Definisi
Krisis kolinergik adalah kondisi gawat darurat yang terjadi akibat stimulasi berlebihan dari reseptor muskarinik dan nikotinik. Krisis kolinergik umumnya disebabkan oleh penggunaan berlebihan dari obat-obatan antikolinesterase, seperti Pyridostigmine, Neostigmine, dan zat organofosfat yang terkandung dalam pestisida. Gejala awal dari krisis kolinergik adalah kram perut, diare, keringat berlebih, mengeluarkan liur berlebih, dan denyut nadi yang semakin melemah. Obat antikolinesterase dikonsumsi oleh pasien miastenia gravis (MG) untuk mengurangi gejala yang dialami. Pasien MG yang mengalami krisis kolinergik umumnya mengonsumsi obat dalam dosis tinggi (sekitar 120 mg per 3 jam). Kondisi yang mirip dengan krisis kolinergik adalah krisis miastenia dan krisis kolinergik lebih jarang terjadi dibandingkan krisis miastenia.
Penyebab
Asetilkolin (ACh) merupakan senyawa penting yang bekerja pada saraf parasimpatis, simpatis, dan otot rangka. Senyawa ini berfungsi untuk menghantarkan stimulus atau informasi dari otak ke organ target, baik itu otak, mata, organ pencernaan, dan otot rangka. Senyawa ini bekerja pada dua reseptor berbeda, yaitu muskarinik dan nikotinik.
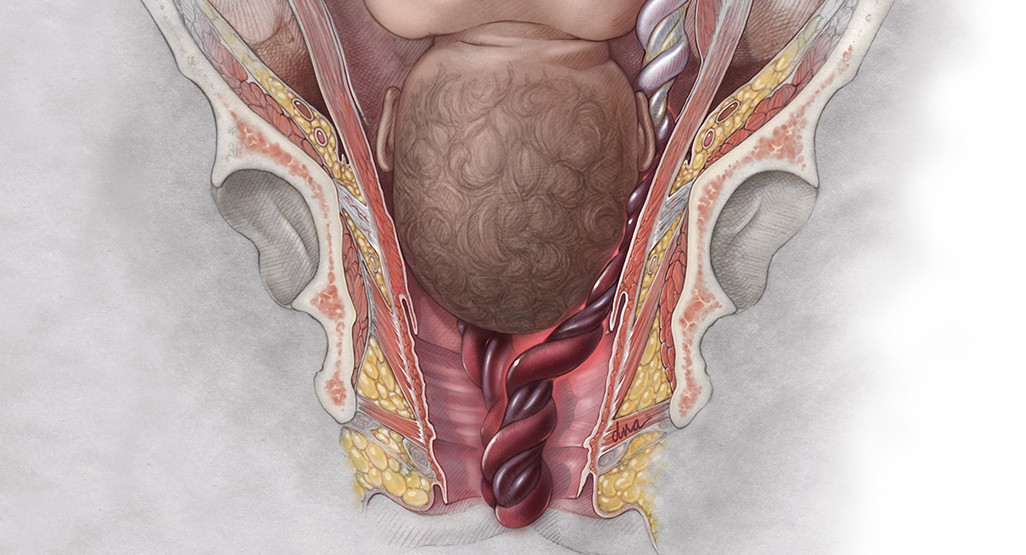
Pada otot rangka, ACh bekerja pada taut otot-saraf yaitu tempat bertemunya saraf dan otot. Setiap terjadi hantaran sinyal melalui saraf, saraf akan menghasilkan senyawa ACh, yang akan berikatan dengan reseptor spesifik pada otot, yaitu reseptor nikotinik. Ikatan antara senyawa dan reseptor menyebabkan kontraksi otot rangka. Dalam beberapa waktu, ikatan antara ACh dan reseptornya akan terlepas, kemudian ACh akan diurai oleh enzim yang disebut asetilkolinesterase (ACh-i), sehingga tidak terjadi stimulasi berlebihan pada otot. Jika terdapat stimulus kembali, proses ini akan berulang.
