Definisi
Bradikardia adalah perlambatan atau berkurangnya laju detak jantung. Jantung orang dewasa saat istirahat normalnya berdetak antara 60-100 kali per menit. Pada bradikardia, jantung berdetak <60 kali per menit.
Bradikardia bisa menjadi masalah serius jika detak jantung sangat lambat dan jantung tidak dapat memompa darah dengan cukup ke seluruh tubuh. Jika ini terjadi, Anda dapat merasa pusing, lemah, atau sesak nafas karena kekurangan oksigen.
Bradikardia dapat menimbulkan gejala ataupun tidak. Bradikardia yang bergejala disebut bradikardia simtomatik. Bradikardia juga ada yang menimbulkan komplikasi dan ada yang tidak.
Detak jantung yang lambat tidak selalu menjadi perhatian. Misalnya, detak jantung istirahat antara 40-60 denyut per menit cukup umum terjadi pada beberapa orang saat tidur, terutama orang dewasa muda yang sehat atau pada atlet terlatih.
Jika bradikardia tergolong berat, alat pacu jantung implan mungkin diperlukan untuk membantu jantung mempertahankan laju normalnya.
Penyebab
Bradikardia dapat disebabkan oleh:
- Kerusakan jaringan jantung akibat penuaan
- Kerusakan jaringan jantung akibat penyakit jantung atau serangan jantung
- Kelainan atau cacat jantung bawaan sejak lahir
- Peradangan jaringan jantung (miokarditis)
- Komplikasi operasi jantung
- Kelenjar tiroid yang kurang aktif (hipotiroidisme)
- Ketidakseimbangan bahan kimia (elektrolit) dalam darah, seperti kalium atau kalsium
- Jeda pernapasan yang berulang saat tidur (obstructive sleep apnea)
- Penyakit peradangan tubuh, seperti demam rematik atau lupus.
- Obat-obatan, termasuk obat penenang, opioid, dan obat-obatan yang digunakan untuk mengobati gangguan irama jantung, tekanan darah tinggi, serta gangguan kesehatan mental tertentu.
Untuk lebih memahami penyebab bradikardia, Anda perlu mengetahui bagaimana proses yang terjadi di dalam jantung hingga dapat berdetak. Jantung memiliki empat ruangan, yaitu 2 serambi (atrium) dan 2 bilik jantung (ventrikel).
Di dalam serambi kanan jantung (atrium kanan), terdapat sekelompok sel yang disebut sinus node. Nodus sinus adalah alat pacu jantung alami yang menghasilkan sinyal untuk memulai setiap detak jantung. Bradikardia terjadi ketika sinyal-sinyal ini melambat atau terhalang.
Masalah pada Sinus Node
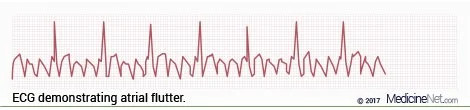
