Definisi
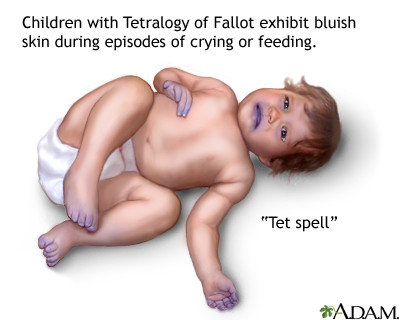
Spell hypoxic merupakan suatu kondisi di mana kulit anak menjadi sedikit biru dalam suatu periode waktu yang singkat. Spell hypoxic juga dikenal dengan beberapa istilah lain, yaitu tet spell, hypercyanotic spell, cyanotic spell, atau paroxysmal dyspnea. Kondisi biru pada kulit dikarenakan menurunnya kadar oksigen dalam darah secara cepat (hipoksia) akibat penurunan aliran darah ke paru-paru. Keadaan ini biasanya berlangsung selama kurang dari satu menit. Spell hypoxic paling sering terlihat pada anak yang berusia kurang dari 2 tahun (lebih sering pada usia 2 sampai 4 bulan), terutama pada saat setelah bangun di pagi hari dan setelah menangis, dan sangat jarang terjadi pada orang dewasa. Pada kasus-kasus tertentu, spell hypoxic dapat hilang dengan sendirinya tanpa intervensi apapun (self-limiting).
Spell hypoxic biasanya disebabkan oleh suatu penyakit jantung bawaan yang mendasarinya, yang tersering disebabkan oleh Tetralogy of Fallot (sehingga disebut juga sebagai Tet Spell). Tetralogy of Fallot merupakan suatu kelainan jantung bawaan yang cukup langka. Pada kelainan ini ditemukan kombinasi dari empat kelainan struktur jantung, yaitu ventrikel septal defek (adanya lubang pada dinding yang memisahkan bilik jantung kiri dan kanan) yang besar, sumbatan pada katup pulmonal (katup yang memisahkan bilik kanan jantung dan pembuluh darah arteri pulmonal), hipertrofi (pembesaran) bilik jantung kanan, dan overiding aorta (perubahan posisi pembuluh darah aorta).
Penyebab
Spell hypoxic terjadi ketika aliran darah ke paru-paru berkurang secara tiba-tiba. Aliran darah ke paru-paru yang berkurang mengakibatkan semakin sedikit oksigen yang terdapat di dalam darah. Darah yang memiliki banyak kandungan oksigen akan tampak berwarna merah cerah, sedangkan darah dengan kandungan oksigen yang sedikit akan tampak berwarna lebih gelap dan berwarna kebiruan. Darah dengan kadar oksigen yang lebih sedikit inilah yang menyebabkan kulit menjadi berwarna kebiruan. Mekanisme pasti dari terjadinya penurunan aliran darah ke paru-paru secara tiba-tiba pada spell hypoxic belum diketahui dengan jelas. Akan tetapi, diduga terdapat beberapa pencetus yang dapat menyebabkan menurunnya aliran darah ke paru-paru sehingga menimbulkan spell hypoxic, antara lain:
- Menangis
- Buang air besar
- Bangun dari tidur
- Minum ASI atau susu
- Demam
- Mandi
- Keadaan stres atau sangat cemas
- Dehidrasi (kekurangan cairan)
- Denyut nadi yang cepat
- Penggunaan obat-obat tertentu, seperti golongan ACE-inhibitor
Faktor Risiko
Faktor risiko utama dari timbulnya spell hypoxic adalah memiliki penyakit jantung bawaan yang mendasarinya. Kelainan jantung bawaan yang paling sering berhubungan dengan timbulnya spell hypoxic adalah menderita Tetralogy of Fallot. Beberapa faktor yang dapat meningkatkan risiko bayi Anda menderita Tetralogy of Fallot, antara lain:
- Terdapat riwayat infeksi virus selama kehamilan, seperti Rubella (campak Jerman)
- Kebiasaan minum alkohol selama kehamilan
- Memiliki keadaan gizi yang buruk selama kehamilan
- Wanita hamil dengan usia lebih dari 40 tahun