Selain bekerja pada otot rangka, senyawa ACh juga penting dalam menjalani fungsi otonom organ lain pada tubuh, terutama aktivasi sistem saraf parasimpatis. Aktivasi dari sistem parasimpatis menyebabkan penurunan curah jantung, relaksasi otot rangka, penyempitan bronkus, produksi air liur, dan penurunan motilitas usus.
Pada MG, jumlah senyawa ACh ingin dipertahankan sehingga otot tetap berkontraksi. Oleh karena itu, dokter akan memberikan obat penghambat enzim asetilkolinesterase, sehingga ACh tidak diurai dan otot dapat bergerak.
Pada krisis kolinergik, jumlah ACh pada taut otot-saraf dan sistem saraf secara umum terlalu banyak, sehingga saraf dan otot teraktivasi terus menerus. Hal ini menimbulkan gejala toksisitas baik secara nikotinik maupun muskarinik. Beberapa kondisi dapat mencetuskan krisis kolinergik ini, antara lain:
- Penggunaan berlebihan dari antikolinesterase pada pengobatan MG
- Paparan terhadap organofosfat (terpapar pestisida, insektisida, atau herbisida) karena tertelan, kontak langsung pada kulit atau membran mukosa, dan menghirup organofosfat
Faktor Risiko
Beberapa kondisi yang dapat meningkatkan risiko mengalami krisis kolinergik antara lain:
- Mendapatkan anestesi umum dengan dosis tinggi untuk mengurangi efek agen penghambat saraf
- Anak atau dewasa yang menghirup gas beracun
- Individu yang terpapar terhadap pestisida atau insektisida
- Pasien Miastenia Gravis yang mengonsumsi asetilkolinesterase inhibitor dosis tinggi
Gejala
Terdapat dua kelompok gejala yang terjadi pada krisis kolinergik.
Gejala muskarinik
- Kesulitan bernapas
- Pandangan buram dan mata berair
- Mual, muntah, dan diare
- Denyut nadi yang lambat
- Air liur banyak
- Keinginan untuk buang air kecil lebih sering
Gejala nikotinik
- Kejang atau kedutan berlebih pada otot yang diikuti oleh kelumpuhan. Jumlah ACh yang berlebih awalnya membuat otot berkontraksi, namun karena terlalu banyak stimulasi yang terjadi, otot tidak dapat berkontraksi kembali dan menjadi lumpuh.
- Denyut nadi yang cepat, kemudian melambat
Gejala lain yang terjadi adalah rasa gelisah, tidak dapat ditenangkan, sempoyongan, pingsan, dan bahkan koma.
Perbedaan Krisis Miastenia dan Krisis Kolinergik
Baik krisis miastenia maupun krisis kolinergik memiliki gejala awal yang sama, yaitu kelemahan dan kesulitan bernapas. Namun, krisis miastenia disebabkan oleh rendahnya senyawa ACh pada tubuh, sehingga gejala lain yang ditimbulkan juga berbeda. Gejala tersebut antara lain adalah pupil yang melebar, nadi yang cepat, tidak dapat menelan, perubahan suara, dan kelemahan pada lidah.
Diagnosis
Krisis kolinergik merupakan kondisi gawat darurat. Dokter Anda akan mendiagnosis krisis kolinergik berdasarkan gejala, tanda, dan pemeriksaan fisik yang komprehensif. Dokter akan menanyakan keluhan Anda, obat-obatan yang Anda konsumsi, dan apakah Anda terpapar terhadap zat tertentu seperti pestisida. Penting untuk Anda memberikan informasi mengenai kapan Anda terpapar zat atau mengonsumsi obat tertentu kepada dokter. Dokter juga perlu membedakan kondisi krisis kolinergik dengan krisis miastenia karena pengobatan yang berbeda.
Pemeriksaan fisik yang dilakukan meliputi sistem saraf, pernapasan, jantung, dan sistem pencernaan. Dokter akan mencari tanda tertentu seperti salivasi (air liur) berlebih, pupil yang mengecil, tekanan darah, dan kesulitan bernapas.
