Definition
Central obesity or abdominal obesity refers to the excessive accumulation of fat in the abdominal region. This condition is not necessarily correlated with body mass index (BMI), meaning that individuals with a normal BMI (weight appropriate to height) can still develop central obesity. Studies have even indicated that those with a BMI <20 kg/m² may also be susceptible to central obesity and the associated health risks.
The prevalence of central obesity has been increasing globally year after year. While many people regard this condition as an inevitable part of aging, it is important to recognize that a larger waistline is linked to heightened health risks.
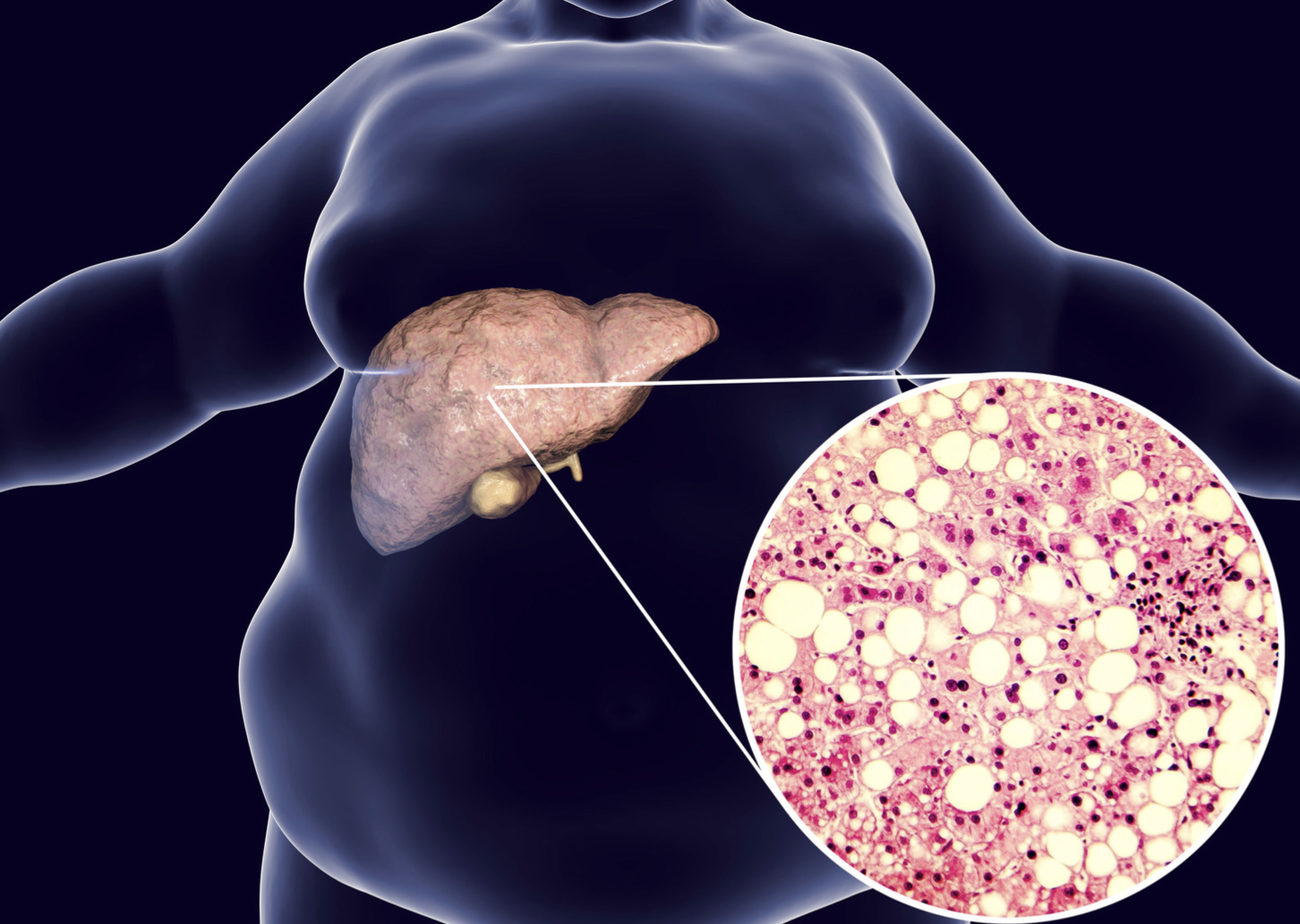
Visceral fat, or belly fat, is particularly concerning due to its significant role in triggering various health issues. This type of fat is more problematic than subcutaneous fat (the fat beneath the skin that can be pinched by hand). Visceral fat resides deep within the abdominal cavity, surrounding the internal organs. Unlike subcutaneous fat, visceral fat cannot be pinched, though it can be seen and measured.
Research suggests that fat cells, especially those in the abdominal region, are biologically active. These fat cells function similarly to an endocrine organ or gland, producing hormones and other substances that can have a profound impact on health. Although the role of these hormones is still under investigation, it is clear that excessive body fat, particularly belly fat, disrupts the normal balance and functioning of hormones.
Causes
A poor diet, characterized by the consumption of high-calorie and high-sugar foods such as sweets, cakes, biscuits, pizza, and chips, can lead to a dramatic increase in abdominal fat cells.
In addition, smoking and excessive alcohol consumption have been linked to an increased risk of central obesity and its associated health problems.
A sedentary lifestyle, such as sitting for extended periods (e.g., jobs with minimal physical activity), also contributes to the accumulation of belly fat, which over time leads to central obesity.
