Definition
Fainting, also known as syncope in medical terms, is a condition where a person loses consciousness, loses control of their body, and suddenly becomes weak, but can recover. Just before fainting, a person may experience symptoms known as pre-syncope. About 35% of the world's population experiences fainting at least once in their lifetime. Syncope can occur once or repeatedly. It is important to recognise what syncope is and when it should be considered a warning sign of life-threatening conditions such as heart problems.
Causes
Syncope is caused by a temporary decrease in blood flow to the brain. This can be due to a drop in blood pressure, a decrease in heart rate, or a change in the amount of blood in the body. Based on the cause, syncope can be classified into:
1. Vasovagal Syncope
The most common type of syncope. It is caused by a sudden drop in blood pressure leading to a decrease in blood flow to the brain. One factor that can cause this is changing position from sitting to standing. Patients with vasovagal syncope often have a condition called orthostatic hypotension, which is a drop in blood pressure due to a change in position.
2. Situational Syncope
This condition is caused by certain situations that can trigger syncope. Situational syncope is a part of vasovagal syncope. Situations that can cause this include dehydration (lack of fluids), emotional stress, anxiety, fear, pain, hunger, use of medication or alcohol, hyperventilation (breathing too quickly), coughing hard, and urinating.
3. Postural Syncope
Caused by suddenly changing position from lying down to standing. This can be due to certain medications and dehydration (lack of fluids). Postural syncope can also occur along with a rapid heart rate known as postural orthostatic tachycardia syndrome.
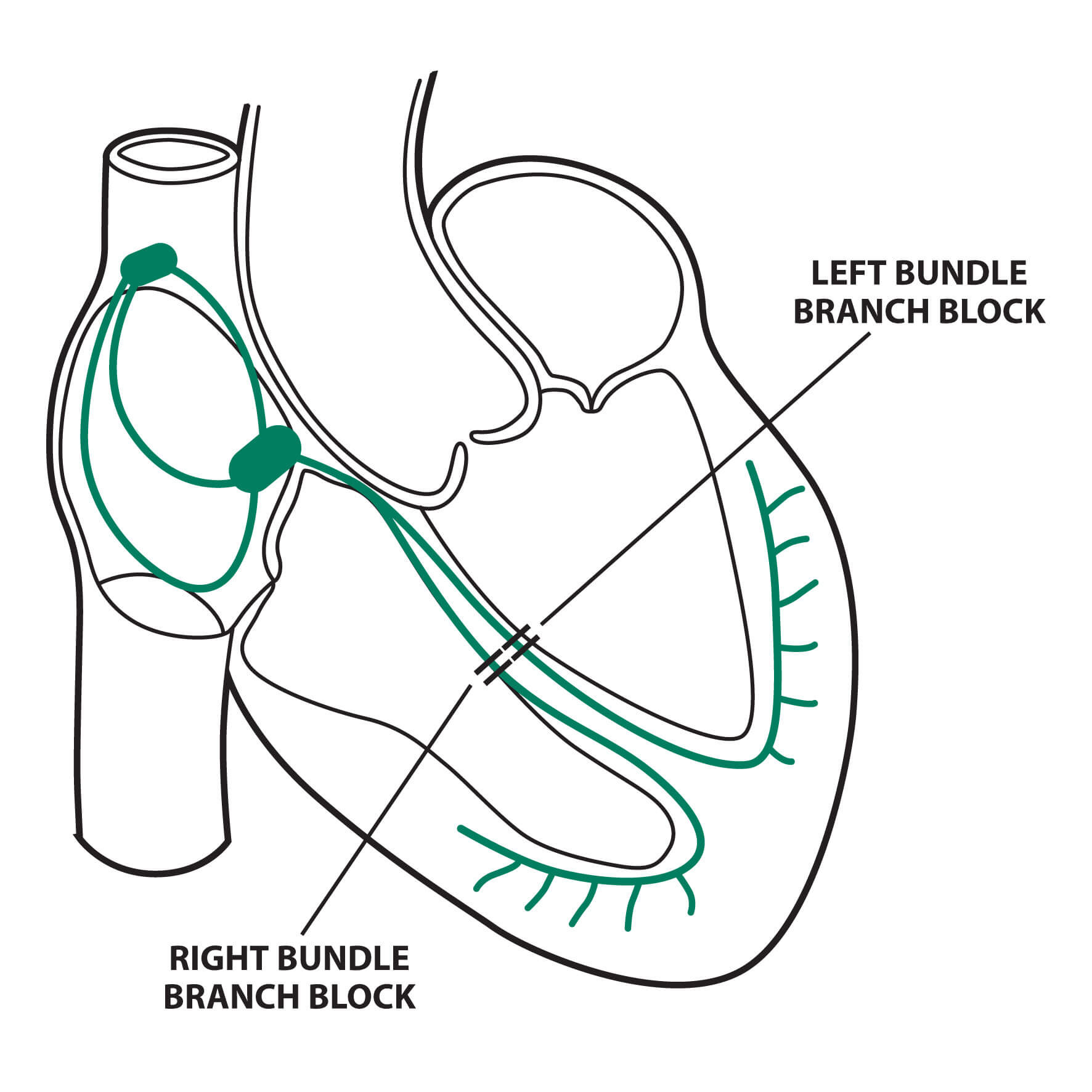
4. Cardiac Syncope
Caused by heart problems or blood vessels in the heart that disrupt blood flow to the brain. Heart disorders that can cause syncope include arrhythmias, structural heart problems, valve issues, and blockages in the heart's blood vessels.
5. Neurological Syncope
Caused by neurological events such as transient ischemic attack (TIA) or stroke. Other events that can cause fainting include migraine headaches and hydrocephalus (fluid buildup in the brain).
