Definition
Cyanosis is a medical condition typically characterized by bluish skin and mucous membrane discoloration. This color change is due to an oxygen deficiency and poor blood circulation. Blood sufficiently oxygenated appears bright red, whereas, when lacking oxygen, it takes on a dark purplish or bluish hue. Cyanosis often indicates an underlying disorder or disease, such as lung or heart disease.
Cyanosis can be divided into two types: central and peripheral. Central cyanosis specifically affects individuals with heart or lung disease and certain blood disorders, such as Methemoglobinemia and Sulfhemoglobinemia. The primary sign of central cyanosis is a bluish tint on the tongue and lips. In central cyanosis, the bluish discoloration is generally observed throughout the body and mucous membranes. In contrast, peripheral cyanosis appears on the hands, fingertips, toes, and sometimes around the mouth.
Causes
Under normal conditions, red blood cells transport most of the oxygen in the blood. Hemoglobin (a substance in red blood cells that binds with oxygen) releases oxygen into tissues, turning darker in color. Deoxygenated blood is carried back to the lungs to be replenished with fresh oxygen from breathing and then returned to the heart to be pumped out to the rest of the body.
Central cyanosis becomes visible on the tongue and lips when the level of deoxygenated blood reaches between 4 to 6 mg/dL due to heart and respiratory disorders that hinder the exchange of oxygen and red blood cells in the lungs or the blood flow in the heart. This blood appears bluish or purplish on the skin and mucous membranes.
The causes of central cyanosis can be divided into two categories:
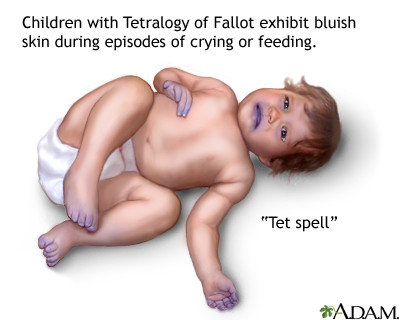
Central cyanosis in newborns
The causes of central cyanosis in newborns include heart and respiratory system disorders. Some heart disorders (due to low oxygen levels in the blood) that cause central cyanosis in newborns are:
- Transposition of the great arteries (TGA)
- Tetralogy of Fallot
- Atrial septal defect (a hole between the left and right atria of the heart)
- Pulmonary or tricuspid valve stenosis/atresia (a valve in the heart that is narrowed or absent)
- Truncus arteriosus (a single large artery leaving the heart that branches into the pulmonary artery and aorta)
- Hypoplastic left heart syndrome
- Persistent fetal circulation (a condition where blood continues to flow through a structure that should close after birth)
Several respiratory system disorders that impede the exchange of oxygen and blood in the lungs, leading to central cyanosis in newborns, include:
- Respiratory distress syndrome
- Birth injury/asphyxia
- Pneumothorax (air in the pleural cavity, the lining around the lungs)
- Meconium aspiration (inhalation of stool during birth)
- Pleural effusion (fluid in the lining around the lungs)
- Pulmonary edema (swelling of the lungs due to excess fluid)
- Upper airway obstruction
Other causes of central cyanosis in newborns include:
- Infection
- Seizures
- Metabolic disorders, such as hypoglycemia, hypomagnesemia
Central cyanosis in adults
In adults, central cyanosis can be caused by conditions such as:
- Pulmonary embolism (a blockage in the pulmonary artery often caused by a blood clot)
- Pulmonary edema
- Severe pneumonia (lung infection)
- Chronic obstructive pulmonary disease (COPD)
- Acute respiratory distress syndrome
- Severe acute asthma
- Hemoglobin disorders preventing sufficient oxygen transport, such as:
- Methemoglobinemia, possibly genetic or associated with certain medications, e.g., quinones, primaquine, sulfonamides.
- Sulfhemoglobinemia, often linked to specific medications, mainly sulfonamides.
- Polycythemia vera (excess red blood cells)
Risk factor
In newborns, the risk of central cyanosis increases with severe airway, respiratory system, or heart and circulatory disorders. Congenital heart defects in newborns also heighten the risk of central cyanosis. These heart defects commonly occur if the baby has genetic disorders such as Down syndrome, Turner syndrome, Marfan syndrome, Noonan syndrome, etc. Congenital heart defects may also be found in babies whose mothers had infections during pregnancy, such as measles or rubella. Women with diabetes during pregnancy and those who take certain medications during pregnancy are at higher risk of giving birth to babies with congenital heart defects.