People with sedentary lifestyles burn fewer calories than those who are physically active, leading to greater long-term fat accumulation in the abdomen.
Other contributing factors to central obesity include sleep disorders, the use of certain medications (e.g., psychiatric drugs, anticonvulsants, insulin, and corticosteroids), and hormonal conditions such as polycystic ovary syndrome (PCOS), Cushing's syndrome, and hypothyroidism.
Risk Factor
With advancing age, particularly during middle age, the proportion of body fat relative to body weight tends to increase, especially in women. Weight gain typically occurs in the trunk region.
Fat accumulation in the lower body (resulting in a pear-shaped body) is primarily subcutaneous fat, whereas fat in the abdominal area (leading to an apple-shaped body) is predominantly visceral fat. Where fat accumulates is influenced by several factors, including genetics and hormonal regulation.
Symptoms
In the absence of comorbidities, individuals with central obesity may experience no symptoms beyond the visible accumulation of fat in the abdominal region.
Diagnosis
Central obesity is diagnosed by measuring waist circumference. An individual is classified as having central obesity if their waist circumference exceeds 90 cm for men or 80 cm for women. While this method is inexpensive and safe, it cannot differentiate between lean body mass and fat.
Computed tomography (CT) scans and magnetic resonance imaging (MRI) are considered the gold standard for assessing central obesity, as they can distinguish between visceral and subcutaneous fat. However, these imaging methods are expensive and limited in availability. Another drawback of CT scans is that they expose patients to radiation.
Management
To reduce abdominal fat, both exercise and a balanced diet are crucial. While staying physically active throughout the day and committing to regular structured exercise is more effective than diet alone, both approaches are essential.
The primary step in managing weight, particularly central obesity, is engaging in regular, moderate-intensity physical activity. A minimum of 30 minutes of exercise per day (preferably 60 minutes) is recommended to help control weight and reduce belly fat. Strength training exercises, such as weight-bearing activities, are also beneficial in targeting belly fat. Although spot exercises like sit-ups can strengthen abdominal muscles, they do not directly reduce visceral fat.
Diet plays an equally important role. Portion control should be observed, with an emphasis on complex carbohydrates, such as fruits, vegetables, and whole grains, along with protein. Simple carbohydrates, like white bread and sugary beverages, should be limited. Replacing saturated and trans fats with unsaturated fats is also advisable.
Consuming high-fiber foods, either through diet or supplements, has been associated with lower rates of obesity, hypertension, coronary heart disease, and stroke, and is linked to improved weight management.
Complications
Central obesity is associated with seven major health complications:
- Cardiovascular Disease. Visceral fat can trigger the release of cytokines, which regulate immune responses. These cytokines cause inflammation in the coronary blood vessels, contributing to atherosclerosis (fat buildup in blood vessels), which narrows the arteries and increases blood pressure. Excess abdominal fat can also elevate blood pressure, lower HDL cholesterol (good cholesterol), and heighten the risk of stroke.
- Type 2 Diabetes Mellitus. Research indicates that abdominal fat cells release large quantities of fatty acids, which can impair blood sugar and insulin metabolism. Individuals with significant visceral fat are likely to have decreased insulin sensitivity, a condition known as insulin resistance, increasing their risk of developing type 2 diabetes, as their bodies no longer respond effectively to insulin's blood sugar-lowering effects.
- Sleep Apnea. Increased visceral fat is linked to obstructive sleep apnea, as abdominal fat can restrict diaphragm movement and limit lung expansion.
- Inflammation. Visceral fat is particularly harmful due to its role in producing proteins and hormones that promote inflammation. This inflammatory response can damage blood vessels, impair liver function, and negatively impact carbohydrate and fat metabolism. These factors contribute to the development of atherosclerosis, leading to heart attacks and strokes.
- Metabolic Syndrome. Excess abdominal fat predisposes individuals to metabolic syndrome, which is characterized by central obesity, abnormal blood sugar levels, elevated triglycerides, low HDL cholesterol, and hypertension.
- Cancer. Central obesity raises the risk of colon cancer in men and postmenopausal women, as well as breast cancer in women.
- Dementia. Research suggests that visceral fat in the abdomen is associated with an elevated risk of dementia, even among individuals with a normal body weight and no other significant risk factors.
Prevention
Maintaining a healthy and balanced lifestyle is key to preventing central obesity. Preventive measures include:
- Avoiding sweet and fatty foods, as well as simple carbohydrates. Focus on consuming fruits, vegetables, lean proteins, and complex carbohydrates.
- Reducing alcohol consumption.
- Increasing physical activity and regular exercise.
- Minimizing stress.
- Improving sleep quality.
- Quitting smoking.
When to See a Doctor?
Consult your doctor to determine a target weight that would improve your overall health. Begin with small, manageable goals to implement lasting changes in your diet, exercise routine, and stress management strategies.
Looking for more information about other diseases? Click here!
- dr. Monica Salim
Abdominal fat and what to do about it (2019) Harvard Health. Available at: https://www.health.harvard.edu/staying-healthy/abdominal-fat-and-what-to-do-about-it (Accessed: February 22, 2023).
Dr. Sruthi M., M.B.B.S. (2022) Why is abdominal obesity dangerous? how to reduce belly fat, MedicineNet. MedicineNet. Available at: https://www.medicinenet.com/why_is_abdominal_obesity_dangerous/article.htm (Accessed: February 22, 2023).
Dhawan, D. and Sharma, S. (2020) Abdominal obesity, adipokines and non-communicable diseases, The Journal of steroid biochemistry and molecular biology. U.S. National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7431389/ (Accessed: February 22, 2023).