Bradikardia umumnya dimulai di area jantung yang disebut sinus node. Pada beberapa orang, sinus node yang bermasalah dapat menyebabkan denyut jantung lambat dan cepat (sindrom bradikardia-takikardia).
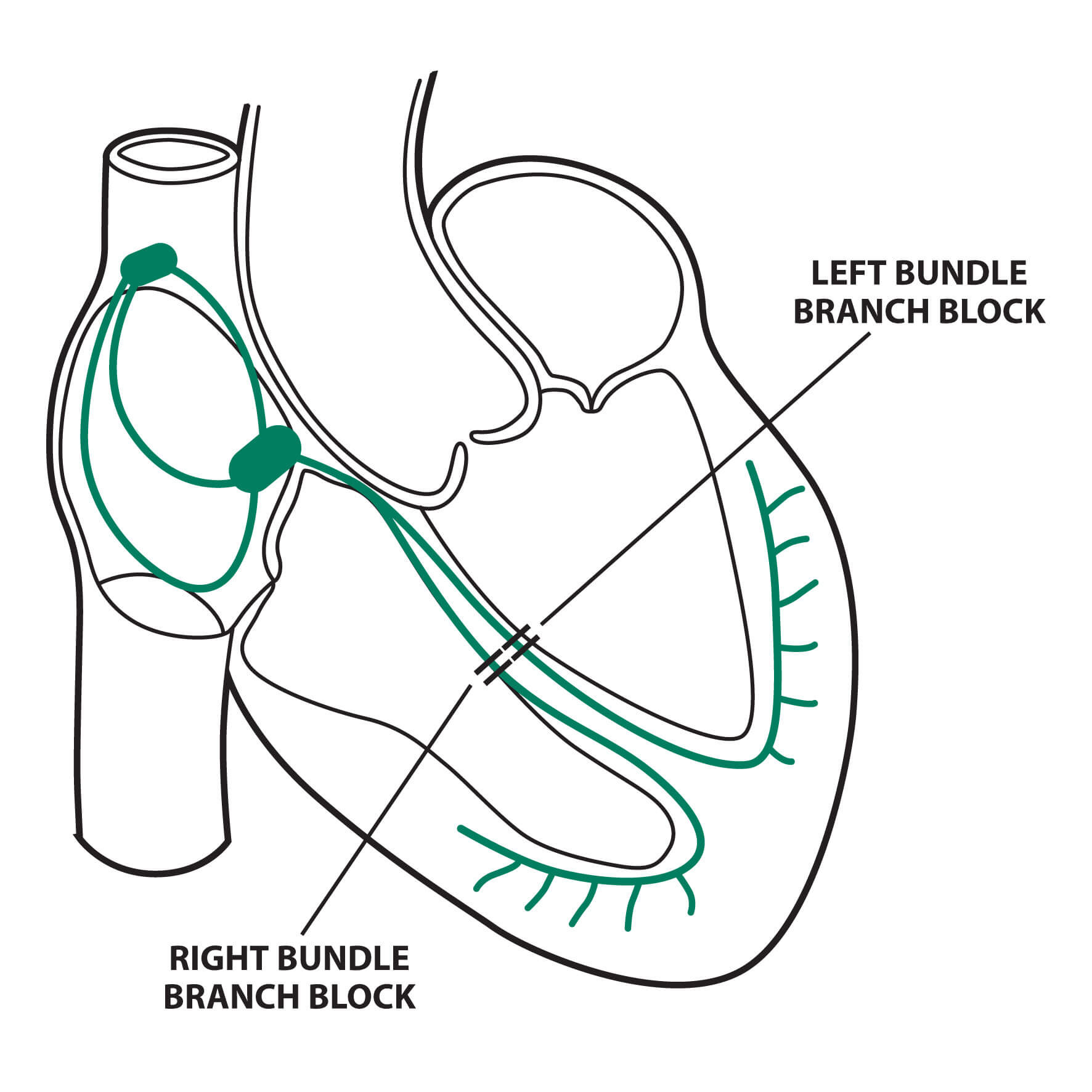
Blok Atrioventrikular (AV)
Bradikardia juga dapat terjadi ketika sinyal listrik jantung tidak bergerak dengan benar dari serambi ke bilik jantung. Jika ini terjadi, disebut blok jantung atau blok atrioventrikular.
Blok jantung terbagi menjadi tiga kelompok utama.
- Blok jantung derajat satu. Merupakan blok jantung yang paling ringan. Pada derajat ini, semua sinyal listrik dari serambi jantung dapat mencapai bilik jantung, namun sinyalnya lebih lambat. Blok jantung tingkat pertama jarang menimbulkan gejala dan biasanya tidak memerlukan pengobatan jika tidak ada masalah lain pada sinyal listrik
- Blok jantung derajat dua. Pada derajat dua, tidak semua sinyal listrik mencapai bilik jantung. Beberapa denyut melambat, menghasilkan irama jantung yang lebih lambat dan terkadang tidak teratur
- Blok jantung derajat ketiga (blok total). Pada derajat ini, tidak ada satupun sinyal listrik dari serambi jantung yang mencapai bilik jantung. Ketika ini terjadi, bilik jantung biasanya akan berdetak dengan sendirinya namun dengan kecepatan yang sangat lambat.
Faktor Risiko
Bradikardia berhubungan dengan kerusakan jaringan jantung pada beberapa jenis penyakit jantung. Apa pun yang meningkatkan risiko masalah jantung dapat meningkatkan risiko bradikardiaa. Faktor risiko penyakit jantung antara lain:
- Usia lanjut
- Tekanan darah tinggi
- Merokok
- Konsumsi alkohol berlebihan
- Penggunaan obat-obatan terlarang
- Stres dan kecemasan
Perubahan gaya hidup sehat atau perawatan medis yang sesuai dapat membantu menurunkan risiko penyakit jantung.
Gejala
Bradikardia atau detak jantung yang lebih lambat dari normal dapat membuat otak dan organ lain tidak mendapatkan cukup oksigen. Kondisi ini dapat menimbulkan beberapa tanda dan gejala berikut:
- Nyeri dada
- Kebingungan atau gangguan memori
- Pusing
- Mudah lelah saat melakukan aktivitas fisik
- Kelelahan
- Pingsan atau hampir pingsan
- Sesak nafas
Diagnosis
Untuk mendiagnosis bradikardia, dokter akan melakukan pemeriksaan fisik dan mendengarkan detak jantung dengan alat stetoskop. Dokter juga akan menanyakan gejala dan riwayat kesehatan Anda.