In adults, the risk of developing central cyanosis rises with underlying conditions such as lung, heart, and hemoglobin disorders.
Symptoms
The most common symptom of central cyanosis is a bluish discoloration of the tongue and lips. Central cyanosis can also accompany other symptoms affecting the heart or respiratory system, including:
- Chest pain
- Breathing difficulties
- Leaning forward while sitting to breathe more easily
- Rapid or labored breathing
- Use of rib muscles to facilitate easier breathing
Central cyanosis may also present with symptoms related to other bodily systems, including:
Confusion or transient loss of consciousness
- Fever
- Irritability
- poor appetite
- and difficulty sleeping in infants and young children
- Lethargy or weakness
- Frequent headaches
Diagnosis
In emergencies, a doctor may need to stabilize the patient before further examination. The doctor will start by interviewing the patient or their family to diagnose central cyanosis. The doctor will inquire about the symptoms experienced, their duration, and the patient's comprehensive medical history, including past illnesses and previous treatments. Next, the doctor will conduct a physical examination focusing on the heart and lungs. The doctor will listen to these organs using a stethoscope and may examine the chest, abdomen, neck, and extremities. A pulse oximeter might be placed on a fingertip to measure the blood's oxygen saturation levels. The clinical presentation of a bluish tint on the lips and tongue may readily recognize Central cyanosis. However, additional tests may be necessary to identify the underlying cause of central cyanosis. These tests may include:
- Arterial blood gas analysis, to measure oxygen saturation and other signs of lung function.
- Blood tests, including a complete blood count and autoimmune tests.
- CHhest X-ray or other chest imaging, such as a CT scan (Computed Tomography).
- Cardiac tests, including an EKG (electrocardiogram) and an echocardiogram, which is an ultrasound.
- Pulmonary function tests and possibly a bronchoscopy, a test that uses an endoscope (a lighted tube inserted into the airway) to look at the inside of the lungs and airways.
Management
Fundamentally, central cyanosis is a symptom of another disease or condition, so its treatment depends on the underlying cause. The first step in treating central cyanosis is to provide supplemental oxygen to address low blood oxygen levels. Then, the doctor will identify the cause and administer appropriate treatment.
Complications
Central cyanosis can be caused by a serious disease or disorder, so delays in treatment can result in severe complications and permanent damage, such as heart failure and respiratory failure.
Prevention
Some causes of central cyanosis are difficult to prevent. However, you can take the following steps to reduce the risk of cyanosis and the conditions that cause it:
Protect your heart, blood vessels, and respiratory system by avoiding smoking and exercising regularly. Schedule routine check-ups with your doctor to monitor your health and report any changes. Follow your doctor's recommended care plan for any health conditions you have, such as diabetes, heart disease, asthma, or COPD. Pregnant women can undergo prenatal echocardiography (before the baby is born) and genetic testing to detect congenital heart disease in the baby. Administering corticosteroids before birth can also prevent respiratory distress syndrome in newborns.
When to see a doctor?
Consult your doctor immediately if you or your child experiences a bluish discoloration of the lips and tongue. This condition may indicate a more serious underlying disease or disorder.
Looking for more information about other diseases? Click here!
- dr Anita Larasati Priyono
Bharati, Kaushik. Cyanosis. (2018). Retrieved 1 April 2022, from https://www.medindia.net/patientinfo/cyanosis.htm#overview
Burke, Daria. What You Should Know About Discoloration of Skin. (2019). Retrieved 1 April 2022, from https://www.healthline.com/health/skin-discoloration-bluish
Cashin-Garbutt, April. Causes of Cyanosis. (2021). Retrieved 1 April 2022, from https://www.news-medical.net/health/Causes-of-cyanosis.aspx
Central Cyanosis. Retrieved 1 April 2022, from https://www.apollohospitals.com/central-cyanosis/
Knott, Laurence. Cyanosis. (2020). Retrieved 1 April 2022, from https://patient.info/doctor/cyanosis
Lloyd, William C. Cyanosis. (2021). Retrieved 1 April 2022, from https://www.healthgrades.com/right-care/symptoms-and-conditions/cyanosis
Pahal, Parul, et al. Central and Peripheral Cyanosis. (2021). Retrieved 1 April 2022, from https://www.ncbi.nlm.nih.gov/books/NBK559167/