- Riwayat orang tua yang memiliki Tetralogy of Fallot
- Terdapat sindrom Down atau sindrom DiGeorge pada bayi
Selain Tetralogy of Fallot, risiko terjadinya spell hypoxic juga dapat meningkat pada beberapa kelainan jantung lainnya, seperti:
- Double outlet right ventricle dengan stenosis katup pulmonal (pembuluh darah aorta dan paru keluar dari bilik kanan)
- Atresia katup pulmonal dengan ventrikel septal defek (tidak berkembangnya katup di paru disertai kelainan pada bilik jantung)
- Atresia trikuspid dengan stenosis pulmonal (tidak berkembangnya katup trikuspid disertai kelainan pada pembuluh darah paru)
- Transposition of great arteries dengan ventrikel septal defek dan stenosis pulmonal (kelainan kongenital dimana terjadi pemindahan tempat pembuluh darah aorta dan paru)
Gejala
Gejala-gejala yang mungkin ditemukan pada spell hypoxic, antara lain:
- Bernapas lebih cepat dan lebih dalam.
- Tampak perubahan menjadi kebiruan, terutama pada area bibir, mulut, wajah dan kuku (sianosis).
- Tampak rewel, panik, gelisah, atau terlihat tidak nyaman.
- Periode menangis yang panjang.
- Pingsan
- Penurunan intensitas atau hilangnya bising jantung (murmur),
Diagnosis
Spell hypoxic termasuk kasus gawat darurat yang perlu penanganan segera. Dokter mungkin akan melakukan pemeriksaan secara lebih lengkap setelah kondisi penderita stabil dan telah mendapat pertolongan pertama. Spell hypoxic cukup mudah dikenali melalui tampilan klinisnya.
Dalam mendiagnosis spell hypoxic, dokter akan melakukan wawancara untuk menanyakan gejala-gejala yang dialami, serta riwayat penyakit sebelumnya yang pernah diderita, khususnya riwayat penyakit jantung bawaan dan riwayat bayi saat lahir (apakah langsung menangis, apakah bayi tampak biru). Dokter juga akan melakukan pemeriksaan fisik secara menyeluruh, seperti memeriksa area tubuh yang mengalami perubahan warna menjadi kebiruan, dan mendengarkan bunyi jantung dengan menggunakan stetoskop. Seringkali, dokter akan melakukan pemeriksaan lanjutan untuk mencari penyakit jantung yang mendasari timbulnya spell hypoxic, di mana penyebab terseringnya adalah Tetralogy of Falllot. Beberapa pemeriksaan penunjang yang mungkin disarankan dokter, antara lain:
- Pengukuran kadar oksigen (pulse oksimetri) dengan menggunakan sebuah sensor kecil yang ditempatkan pada jari tangan atau kaki untuk mengukur kadar oksigen dalam darah.
- Ekokardiogram dengan menggunakan gelombang suara untuk menunjukkan gambar jantung yang sedang bergerak. Ekokardiogram dapat menunjukkan struktur, letak, dan fungsi dinding jantung, bilik jantung, katup jantung dan paru, serta pembuluh darah aorta.
- Elektrokardiogram (EKG) untuk merekam aktivitas listrik di jantung setiap kali berkontraksi. Selama prosedur ini, kabel dan elektroda akan ditempatkan di dada, pergelangan tangan, dan pergelangan kaki. EKG dapat membantu menentukan apakah ruang jantung membesar dan apakah ada detak jantung yang tidak normal (aritmia).
- Rontgen dada dapat menunjukkan struktur jantung dan paru-paru. Tanda umum Tetralogi of Fallot pada rontgen adalah jantung berbentuk seperti sepatu bot, karena bilik jantung kanan yang membesar.
