Definition
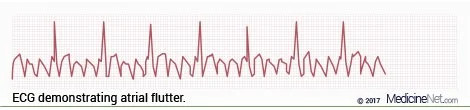
Atrial flutter (AFL) occurs when the heart's atria beat too fast, causing the heart to beat rapidly but irregularly. Atrial flutter is a heart rhythm disorder or arrhythmia caused by a malfunction in the heart's electrical system.
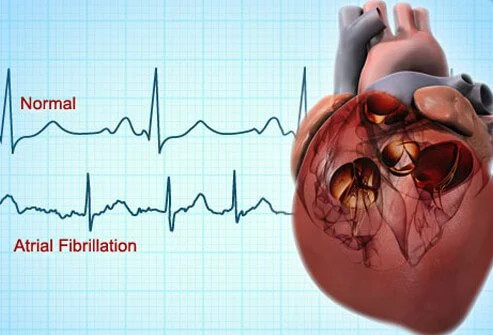
Atrial flutter is resembling to atrial fibrillation (AFib), a common disorder in which the heart beats irregularly. However, people with atrial flutter have a more consistent and less chaotic heart rhythm than those with atrial fibrillation. Atrial flutter and atrial fibrillation can occur at the same time.
People with atrial flutter may experience no symptoms. However, the disorder may increase the risk of stroke, heart failure, and other complications.
Causes
It is unclear what causes atrial flutter. The disorder is thought to be caused by damage to the heart, its electrical system, or other body parts that affect the heart.
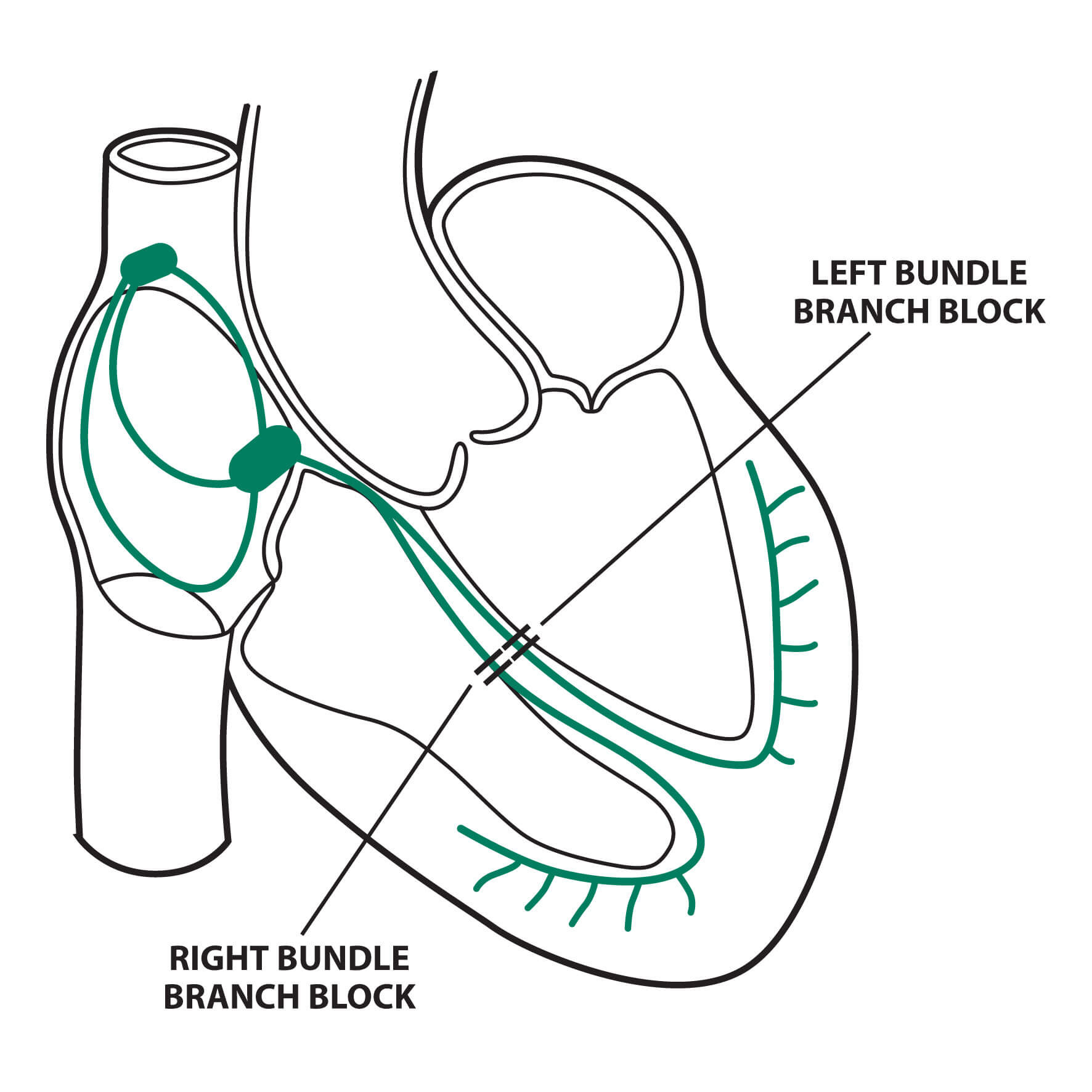
The sinoatrial node (SA node) is the natural pacemaker that controls the heartbeat. The SA node is located in the right foyer of the heart. The SA node sends electrical signals to the right and left atriums to tell the upper part of the heart how and when to contract.
When atrial flutter occurs, signals from the SA node move abnormally fast and continuously around the right atrium, causing the atriums to beat too quickly between 250 and 320 beats per minute (bpm) and the lower ventricles to beat at 150 bpm.
A normal resting heart rate ranges from 60 to 100 beats per minute, with the atriums and ventricles beating simultaneously. At this normal rate, the ventricles can pump blood throughout the body. Your heart rate can be measured by touching a large blood vessel in the neck or wrist, as well as using medical and smart devices.
Researchers have linked many factors to the onset of disruptions in the heart's electrical circuits that cause AFL. However, sometimes it is still difficult to pinpoint the exact cause.
Heart disorders
Certain heart diseases or disorders can be a major cause of AFL. For example:
- Scarring following heart surgery or cardiac ablation, which are non-surgical procedures to treat AFL and AFib
