Definisi
Fraktur mandibula adalah kondisi patahnya tulang mandibula, yaitu tulang rahang bawah berbentuk V yang menjadi bagian dari tulang wajah. Penyakit ini adalah salah satu kondisi patah tulang wajah yang paling banyak ditemukan di unit gawat darurat.
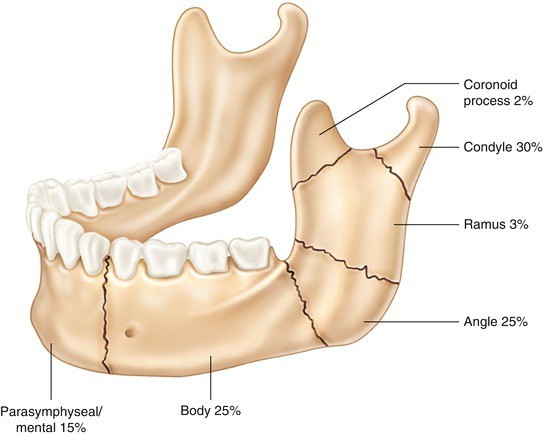
Tulang mandibula adalah struktur tulang yang kompleks. Mandibula berperan dalam pencernaan makanan di mulut, kemampuan dan artikulasi dalam berbicara serta ekspresi wajah. Patah tulang yang terjadi sering ditemukan pada lebih dari satu lokasi di tulang mandibula. Fraktur berisiko menyebabkan luka terkontaminasi dengan bakteri yang ada di mulut.
Penanganan sering melibatkan prosedur pembedahan karena kompleksnya anatomi dan fungsi dari struktur tulang wajah, di mana fraktur bisa melibatkan kerusakan gigi dan jalan napas pasien.
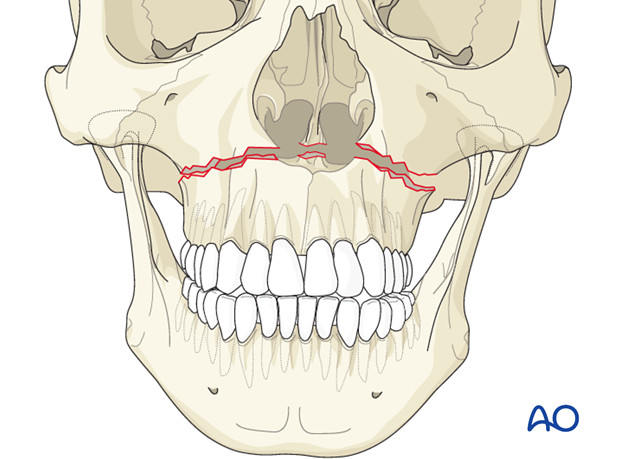
Patah tulang juga bisa terjadi pada rahang atas yang bisa Anda baca di sini: Fraktur Maksila.
Penyebab
Tulang mandibula adalah tulang wajah yang paling sering ditemukan fraktur selain tulang hidung dan tulang pipi. Penyebab dari fraktur mandibula beragam tergantung dengan usia, pola demografi masyarakat negara tersebut, kondisi lingkungan, derajat sosioekonomi dan faktor budaya.
Di bawah ini adalah hal-hal yang bisa menyebabkan fraktur mandibula, yaitu:
- Kecelakaan kendaraan bermotor.
- Kekerasan fisik dari perkelahian.
- Luka tembak.
- Kecelakaan dalam olahraga.
- Kecelakaan kerja seperti dalam pabrik industri.
- Jatuh dari ketinggian.
- Memiliki suatu kondisi medis yang menyebabkan tulang mudah patah.
Faktor Risiko
Pada cedera yang terjadi di perkotaan, kekerasan fisik adalah penyebab terbanyak dari patah tulang mandibula bila dibandingkan dengan kecelakaan bermotor. Laki-laki tiga kali lebih banyak mengalami fraktur mandibula dibandingkan perempuan, dengan sebagian besar kasus terjadi pada dekade ketiga kehidupan. Fraktur mandibula jarang ditemukan pada anak-anak yang berusia kurang dari enam tahun.