Risk factor
Several risk factors can make someone more likely to experience syncope, including:
- Diabetes mellitus.
- Heart disorders, such as arrhythmias and a history of congestive heart failure.
- Neurological disorders like stroke.
- Anemia or lack of red blood cells, which carry oxygen to the body's tissues.
- History of low blood pressure.
- Age: Older people are more prone to syncope.
Symptoms
When a person loses consciousness accompanied by seizures, heart attack, head injury, intoxication (poisoning), and low blood sugar, this is not called fainting. Symptoms of fainting include:
- Feeling dizzy and often experiencing visual disturbances such as darkened vision.
- Hearing disturbances.
- Palpitations or heart pounding.
- Cold sweat.
- Difficulty standing for long periods and loss of balance.
- Headache.
- Sudden fall.
- Fainting occurs for a short time, and confusion may be felt upon regaining consciousness.
- Recurrent fainting can be a symptom of a more serious illness.
Diagnosis
When someone faints, several tests can be done to find the cause of syncope:
- Laboratory tests: Blood tests to check hemoglobin levels or other metabolic disorders that can cause syncope.
- Electrocardiogram (EKG): A simple test to check the electrical activity of the heart. EKG can be done while lying down or during activities like treadmill exercises.
- Echocardiogram: A heart test using ultrasound to view the heart's structure.
- Neurological examination: Includes testing consciousness, higher functions, cranial nerves, motor system, and sensory system.
- Computed Tomography (CT) Scan: Done to check for abnormalities in the central nervous system, such as a stroke that could cause fainting.
Management
If you experience fainting, there are several things to be cautious about:
- Review any medications you are taking or consult a doctor if your medications cause symptoms.
- Monitor your diet. Ensure your food meets daily nutritional needs and stay hydrated.
- If you have a history of heart disorders, consult a doctor for appropriate treatment.
- Be careful when changing positions from sitting to standing. If you feel like you might faint, sit down and put your head between your knees while leaning forward.
- Treatment for syncope varies for each individual. The main goal is to increase blood flow to the brain to meet oxygen needs. Therefore, it is important to consult a doctor to find the cause of syncope.
Complications
Recurrent syncope can affect a person's quality of life. Potential complications include:
- Body injuries, which can be severe if fainting occurs while driving.
Prevention
If you have a history of fainting, several measures can be taken to prevent recurrence:
- Avoid standing for long periods.
- Stay hydrated by drinking plenty of water to prevent dehydration.
- Get adequate rest.
- Be cautious when changing positions from sitting to standing.
- If you have a history of heart disease or neurological disorders like stroke, have regular health check-ups.
When to see a doctor?
Seek immediate medical attention if you or someone close to you experiences:
- Fainting while lying down.
- Fainting accompanied by sudden chest pain or shortness of breath.
- A family history of heart attacks at a young age.
- Use of a pacemaker.
- History of low blood pressure and abnormal heart rate (either too slow - bradycardia, or too fast - tachycardia).
- Other symptoms related to heart disorders.
- Recurrent fainting requires further examination and treatment. Consult your symptoms with a doctor for appropriate therapy.
Looking for more information about other diseases Click here!
- dr Nadia Opmalina
- Syncope (Fainting). Hopkinsmedicine.org. (2021). Retrieved 29 November 2021, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/syncope-fainting.
- Syncope: Symptoms, Causes, Treatments. Cleveland Clinic. (2021). Retrieved 29 November 2021, from https://my.clevelandclinic.org/health/diseases/17536-syncope.
- Ling, L., Feng, T., Xue, X., & Ling, Z. (2021). Etiology, risk factors, and prognosis of patients with syncope: A single‐center analysis. Annals Of Noninvasive Electrocardiology, 26(6). https://doi.org/10.1111/anec.12891
- Fedorowski, A., Pirouzifard, M., Sundquist, J., Sundquist, K., Sutton, R., & Zöller, B. (2021). Risk Factors for Syncope Associated With Multigenerational Relatives With a History of Syncope. JAMA Network Open, 4(3), e212521. https://doi.org/10.1001/jamanetworkopen.2021.2521Fedorowski, A., Pirouzifard, M., Sundquist, J., Sundquist, K., Sutton, R., & Zöller, B. (2021). Risk Factors for Syncope Associated With Multigenerational Relatives With a History of Syncope. JAMA Network Open, 4(3), e212521. https://doi.org/10.1001/jamanetworkopen.2021.2521
- Kojodjojo, P., Boey, E., Elangovan, A., Chen, X., Tan, Y., & Singh, D. et al. (2016). Mapping clinical journeys of Asian patients presenting to the Emergency Department with syncope: Strict adoption of international guidelines does not reduce hospitalisations. International Journal Of Cardiology, 218, 212-218. https://doi.org/10.1016/j.ijcard.2016.05.019
- Gibson, T., Weiss, R., & Sun, B. (2018). Predictors of Short-Term Outcomes after Syncope: A Systematic Review and Meta-Analysis. Western Journal Of Emergency Medicine, 19(3), 517-523. https://doi.org/10.5811/westjem.2018.2.37100
- Barbic, F., Dipaola, F., Casazza, G., Borella, M., Minonzio, M., & Solbiati, M. et al. (2019). Syncope in a Working-Age Population: Recurrence Risk and Related Risk Factors. Journal Of Clinical Medicine, 8(2), 150. https://doi.org/10.3390/jcm8020150
- Grossman, S., & Badireddy, M. (2021). Syncope. Ncbi.nlm.nih.gov. Retrieved 29 November 2021, from https://www.ncbi.nlm.nih.gov/books/NBK442006/.
- Vasovagal Syncope | Cedars-Sinai. Cedars-sinai.org. (2021).
- Syncope. Rms.kernowccg.nhs.uk. (2021).