Pemeriksaan penunjang yang dapat dilakukan, antara lain:
- Pemeriksaan darah lengkap untuk melihat infeksi
- Panel metabolik untuk menyingkirkan kemungkinan penyebab lain, seperti metabolik, dan kondisi tidak normal yang disebabkan oleh keracunan organofosfat
- Elektrokardiografi untuk melihat adanya aritmia (gangguan irama jantung)
- X-ray toraks untuk melihat adanya edema pulmonal (penumpukan cairan diparu-paru) dan aspirasi
- CT scan untuk menyingkirkan penyebab lain dari kondisi saat ini
Tata laksana
Terdapat beberapa tahapan penanganan dari krisis kolinergik:
- Sebelum ke rumah sakit, pastikan Anda dapat mengurangi paparan terhadap zat yang menyebabkan krisis kolinergik. Dekontaminasi perlu dilakukan segera apabila kondisi ini disebabkan oleh zat organofosfat, baik gas maupun cairan. Pakaian perlu dilepaskan dari pasien untuk mencegah kontaminasi berlebihan. Segera panggil bantuan medis jika Anda berada di sekitar orang yang diduga mengalami krisis kolinergik.
- IGD, penanganan di IGD meliputi stablisasi jalan napas, pernapasan, dan sirkulasi. Jika jalan napas tidak bebas karena terhalang liur, dokter dapat melakukan intubasi (pemasangan alat bantu napas). Bantuan napas akan diberikan jika pasien kesulitan bernapas. Dokter juga akan melakukan pemberian cairan melalui infus.
- Antidotum. Penawar dari zat organofosfat adalah atropin dan oxime. Atropin dapat diberikan jika terdapat tanda nadi yang cepat, kulit yang kering dan hangat, serta pupil yang melebar. Oxime dapat diberikan jika terdapat tanda gagal napas atau kelemahan pada seluruh otot.
- Penanganan lainnya. Kejang dan rasa gelisah merupakan tanda dari krisis kolinergik yang dapat ditangani dengan obat penenang.
Penanganan ini hanya dilakukan oleh tenaga medis.
Komplikasi
Komplikasi yang dapat terjadi akibat krisis kolinergik adalah:
- Gagal napas. Gagal napas merupakan penyebab utama kematian yang disebabkan oleh krisis kolinergik.
- Aspirasi yang menyebabkan pneumonia
- Tekanan darah rendah
- Ritme jantung tidak stabil (aritmia)
- Halusinasi
- Kejang
- Gangguan elektrolit akibat muntah dan diare
- Kematian. Tingkat mortalitas dari krisis kolinergik berkisar antara 3–25%
Pencegahan
Krisis kolinergik dapat dicegah dengan menggunakan alat pelindung diri apabila berkontak erat dengan zat pestisida, insektisida, dan herbisida. Mengonsumsi obat-obatan antikolinergik sesuai dengan anjuran dokter sangat penting untuk dapat mencegah krisis kolinergik.
Kapan Harus Ke Dokter?
Jika Anda mengalami gejala krisis kolinergik di atas, segera periksakan diri ke fasilitas kesehatan terdekat. Kondisi ini merupakan kondisi gawat darurat yang memerlukan penanganan segera.
- dr Nadia Opmalina
Adeyinka A, Kondamudi NP. Cholinergic Crisis. [Updated 2021 Sep 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482433/
Sam C, Bordoni B. Physiology, Acetylcholine. [Updated 2021 Apr 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557825/
Bersten AD. (2019). Oh's Intensive Care Manual: Neuromuscular disorder. Sciencedirect. Available from: https://www.clinicalkey.com/#!/content/book/3-s2.0-B9780702072215000584
Goldenberg WD. (2018). How is a cholinergic crisis differentiated from a myasthenic crisis in myasthenia gravis?. Medscape. Available from: https://www.medscape.com/answers/793136-158060/how-is-a-cholinergic-crisis-differentiated-from-a-myasthenic-crisis-in-myasthenia-gravis