Definition
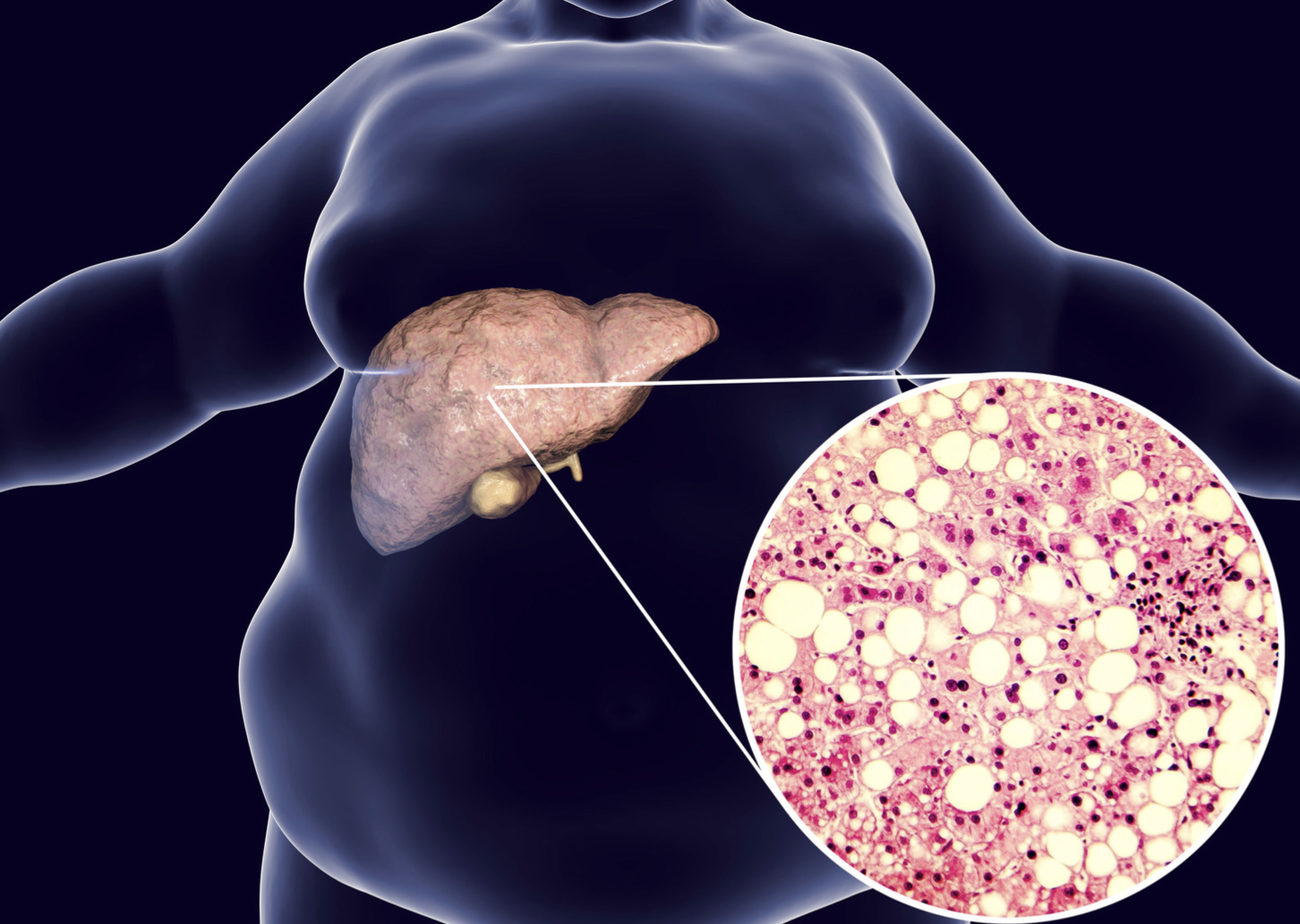
Fatty liver (hepatic steatosis) is an accumulation of excessive fat on the liver. There are two kinds of fatty liver which are:
- Nonalcoholic Fatty Liver Disease (NAFLD), is liver fat accumulation in individuals who do not consume alcohol. NAFLD is divided into simple fatty liver and non-alcoholic steatohepatitis (NASH).
- Simple fatty liver is a condition of liver fat accumulation without cell injury.
- NASH is a condition of liver fat accumulation accompanied by cell injury. About 5–12% of individuals with NASH progress to cirrhosis (liver organ damage).
- Alcohol-related Fatty Liver Disease (AFLD), is liver fat accumulation associated with excessive alcohol consumption.
Causes
Fatty liver is caused by elevated Free fatty acids (FFA) in the liver. In NAFLD, the accumulation of FFA is caused by:
- Excessive fatty acid intake, such as in cases of obesity, drastic weight loss, or overfeeding.
- Disruption of FFA oxidation, for example, due to a deficiency of vitamin B5.
- Insulin resistance which occurs when the body's cells are unable to respond to insulin hormone, causing sugar to remain unabsorbed by cells.
- Hyperglycemia, or elevated glucose levels in the blood, as seen in type 2 diabetes or prediabetes.
A combination of these factors can increase fat deposition in the liver. Excessive fat accumulation can damage liver cells, leading to inflammation and tissue transformation into scar tissue, disrupting liver function.
Excessive alcohol consumption can disrupt fatty acid oxidation and increase fat production, leading to AFLD. Initially, the liver responds to alcohol consumption by developing steatosis, the accumulation of fat in liver cells. Steatosis occurs in 90% of individuals who consume alcohol at a rate of 4–5 drinks per day for several years. Steatosis can progress to steatohepatitis when the fatty liver becomes inflamed. Continuous inflammation can cause structural changes in the liver, forming connective tissue known as fibrosis. Persistent fibrosis can lead to extensive changes in liver cells, ultimately resulting in cirrhosis.
