Definisi
Hifema adalah suatu kondisi berupa berkumpulnya darah pada bola mata bagian depan. Angka kejadian hifema akibat trauma sekitar 12 kejadian pada 100.000 orang, dan 70% di antaranya dialami oleh anak-anak. Pada umumnya, hifema ditemukan pada laki-laki berusia 10-20 tahun dan terjadi akibat hantaman depan bola mata saat berolahraga dengan bola, seperti basket, sepakbola, bisbol, dan sebagainya.
Penyebab
Penyebab hifema pada umumnya adalah trauma, baik trauma tumpul atau gores. Trauma tumpul biasanya disebabkan oleh hantaman langsung ke bola mata bagian depan. Hantaman ini dapat melukai selaput pelangi/iris serta struktur di sekitarnya, termasuk pembuluh darah. Pembuluh darah yang pecah akan menyebabkan darah berkumpul pada ruang di bola mata bagian depan. Selain bola, benda lain yang berpotensi menyebabkan hifema adalah batu, mainan tembak-tembakan, peluru pada permainan paintball, kok bulutangkis, pembuka botol, serta tonjokan tangan. Selain itu, hifema dapat terjadi pascaoperasi. Misalnya, pada pasca operasi katarak, jika lensa buatan salah letak, dapat terbentuk pembuluh darah baru pada selaput pelangi yang mudah pecah. Operasi dengan laser dapat pula berefek samping hifema.
Hifema juga dapat terjadi secara spontan. Biasanya, hifema ini terjadi sebagai akibat dari pembentukan pembuluh darah baru pada mata seperti pada diabetes, tumor pada mata, peradangan pada lapisan bola mata (uveitis), serta kelainan struktur pembuluh darah.
Faktor Risiko
Faktor risiko hifema adalah aktivitas seperti olahraga yang dilakukan pada pelindung mata. Selain itu, riwayat operasi pada mata dapat pula meningkatkan risiko hifema hingga 7 hari setelah operasi. Ada pula beberapa penyakit yang meningkatkan risiko hifema spontan, yang pada umumnya adalah gangguan pembekuan darah seperti hemofilia, penyakit von Willebrand, serta penyakit sel sabit. Keganasan pada darah seperti leukemia juga dapat menjadi faktor risiko. Pengobatan untuk mengencerkan darah, misalnya pada pasien dengan riwayat pemasangan stent pada jantung atau stroke, dapat pula menjadi faktor risiko hifema.
Gejala
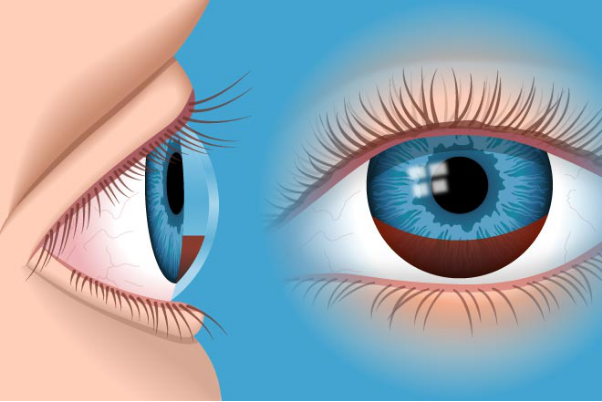
Gejala hifema secara umum adalah mata merah. Gangguan penglihatan dapat terjadi jika darah yang berkumpul menutupi pupil atau lubang hitam pada bagian tengah mata. Gangguan penglihatan yang dikeluhkan biasanya berupa blur, distorsi benda, atau sensitif terhadap cahaya. Selain gejala tersebut, keluhan nyeri juga dapat muncul terutama apabila tekanan bola mata meningkat.
Diagnosis
Diagnosis hifema dapat ditegakkan oleh dokter. Dokter dapat menanyakan riwayat trauma, operasi, riwayat pengobatan, serta riwayat perdarahan spontan sebelumnya. Jika hifema disebabkan oleh trauma, dokter akan memprioritaskan untuk mengamankan Anda terlebih dahulu serta memeriksa kemungkinan adanya trauma pada bagian tubuh lainnya. Pemeriksaan yang dapat dilakukan untuk menegakkan diagnosis hifema dapat dilakukan secara langsung oleh dokter, dan seringkali tidak membutuhkan pemeriksaan laboratorium.
Jika hifema disebabkan oleh trauma, dokter akan memastikan terlebih dahulu bahwa cedera yang terjadi bukan berupa cedera bola mata terbuka dengan pengecekan bola mata dan kulit sekitar mata. Selanjutnya, dokter akan melakukan pemeriksaan tajam penglihatan, pemeriksaan refleks cahaya pada mata, dan tekanan bola mata. Pemeriksaan ini, selain merupakan pemeriksaan rutin pada mata, berfungsi untuk menilai besarnya gangguan penglihatan yang disebabkan oleh hifema. Jika tekanan bola mata tinggi, kemungkinan terdapat gangguan pada aliran cairan di bola mata bagian depan. Oleh karena itu, jika Anda ke dokter spesialis mata, Anda dapat diperiksakan gonioskopi, untuk melihat sudut bola mata serta jaring-jaring yang berfungsi untuk mengeluarkan cairan pada bola mata bagian depan. Selain itu, dokter akan melakukan pemeriksaan dengan slit lamp atau funduskopi untuk menentukan derajat hifema, serta melihat ke bagian dalam bola mata, apabila penyebab hifema dicurigai akibat pembentukan pembuluh darah baru.