Selain itu, adanya gigi bungsu di bagian bawah bisa meningkatkan risiko fraktur mandibula. Pasien fraktur mandibula yang memiliki gigi bungsu juga memiliki risiko lebih tinggi mengalami infeksi.
Gejala
Pasien yang mengalami patah tulang pada rahang bawahnya bisa mengalami keluhan-keluhan di bawah ini:
- Nyeri pada rahang bawah yang bisa terasa terus-menerus karena fragmen tulang yang patah terus bergerak.
- Sensasi tersengat atau seperti kesemutan di area dagu bila terdapat kerusakan pada saraf mental yang menjalar ke rahang bawah.
- Maloklusi, yaitu susunan gigi di rahang atas dan bawah yang tidak sejajar.
- Wajah terlihat tidak simetris.
- Perubahan bentuk rahang.
- Penurunan rentang gerak sendi TMJ (temporomandibular joint) yang berada di dekat telinga.
- Disfagia atau kesulitan menelan.
- Trismus, kondisi otot yang spasme sehingga tidak bisa membuka mulut.
- Kerusakan gigi dan susunan gigi menjadi tidak teratur.
- Luka pada kulit liang telinga luar.
- Bengkak dan memar pada area wajah serta rahang.
- Terdengar bunyi gemeretak pada bagian tulang yang patah di mandibula.
- Perdarahan pada area rahang, mulut atau wajah.
Diagnosis
Dokter akan melakukan pemeriksaan menyeluruh ketika bertemu dengan pasien patah tulang. Dokter akan memeriksa terlebih dahulu apakah kondisi pasien tergolong stabil atau tidak. Bila pasien tidak stabil, dokter akan berusaha menstabilkan kondisi pasien terlebih dahulu.
Pemeriksaan Awal
Pada pemeriksaan awal, untuk penderita fraktur mandibula dokter akan memeriksa adanya kemungkinan penyumbatan jalan napas. Hal ini bisa diakibatkan karena patah tulang itu sendiri atau akibat perdarahan dalam rongga mulut yang bisa masuk ke dalam saluran napas.
Fraktur mandibula juga bisa disertai dengan cedera lainnya, sehingga akan diperiksa bila pasien juga mengalami cedera pada tulang belakang leher atau otak. Tanda vital seperti tekanan darah, denyut nadi, napas, suhu dan derajat nyeri, kemudian fungsi saraf dan status kesadaran pasien akan dinilai.
Wawancara Medis
Dokter bisa bertanya pada pasien atau orang-orang maupun anggota keluarga yang mengantar pasien ke fasilitas kesehatan mengenai hal-hal berikut:
- Waktu dan mekanisme terjadinya patah tulang, apakah karena kecelakaan lalu lintas, kekerasan atau hal lainnya.
- Hal-hal yang terlihat dikeluhkan pasien seperti nyeri atau perdarahan pada anggota tubuhnya.
- Riwayat penyakit pasien selama ini.
- Riwayat pengobatan yang sedang dijalankan pasien secara rutin.
Pemeriksaan Fisik
Dokter bisa melakukan beberapa jenis pemeriksaan fisik pada pasien, seperti:
- Pemeriksaan klinis pada wajah, area gigi dan mulut
- Pemeriksaan saraf untuk melihat:
- Bila terdapat perubahan sensasi
- Refleks pupil
- Perubahan kemampuan penglihatan
- Gerakan bola mata
- Gerakan lidah
- Ekspresi wajah dan otot-otot dalam mengunyah
- Pemeriksaan klinis
- Memar, bengkak, perdarahan dan gumpalan darah
- Bunyi gemeretak atau krepitasi pada tulang yang patah
- Gerakan tulang mandibula
- Keterbatas gerakan
- Perubahan susunan dan kerusakan pada gigi, seperti gigi yang longgar, patah atau tanggal
- Cedera lain pada anggota tubuh lain
Pemeriksaan Penunjang
Kondisi patah tulang akan memerlukan pemeriksaan pencitraan atau gambaran radiologi. Dokter bisa melakukan pemeriksaan di bawah ini:
- Pemeriksaan x-ray pada tulang mandibula yang dilihat dari tampilan depan-belakang, samping kanan dan kiri atau lainnya untuk melihat kelainan yang ada.