Dokter dapat merekomendasikan tes untuk memeriksa detak jantung dan melihat apakah Anda memiliki masalah jantung yang menyebabkan bradikardia. Tes darah dapat dilakukan untuk memeriksa kondisi lain yang menyebabkan perlambatan detak jantung, seperti infeksi, hipotiroidisme, atau ketidakseimbangan elektrolit.
Pemeriksaan
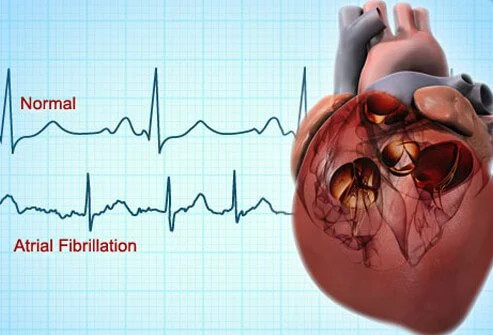
Elektrokardiogram atau EKG adalah tes utama untuk mendiagnosis bradikardia. EKG mengukur aktivitas listrik jantung. Elektroda atau suatu alat logam ditempelkan di dada, lengan, dan kaki. Kabel akan menghubungkan elektroda ke mesin EKG yang akan menampilkan hasil rekaman listrik jantung. EKG dapat menunjukkan apakah jantung berdetak terlalu lambat, terlalu cepat, atau tidak berdetak sama sekali.
Namun, EKG tidak dapat mendeteksi bradikardia kecuali bradikardia terjadi saat pemeriksaan. Oleh karena itu, dokter dapat merekomendasikan perangkat portabel, seperti:
- Monitor Holter. Alat ini bisa dimasukkan ke dalam saku atau dikenakan di ikat pinggang dan dibawa kemana-kemana. Alat ini merekam aktivitas jantung terus menerus selama 24 jam atau lebih.
- Event recorder. Alat ini mirip dengan monitor Holter, namun hanya merekam pada waktu tertentu selama beberapa menit sekali. Alat ini dipakai lebih lama dari monitor Holter, biasanya 30 hari. Ketika merasakan gejala, Anda perlu menekan sebuah tombol agar hasil rekaman listrik jantung Anda dapat ditampilkan. Beberapa alat secara otomatis akan merekam ketika mendeteksi adanya irama jantung yang tidak teratur
Pemeriksaan EKG dapat disertai dengan pemeriksaan lain untuk memahami bagaimana munculnya bradikardia pada jantung Anda. Tes ini meliputi:
- Tes meja miring. Tes ini membantu dokter untuk lebih memahami bagaimana bradikardia menyebabkan Anda pingsan. Saat Anda berbaring di meja khusus, meja dimiringkan seolah-olah Anda sedang berdiri. Tes kemiringan dilakukan untuk melihat apakah perubahan posisi menyebabkan pingsan
- Tes latihan stres. EKG dapat dilakukan untuk memantau aktivitas listrik jantung saat Anda mengendarai sepeda statis atau berjalan di atas treadmill. Jika Anda mengalami kesulitan berolahraga, obat tertentu dapat diberikan untuk merangsang kerja jantung, mirip dengan rangsangan yang ditimbulkan oleh olahraga
Sebuah sleep study dapat direkomendasikan jika dokter mencurigai adanya hubungan antara bradikardia dan obstructive sleep apnea.
Tata Laksana
Pengobatan bradikardia bergantung pada tingkat keparahan gejala dan penyebabnya. Jika bradikardia tidak menimbulkan gejala, pengobatan mungkin tidak diperlukan.
Penanganan bradikardia meliputi perubahan gaya hidup, pengobatan, atau pemasangan alat pacu jantung implan. Jika disebabkan oleh penyakit tertentu seperti penyakit tiroid atau sleep apnea, pengobatan pada penyakit-penyakit tersebut dapat memperbaiki bradikardia.
Obat-obatan
Banyak obat, termasuk yang digunakan untuk mengobati penyakit jantung lainnya, dapat menyebabkan bradikardia. Saat pemeriksaan, selalu beri tahu dokter tentang semua obat yang Anda minum, termasuk yang dibeli tanpa resep. Jika obat yang Anda minum menyebabkan bradikardia, dokter akan merekomendasikan dosis yang lebih rendah atau pilihan obat yang berbeda.