Derajat hifema terbagi menjadi empat:
- Derajat I: darah menutupi kurang dari sepertiga ruang depan bola mata
- Derajat II: darah menutupi sepertiga hingga setengah ruang depan bola mata
- Derajat III: darah menutupi ruang depan bola mata, lebih dari setengah namun tidak penuh
- Derajat IV: darah menutupi ruang depan bola mata penuh
Semakin tinggi derajat hifema, semakin tinggi pula kemungkinannya tekanan bola mata meningkat.
Jika Anda dicurigai memiliki kondisi yang menyebabkan hifema spontan, Anda dapat dirujuk untuk pemeriksaan laboratorium. Pemeriksaan biasanya dapat berupa faktor pembekuan darah untuk mengecek adanya hemofilia atau penyakit von Willebrand, serta pemeriksaan apus darah tepi untuk melihat adanya sel darah yang berbentuk seperti bulan sabit seperti pada penyakit sel sabit. Sementara itu, jika Anda mengalami hifema akibat trauma, dokter dapat menyarankan pemeriksaan CT scan untuk mencari adanya patah tulang wajah atau cedera pada otak yang mungkin terjadi bersamaan dengan hifema.
Tata Laksana
Hifema tanpa komplikasi biasanya dapat ditangani tanpa obat-obatan. Penggunaan pelindung mata diperlukan agar mata yang terkena hifema tidak mengalami trauma yang dapat memperparah hifema. Selain itu, pembatasan aktivitas dan menjaga kepala agar selalu tegak (minimal 45 derajat) dapat mengendapkan hifema pada bagian bawah bola mata. Hal ini diperlukan agar penglihatan tidak terganggu, karena pada umumnya posisi terlentang memperparah gangguan penglihatan akibat hifema. Pemantauan juga akan dilakukan selama beberapa hari pertama karena tingginya angka perdarahan ulang.
Selain itu, dokter dapat memberikan terapi terkait gejala. Jika terdapat nyeri, dokter akan memberikan obat antinyeri, namun perlu diperhatikan bahwa orang dengan hifema memiliki risiko perdarahan ulang yang dapat meningkat akibat obat-obatan antinyeri tertentu. Jika sensitivitas terhadap cahaya terlalu parah, dokter dapat memberikan obat tetes mata untuk melemaskan otot-otot di dalam mata. Jika tekanan bola mata meningkat, dokter dapat memberikan obat-obatan tetes mata untuk menurunkan tekanan bola mata.
Dari seluruh kejadian hifema, hanya 5% yang membutuhkan operasi. Operasi ini biasanya dilakukan jika hifema tidak segera membaik atau terdapat komplikasi. Namun, pada orang dengan penyakit sel sabit, jika tekanan bola mata tetap tinggi setelah 24 jam, operasi harus segera dilakukan.
Komplikasi
Komplikasi hifema terkait dengan struktur di bola mata bagian depan. Jika jaring-jaring yang mengalirkan cairan rusak akibat trauma, tekanan dalam bola mata dapat meningkat. Selain itu, jika trauma mempengaruhi selaput pelangi atau lensa mata, dapat terjadi penempelan yang tidak diinginkan. Hal ini dapat mempersulit otot mata untuk mengatur cahaya yang masuk. Perdarahan ulang juga dapat menjadi komplikasi terutama hingga 5 hari. Selain itu, refleks cahaya dapat menurun karena pupil tertutup oleh darah. Ambliopia atau mata malas juga dapat menjadi komplikasi terutama apabila hifema terjadi pada anak-anak.
Pencegahan
Pencegahan hifema dapat dilakukan dengan pencegahan trauma pada mata menggunakan pelindung mata saat melakukan olahraga dengan bola, atau saat melakukan kegiatan yang melibatkan melempar atau menembak benda. Pada kondisi diabetes, kontrol gula darah dengan memperbaiki pola makan, aktivitas fisik, serta taat pada pengobatan dapat mencegah terjadinya pembentukan pembuluh darah baru yang merupakan faktor risiko hifema. Namun, pada penyakit terkait darah, hifema sulit dicegah.
Kapan Harus ke Dokter?
Segeralah ke dokter apabila Anda mengalami mata merah dengan penurunan tajam penglihatan secara tiba-tiba atau setelah terbentur sesuatu. Hifema merupakan salah satu kemungkinan pada kondisi ini, namun ada kondisi lainnya yang memiliki gejala serupa dan memerlukan terapi cepat seperti glaukoma akut.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Ayu Munawaroh, MKK
Gragg, J., Blair, K., & Baker, M. (2021). Hyphema. Retrieved 8 November 2021, from https://www.ncbi.nlm.nih.gov/books/NBK507802/.
Nash, D. (2019). Hyphema: Overview, Elevated Intraocular Pressure, Secondary Hemorrhage. Retrieved 8 November 2021, from https://emedicine.medscape.com/article/1190165-overview#a1.
Oldham, G., Patel, A., Greenwood, M., Salim, S., Epley, K., & Kim, W. (2021). Hyphema - EyeWiki. Retrieved 8 November 2021, from https://eyewiki.aao.org/Hyphema.