- Scan panoramik gigi untuk membantu menilai tulang rawah.
- CT scan juga bisa dilakukan bila dicurigai terjadi patah tulang pada wajah
- X-ray dada dilakukan pada pasien yang tidak sadar atau mengalami gigi tanggal, untuk memeriksa bila gigi yang tanggal tersebut tidak masuk ke saluran napas.
- Pemeriksaan laboratorium dilakukan bila perlu atau sebelum prosedur bedah.
Tata Laksana
Penanganan Awal
Dokter akan berusaha menstabilkan kondisi pasien terlebih dahulu serta menangani kondisi yang bersifat darurat dan membahayakan nyawa pasien. Pasien akan dibaringkan dalam posisi telentang. Kemudian hal-hal yang bisa menyumbat mulut dan jalan napas pasien seperti benda asing, gigi yang tanggal, darah, lendir, atau gumpalan darah akan dibersihkan. Leher pasien juga akan distabilkan dengan collar leher. Bila ada perdarahan hebat, cedera pada tulang belakang leher atau kepala, dokter bisa mengutamakan pengobatan pada kondisi tersebut terlebih dahulu.
Untuk mencegah terjadinya infeksi bakteri yang bisa memperparah kondisi pasien, dokter bisa memberikan obat antibiotik. Selain itu, bila tidak ada luka yang bersih, pemberian vaksin tetanus juga dapat dipertimbangkan. Obat antinyeri akan diberikan dokter untuk mengurangi keluhan nyeri.
Pengobatan Fraktur
Tujuan pengobatan pada kondisi fraktur adalah untuk memulihkan kekuatan mekanis pada lokasi tulang yang patah agar sehat kembali. Selain itu diharapkan fungsi otot di sekitar tulang yang patah juga dapat kembali normal.
Pada pengobatan fraktur, bagian tulang yang patah akan berusaha dikembalikan ke posisi anatomi normalnya. Kemudian bagian tulang tersebut akan difiksasi. Dokter akan mempertimbangkan bila pasien memerlukan prosedur pembedahan untuk mengatasi kondisinya.
Komplikasi
Umumnya prognosis atau prediksi mengenai kesembuhan penyakit pasien pada fraktur mandibula baik, terutama bila patah tulang tidak disertai dengan cedera lainnya. Namun, sebagian pasien fraktur mandibula bisa mengalami cedera lain seperti cedera pada kepala, leher atau mata, dan patah tulang pada area wajah, hidung atau tulang belakang.
Komplikasi yang paling sering terjadi adalah infeksi. Terjadinya infeksi bisa meningkatkan risiko patah tulang tidak sembuh setelah 9 bulan tanpa adanya tanda-tanda penyembuhan, atau tulang sembuh namun dalam posisi yang tidak normal.
Komplikasi lain yang bisa terjadi adalah gangguan saraf yang menjalar di area wajah dan rahang serta masalah pada gigi.
Pencegahan
Anda bisa menerapkan kebiasaan berkendara yang baik untuk menghindari terjadinya kecelakaan. Pakailah helm atau sabuk pengaman dan selalu mengemudi dalam batas kecepatan yang aman. Jika Anda bekerja di area yang rawan seperti pabrik industri, selalu kenakan alat pelindung diri untuk melindungi diri dari kemungkinan terjadinya cedera.
Kapan Harus ke Dokter?
Patah tulang adalah kondisi gawat darurat yang perlu ditangani. Oleh karena itu, bila Anda atau orang yang Anda kenal mengalami patah tulang, mereka harus segera dibawa ke unit gawat darurat untuk mendapat pengobatan.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Hanifa Rahma
Yuen, H. W., Hohman M. H., Mazzoni, T. Mandible Fracture (2023). Retrieved 26 March 2023, from https://www.ncbi.nlm.nih.gov/books/NBK507705/#.
Weerakkody, Y. Mandibular Fracture (2022). Retrieved 26 March 2023, from https://radiopaedia.org/articles/mandibular-fracture.
Dergin, G., Emes, Y., Aybar, B. Evaluation and Management of Mandibular Fracture (2019). Retrieved 26 March 2023, from https://www.intechopen.com/chapters/65088.