Definition
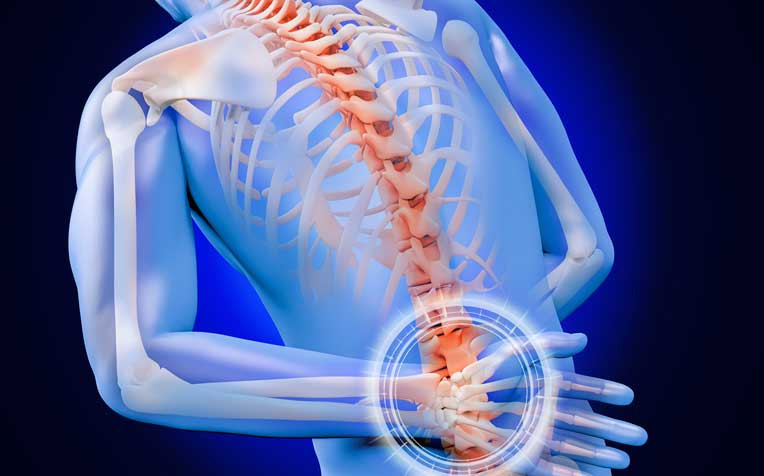
Vertebral abscess, also known as spinal cord abscess (SCA), is a rare condition that can cause permanent damage to the spinal cord. An abscess is a swelling in tissue containing a buildup of pus. This condition can occur when injured tissue becomes infected. The immune system sends white blood cells to help fight the infection. White blood cells begin to fill the damaged tissue, causing pus to accumulate. Pus consists of dead cells, immune cells, and bacteria. Since the advent and widespread use of antibiotics, the incidence of SCA has become extremely rare. SCA itself can be treated using surgery, antibiotics, and rehabilitation therapy to address its neurological symptoms.
The diagnosis of SCA is often misinterpreted with Pott's disease, osteomyelitis, compression fractures, diabetic neuropathy, or metastasis. With the development of antibiotics, radiological examinations, and surgery, the mortality rate due to SCA has decreased from 90% to 4%. However, there is still the potential for neurological disorders such as paralysis or sensory disturbances. This condition can be treated with physical therapy and rehabilitation.
Causes
SCA is usually caused by bacteria entering the spinal cord. The most common bacteria causing SCA come from Staphylococcus and Streptococcus species. Once these bacteria are in the body, they will invade places to live and grow in the spinal cord. The body will send signals to white blood cells to fight bacterial infections, causing pus to accumulate and abscesses to form. Other causes of SCA include boils that develop on the skin, especially on the back or scalp, septicemia, which is a blood infection that can spread to the central nervous system, injuries caused by foreign objects such as bullets or knives, complications from spinal surgery or lumbar puncture procedures, dermal sinuses that can form between the skin and the spinal cord during fetal development, and tuberculosis infections.
To survive, the spinal cord needs perfusion of its tissue with blood. When the pia mater layer covering the spinal cord is breached, or the patient acquires an infection in the bloodstream, infectious agents such as bacteria can breach the blood-brain barrier at the spinal cord. As part of the central nervous system, the blood-spinal cord barrier is functionally equivalent to the blood-brain barrier (defense system in the brain), causing people with low immune systems or intravenous drug users to be at risk of spinal cord infection due to mechanisms similar to those that can cause brain abscesses.
Risk factor
Some risk factors that can exacerbate SCA include a history of anticoagulant use (blood-thinning medication) or blood thinners for a long period, weakened immune systems that make it easier for bacteria to infect and thrive, Crohn's disease, which causes the formation of wounds in the digestive system, and the habit of using injectable drugs.
SCA is more common in men than in women, with the peak incidence in the first and third decades of life. Patients with a history of drug abuse, especially injectable drugs, are at very high risk, such as other immunocompromised patients like those with HIV, diabetes, or multiple organ failure.
