinal bleeding.
- Infection and Inflammation of the Abdominal Layer: Compromised integrity of the layer covering the abdomen.
- Sudden Bleeding in the Digestive Tract: Unanticipated bleeding within the digestive system.
- Anemia and Iron Deficiency: Resulting from prolonged bleeding.
- Hepatorenal Syndrome: Dysfunction of renal function due to the worsening of liver disease.
Prevention
Prevention involves adopting a healthy lifestyle, which includes avoiding excessive alcohol consumption. Additionally, for those at risk of hepatitis exposure, considering hepatitis vaccination is advisable to mitigate the potential risks associated with the condition.
When to see a Doctor?
If symptoms worsen, like vomiting blood, it's recommended to seek advice from either an internist or a specialist in gastroenterohepatology. The doctor will conduct a medical interview, a physical examination, and additional tests to diagnose the underlying cause and determine the appropriate management.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Oliver TI, Sharma B, John S. Portal Hypertension. [Updated 2022 May 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507718/
Healthline. Portal hypertension. January 2019. Available from: https://www.healthline.com/health/portal-hypertension
Cleveland Clinic. Portal hypertension. July 2022. Available from: https://my.clevelandclinic.org/health/diseases/4912-portal-hypertension#.