- Decreased blood flow to the heart (ischemia), usually due to hardening of the arteries (atherosclerosis) or blood clots
- High blood pressure
- Heart muscle disease or cardiomyopathy
- Heart valve abnormalities
- Enlargement of the heart chambers (hypertrophy or dilation)
- Heart attack
- Blood clot in the lungs
- Non-cardiac surgery
Other conditions
Disorders in other parts of the body that affect the heart can also play a role in the development of AFL. For example:
- Thyroid disease
- Blood clots in blood vessels
- Chronic lung diseases, such as chronic obstructive pulmonary disease (COPD) or emphysema
- Sleep apnea, where breathing stops briefly during sleep, which is left untreated
Lifestyle
Lifestyle factors may also play a role in the development of AFL. This is often related to the consumption of substances that can affect the heart's electrical system, such as:
- Alcohol abuse
- Substance and drug abuse, especially stimulants
- Smoking
- Consumption of certain medications, such as diet pills or cold medications
- Consumption of high amounts of caffeine
Risk Factor
Some of the following conditions may increase the risk of AFL, such as:
- Age 50 years or older
- High blood pressure
- Coronary heart disease
- Congenital heart disease
- History of previous heart attack
- Heart surgery
- Lung disease
- Thyroid disease
- Chronic (long-term) stress or anxiety
- Smoking
- Diabetes
- Certain medications, such as cold medicines or diet pills
- Alcohol or other illicit substance abuse
- Untreated sleep apnea, which can cause dilation of the heart chambers
Symptoms
The symptoms of AFL are extensive and may last for hours, days, or even weeks. Symptoms include:
- Rapid but steady pulse
- Shortness of breath
- Dizziness or feeling like you are going to pass out
- Chest feels compressed or constricted
- Dizziness
- Heart palpitations
- Fatigue that prevents you from doing your daily activities
These symptoms may be similar to other heart conditions or conditions unrelated to the heart. However, exhibiting one or more of these symptoms is not always indicative of AFL. Some people with AFL experience no symptoms at all. Because it is difficult to diagnose AFL, always consult your doctor if you experience any of the symptoms listed above.