Symptoms
SCA may initially occur without symptoms. However, over time, the infection can spread or worsen, causing compression of the spinal cord. The onset of infection and compression can trigger symptoms such as:
- Sudden pain in the spine
- Sharp pain radiating to the arms or legs
- Severe weakness
- Loss of sensation below the area of the abscess
- Weakness below the area of the abscess
- Loss of bladder and bowel control
- May be accompanied by fever
Diagnosis
A thorough interview (anamnesis) regarding the symptoms experienced, the timing of onset, and the patient's medical history and habits is necessary to establish a diagnosis of SCA. SCA symptoms are often unclear and may resemble other conditions. As a result, diagnosing SCA can be challenging in some cases.
Doctors may require several tests and diagnostic tools, including blood tests, imaging tests, and lumbar punctures. Blood tests are used to determine if there is an infection, such as complete blood count, erythrocyte sedimentation rate, C-reactive protein levels, and lumbar puncture. Doctors will also collect cerebrospinal fluid (CSF) samples for analysis.
CSF is a clear, watery fluid that surrounds and protects the spinal cord and brain. To collect CSF samples, a lumbar puncture or spinal tap is performed by inserting a needle into the spinal cavity. Other diagnostic tests can be performed including imaging tests to examine the spine. Imaging tests that can be done include X-rays, CT scans, and MRIs.
Management
Early diagnosis and treatment of SCA are crucial because if left untreated, SCA can rupture, and the infection can spread throughout the body. Because prompt treatment is needed to prevent or minimize neurological abnormalities, doctors should consider spinal abscess if patients have back pain not due to significant injury, especially if there is tenderness and pain when tapping on the upper part of the spine, or if there is fever or recent infection or dental procedure. More specific neurological abnormalities may emerge but can occur later, so delaying imaging until these neurological abnormalities appear may make adverse outcomes more likely.
Once SCA is diagnosed and its location identified, the doctor will refer to a surgeon to perform a laminectomy procedure to remove pus and fluid inside it. If dermal sinuses are found during surgery, the doctor will cut the dermal sinuses. Then the patient will be given antibiotics as further management because antibiotics can kill the bacteria causing the disease and prevent the risk of further infection.
Complications
Dangerous complications of SCA include recurrent infections, continuous pain, weakness, numbness, loss of bladder or bowel control, and even death.
This condition can also cause long-lasting neurological symptoms and complications that can last for weeks or even years after the abscess is removed. Patients may need rehabilitation to treat these symptoms. Other complications may include urinary disturbances such as dysuria or stress incontinence. Dysuria refers to difficult or painful urination. If patients experience stress incontinence, they will have difficulty controlling the bladder under physical pressure, such as when laughing.
Prevention
Prevention can be achieved by avoiding some risk factors for SCA. Stop using anticoagulant medications under a doctor's guidance if you experience sudden back pain with a pus-filled lump. Maintain your immune system and avoid drug abuse, especially injectable drugs. If you experience symptoms such as boils on the skin, especially around the spine, or infection, seek medical attention immediately for immediate treatment.
When to see a doctor?
It is recommended to see a doctor immediately if experiencing symptoms of SCA such as sudden pain, sharp pain radiating to the arms or legs, severe weakness, loss of sensation below the area of the abscess, weakness below the area of the abscess, loss of bladder and bowel control, and may be accompanied by fever. Early treatment of SCA can prevent serious complications.
- dr Nadia Opmalina
Spinal Cord Abscess: Risk Factors, Causes, & Symptoms. Healthline. 2021. Available from: https://www.healthline.com/health/spinal-cord-abscess#complications
Encyclopedia M, abscess S. Spinal cord abscess: MedlinePlus Medical Encyclopedia. Medlineplus.gov. 2021. Available from: https://medlineplus.gov/ency/article/001405.htm
Keefe P, Das J, Al-Dhahir M. Spinal Cord Abscess. Ncbi.nlm.nih.gov. 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532939/
Spinal Cord Abscess: Background, Problem, Epidemiology. Emedicine.medscape.com. 2021. Available from: https://emedicine.medscape.com/article/248030-overview#a5