Pembedahan atau Prosedur Lain
Ketika pengobatan lain tidak memungkinkan dan gejala bradikardia memberat, diperlukan alat pacu jantung untuk mengontrol irama jantung. Alat pacu jantung bekerja hanya bila diperlukan. Ketika jantung berdetak terlalu lambat, alat pacu jantung akan mengirimkan sinyal listrik ke jantung untuk mempercepat detaknya.
Memasang alat pacu jantung memerlukan prosedur pembedahan. Beberapa kawat khusus dimasukkan ke dalam pembuluh darah vena besar di selangkangan dan dipandu menuju ke jantung menggunakan sinar-X. Salah satu ujung kawat diarahkan ke area yang sesuai di jantung, sementara ujung lainnya dipasang ke alat generator denyut jantung yang ditanam di bawah kulit selangkangan.
Komplikasi
Kemungkinan komplikasi bradikardia meliputi:
- Sering pingsan
- Gagal jantung atau ketidakmampuan jantung untuk memompa cukup darah ke seluruh tubuh
- Serangan jantung mendadak, atau
- Kematian mendadak
Pencegahan
Bradikardiaa dapat disebabkan oleh obat-obatan tertentu, terutama jika dikonsumsi dalam dosis yang berlebihan. Sehingga, minum obat harus sesuai dengan petunjuk dokter. Meskipun bradikardia umumnya tidak dapat dicegah, ada beberapa strategi untuk mengurangi risiko penyakit jantung, seperti:
- Olahraga teratur. Dokter akan merekomendasikan jadwal olahraga yang sesuai dengan kondisi Anda
- Makan makanan yang sehat. Pilih diet rendah lemak, rendah garam, rendah gula, kaya buah-buahan, sayuran, dan biji-bijian
- Pertahankan berat badan ideal. Kelebihan berat badan meningkatkan risiko terkena penyakit jantung
- Jaga tekanan darah dan kolesterol agar tetap terkendali. Lakukan perubahan gaya hidup dan minum obat sesuai resep dokter untuk mengelola tekanan darah tinggi, kadar gula darah, dan kolesterol tinggi
- Jangan merokok. Jika Anda memerlukan bantuan untuk berhenti merokok, konsultasi dengan dokter tentang strategi atau program yang sesuai
- Batasi konsumsi alkohol. Jika Anda tidak dapat mengontrol penggunaan alkohol, konsultasi dengan dokter tentang program berhenti minum dan mengelola perilaku lain yang terkait dengan penyalahgunaan alkohol
- Kelola stres. Emosi yang tidak terkontrol dapat mempengaruhi detak jantung. Beberapa cara untuk menghilangkan stres adalah dengan olahraga secara teratur, bergabung dengan kelompok pendukung, atau mencoba teknik relaksasi seperti yoga
- Rutin kontrol kesehatan. Kontrol ke dokter secara teratur dan laporkan jika ada tanda atau gejala baru pada dokter
Monitor dan Obati Penyakit Jantung
Jika Anda sudah memiliki penyakit jantung, ada beberapa cara untuk mengurangi risiko bradikardia atau gangguan irama jantung lainnya:
- Patuhi aturan pengobatan dokter. Pastikan Anda memahami rencana pengobatan yang diberikan dokter dan minum semua obat sesuai resep
- Laporkan perubahan segera. Jika gejala berubah, memburuk, atau muncul gejala baru, segera beritahu dokter
Kapan Harus ke Dokter?
Banyak hal yang dapat menyebabkan tanda dan gejala bradikardia. Sangat penting untuk mendapatkan diagnosis yang cepat, akurat, serta pengobatan yang tepat. Konsultasi ke dokter jika Anda memiliki gejala bradikardia.
Jika Anda pingsan, mengalami kesulitan bernapas, atau merasakan nyeri dada yang berlangsung lebih dari beberapa menit, hubungi nomor telepon darurat atau kunjungi unit gawat darurat untuk mendapatkan penanganan segera.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Anita Larasati Priyono
Bradycardia. (2021). Retrieved 29 March 2022, from https://www.mayoclinic.org/diseases-conditions/bradycardia/symptoms-causes/syc-20355474
Brouhard R. (2019). Symptomatic bradycardia in the field. Retrieved 29 March 2022, from https://www.verywellhealth.com/symptomatic-bradycardia-in-the-field-4144749
Hafeez Y, Grossman SA. (2021). Sinus bradycardia. Retrieved 29 March 2022, from https://www.ncbi.nlm.nih.gov/books/NBK493201/