Diagnosis
Doctors start considering the diagnosis of AFL if the resting heart rate is above 120 bpm and if the ECG shows atrial flutter waves. Family history is important for diagnosing AFL. A history of heart disease, anxiety, or high blood pressure may increase your risk. The doctor can make an initial diagnosis of AFL with an ECG. You may also be referred to a cardiologist for further examination.
Some of the tests used to diagnose and confirm AFL are:
- ECG can measure blood flow through the heart and blood vessels and see if the heart has shown signs of weakness due to rapid beating, such as cardiomyopathy triggered by tachycardia or a condition of dilated atriums
- ECG to record the heart's electrical patterns
- Holter monitor to monitor the heart rhythm for 24 hours
- Electrophysiology (EP) study to record the heart rhythm. A tube is inserted through a blood vessel in the groin into the heart. A special device is then inserted into the heart to monitor the heart rhythm in several different areas
Management
The main goal of treatment is to restore normal heart rhythm. Treatment depends on the severity of the condition and response to medications. The underlying disease can have an impact on the treatment of AFL and must also be treated.
Medicines
Medicines can slow or regulate the heart rate. Examples of medications include:
- Calcium channel blockers
- Beta-blockers
- Digoxin
Certain medications may require hospitalization for administration, such as antiarrhythmic drugs.
Other medications may be used to change the rhythm of atrial flutter back to normal, such as amiodarone, propafenone, and flecainide. Blood thinners, such as non-vitamin K tablet anticoagulants (DOACs), may be used to prevent clots from forming in the arteries. Blood clots can lead to a stroke or heart attack.
People with AFL have a higher risk of blood clots. Blood thinning treatment depends on age, gender, and other risk factors, which are assessed using the CHA2DS2-Vasc scoring system.
Warfarin was previously the most frequently prescribed anticoagulant. DOACs are now preferred because they do not require frequent blood test monitoring and have no food interactions.
Surgery
Ablation therapy inhibits the heart tissue that is causing the abnormal rhythm. This technique is used when AFL cannot be controlled with medication or when medication has side effects. However, it is increasingly being used as a first-line treatment for atrial flutter.
Alternative Therapy
Cardioversion using electricity to shock the heart rhythm back to normal is used to reset the heart rhythm and eliminate atrial flutter. After anesthesia has been administered, electrodes are placed on specific areas of the chest to deliver an electric shock.
Complications
Atrial flutter occurs when the heart does not pump blood properly. When blood flow slows, blood clots can form easily. If a clot makes its way to a blood vessel in the brain and blocks it, it can cause a stroke.
A fast heartbeat also weakens the heart muscle over time. This can result in heart failure if the heart is unable to pump enough blood throughout the body.
However, if you don't have other heart issues, your condition is generally quite good. If atrial flutter occurs once without any serious heart or lung disease, you may never have it again. If you have other heart conditions, atrial flutter may return. If that happens, you should consult a heart specialist immediately.
Prevention
Prevention of atrial flutter is to control and prevent modifiable risk factors, such as:
- Maintaining an ideal body weight
- Limiting alcohol consumption
- Quitting smoking
- Controlling blood pressure and blood sugar
When to See a Doctor?
Consult with a doctor if you:
- Have any of the symptoms of atrial flutter
- Are taking atrial flutter medication and have any of the signs and symptoms described above
If you have been diagnosed and are being treated for atrial flutter, visit a hospital emergency department immediately if you:
- Have severe chest pain
- Feel lightheaded
- Faint
Looking for more information about other diseases? Check here, yes!
- dr Anita Larasati Priyono
Lamoreux K. (2021). Atrial flutter. Retrieved 29 March 2022, from https://www.healthline.com/health/heart-disease/atrial-flutter
Atrial flutter. (2020). Retrieved 29 March 2022, from https://www.mayoclinic.org/diseases-conditions/atrial-flutter/symptoms-causes/syc-20352586
Rosenthal L. (2019). Atrial flutter. Retrieved 29 March 2022, from https://emedicine.medscape.com/article/151210-overview
Atrial flutter. (2020). Retrieved 29 March 2022, from https://www.webmd.com/heart-disease/atrial-fibrillation/atrial-flutter#091e9c5e8000ae91-6-24