- Kateterisasi jantung. Dokter dapat menggunakan tes ini untuk mengevaluasi struktur jantung dan merencanakan perawatan bedah. Selama prosedur ini, dokter akan memasukkan sebuah tabung tipis yang fleksibel (kateter) ke dalam pembuluh darah, biasanya di selangkangan, dan diarahkan ke jantung. Zat pewarna juga bisa dialirkan melalui kateter untuk membuat struktur jantung lebih mudah dilihat pada sinar-X. Dokter dapat mengukur tekanan dan kadar oksigen di ruang jantung dan pembuluh darah selama prosedur ini.
Tata Laksana
Spell hypoxic merupakan suatu kondisi yang membutuhkan penanganan segera untuk mencegah timbulnya komplikasi. Spell hypoxic mungkin termasuk keadaan yang menakutkan bagi anak-anak dan orang tua mereka, tetapi biasanya hanya berlangsung kurang dari 1 menit. Jika anak Anda menunjukkan gejala spell hypoxic, maka Anda dapat melakukan beberapa hal di bawah ini:
- Tetap tenang, jangan panik.
- Miringkan anak Anda ke samping atau ke belakang.
- Angkat lutut anak hingga menyentuh dada (knee-chest-position).
- Beberapa anak akan secara refleks berjongkok ketika terjadi spell hypoxic. Hal ini termasuk cara anak-anak melakukan knee-chest-position.
- Tenangkan anak Anda dengan menyentuh atau memeluknya.
- Pastikan Anda dapat melihat wajah anak Anda agar dapat memperhatikan:
- Perubahan warna kulit
- Seberapa sadar anak Anda
- Berapa lama keadaan tersebut bertahan
Jika langkah-langkah awal tersebut tidak menunjukkan perbaikan, dokter mungkin akan memberikan obat-obatan, cairan infus, dan bahkan pembedahan. Selain mengatasi spell hypoxic, dokter juga akan menyarankan untuk mengobati penyakit jantung bawaan yang mendasari timbulnya spell hypoxic.
Komplikasi
Jika tidak ditatalaksana tepat waktu, spell hypoxic dapat menyebabkan timbulnya komplikasi, seperti kelumpuhan, kejang, gangguan saraf, dan bahkan kematian.
Pencegahan
Belum diketahui cara pasti untuk mencegah timbulnya spell hypoxic. Namun, risiko spell hypoxic dapat diturunkan dengan mengontrol dan mengatasi penyakit jantung bawaan yang menjadi penyebab dasarnya. Selain itu, disarankan juga untuk menghindari kondisi-kondisi yang dapat mencetuskan timbulnya spell hypoxic.
Kapan Harus ke Dokter ?
Lakukan langkah-langkah penanganan awal jika anak Anda mengalami spell hypoxic. Jika belum terjadi perbaikan, segera bawa anak Anda ke Instalasi Gawat Darurat (IGD) untuk mendapatkan pertolongan lanjutan.
- dr Nadia Opmalina
Beerman, Lee B. Tetralogy of Fallot. (2020). Retrieved 9 April 2022, from https://www.msdmanuals.com/professional/pediatrics/congenital-cardiovascular-anomalies/tetralogy-of-fallot
Gawalkar, Atit A., et al. Management of Tet Spell – An Updated Review. (2021). Currenr Research in Emergency Medicine (CREM), Vol. I, Issue I.
Gentles, Tom, et al. Tetralogy of Fallot. Retrieved 9 April 2022, from https://starship.org.nz/guidelines/tetralogy-of-fallot/
Hypercyanotic Spells. (2021). Retrieved 9 April 2022, from https://pch.health.wa.gov.au/For-health-professionals/Emergency-Department-Guidelines/Hypercyanotic-spells
Song, Ho Young, et al. A 75-Year-Old Natural Survivor with Uncorrected Tetralogy of Fallot Presenting with Hypoxic Spell. (2017). Retrieved 9 April 2022, from https://doi.org/10.12771/emj.2017.40.2.94
Tetralogy of Fallot. (2021). Retrieved 9 April 2022, from https://www.mayoclinic.org/diseases-conditions/tetralogy-of-fallot/symptoms-causes/syc-20353477