Risk factor
There are several factors that can increase the risk of NAFLD, including:
- High cholesterol
- High triglycerides
- Metabolic syndrome
- Obesity, particularly central obesity (around the abdomen)
- Sleep apnea (a sleep disorder)
- Type 2 diabetes
On the other hand, NASH is more common in:
- Older individuals
- Those with diabetes
- Individuals with central obesity
Regarding AFLD, the risk factors include consuming alcohol over 10-80 g/day (moderate consumption). Consuming more than 60 g/day for males and 20 g/day for females significantly increases the risk of cirrhosis. Beer consumption poses a higher risk of AFLD compared to wine. Additionally, females who consume alcohol frequently are more likely to develop AFLD than males. Even a few days of excessive alcohol consumption can increase the risk of fatty liver.
Symptoms
NAFLD and AFLD generally do not exhibit specific symptoms. In the rare instances where symptoms manifest, they are often nonspecific and may include fatigue or upper right abdominal pain.
However, if you already have cirrhosis or NASH, you may experience:
- Abdominal swelling (ascites)
- Dilated blood vessels under the skin
- Enlarged spleen
- Red palms
- Yellowing of the skin and whites of the eyes (jaundice)"
Diagnosis
Since NAFLD and AFLD often do not present symptoms, diagnosis is typically made through diagnostic tests or when symptoms indicate liver damage. The following examinations are commonly used to assess liver function:
- Blood tests: These include a complete blood count, liver function tests, liver enzymes, hepatitis serology tests, random blood sugar test, HbA1c, and lipid profile (cholesterol and triglycerides).
- Elevated liver enzymes are often early indicators of liver inflammation.
- Imaging tests: Imaging techniques such as abdominal ultrasound (USG), CT scan, or MRI may be utilized. Abdominal ultrasound is typically the initial test performed.
- Liver biopsy: A liver biopsy may be performed if other tests are inconclusive. During this procedure, a small tissue sample is taken from the liver and examined in a laboratory for signs of inflammation in the cells.
AFLD is suspected if there is a history of alcohol consumption exceeding 210 g/week in men or 140 g/week in women for a period of 2 years, or if abnormal liver function test results are present.
Management
Fatty liver, whether it's NAFLD (nonalcoholic fatty liver disease), simple fatty liver, or AFLD (alcohol-related fatty liver disease), can be reversible or improved with lifestyle modifications. Here are some key strategies:
- Gradual weight loss: Aim to lose 3–5% of your initial body weight initially, aiming to achieve a 10% reduction overall. This can be accomplished by reducing your daily calorie intake by 500-1000 calories. Consult with your doctor and a nutritionist to develop personalized diet plans and strategies tailored to your needs and goals.
- Reduce consumption of high-fat and high-carbohydrate foods.
- Engage in physical activity for 150-200 minutes per week with moderate intensity and aerobic nature.
- Stopping alcohol consumption is crucial for improving liver health. Consult with your doctor for steps to help reduce your alcohol consumption.
At present, there is no specific medication available for treating fatty liver.
In cases of advanced liver damage, such as NASH progressing to cirrhosis, the primary treatment option is liver transplantation. Liver transplantation is considered a last resort if the individual does not respond to lifestyle modifications.
Complications
The primary complication of fatty liver, whether NAFLD or AFLD, is cirrhosis, which represents the final stage of liver damage. Cirrhosis develops due to persistent liver irritation, transforming liver tissues into scar tissue (fibrosis). If the irritation continues, fibrosis can spread throughout the liver, resulting in various complications such as:
- Accumulation of fluid in the abdomen (ascites)
- Swelling in the esophagus (esophageal varices) that may rupture and cause bleeding
- Decreased consciousness, confusion, and slurred speech (hepatic encephalopathy)
- Liver cancer
- Liver failure, characterized by impaired liver function.
Prevention
Prevention is crucial in reducing the risk of fatty liver, restoring liver health, and preventing further deterioration. Individuals may consider the following strategies:
- Gradually achieving and maintaining an ideal body weight through methods endorsed by medical guidelines.
- Adopting a balanced diet, with the Mediterranean diet often recommended by healthcare professionals for managing liver steatosis. Consultation with a doctor is advised to customize dietary plans.
- Incorporating regular physical activity into daily routines.
- Limiting alcohol consumption or abstaining entirely. The recommended alcohol intake is typically below 14 units per week, with one alcohol unit equivalent to 25 ml of spirits
When to see a doctor?
If you experience any of the symptoms mentioned above, seek evaluation at the nearest healthcare facility for further examination. It is especially important to go to a healthcare facility promptly if you notice yellowing of the eyes or skin (jaundice), confusion or reduced consciousness, or if you vomit blood.
Looking for more information about other diseases? Click here!
- dr Nadia Opmalina
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018; 67(1):328-57.
Vozzo CF, et al. (2020). Alcoholic liver disease. Cleveland Clinic. Available at: https://my.clevelandclinic.org/departments/digestive/medical-professionals/hepatology/alcoholic-liver-disease
Osna, N. A., Donohue, T. M., Jr, & Kharbanda, K. K. (2017). Alcoholic Liver Disease: Pathogenesis and Current Management. Alcohol research : current reviews, 38(2), 147–161.
Mayo Clinic Staff. (2021). Nonalcoholic fatty liver disease. MayoClinic. Available at: https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/symptoms-causes/syc-20354567
National Health Service. (2018). Alcohol-related liver disease. NHS UK. Available at: https://www.nhs.uk/conditions/alcohol-related-liver-disease-arld/