Definisi
Kegawatdaruratan psikiatri adalah gangguan kejiwaan akut pada pikiran, perilaku, suasana hati, atau hubungan sosial yang memerlukan penanganan segera. Akut berarti keluhan baru saja terjadi atau muncul secara tiba-tiba. Keadaan darurat ini harus segera ditangani untuk menyelamatkan pasien dan/atau orang lain dari bahaya yang mungkin terjadi karena gangguan tersebut.
Pasien yang datang dengan keadaan darurat psikiatri biasanya memiliki gangguan mania, psikosis akut, ide bunuh diri, atau ide pembunuhan. Psikosis adalah ketika seseorang mengalami gangguan hubungan dengan kenyataan sehingga tidak dapat membedakan mana yang nyata dan tidak nyata.
Penyebab
Penyebab gangguan perilaku ekstrem ini bervariasi, seperti penggunaan zat, kondisi medis, gangguan mood, atau kecemasan dan trauma yang hebat. Hampir semua pasien dengan pikiran bunuh diri juga memiliki penyakit kejiwaan sebelumnya, seperti depresi berat, penyalahgunaan zat, atau skizofrenia.
Sekitar 50% pasien dengan kedaruratan psikiatri juga memiliki penyakit medis. Sehingga, skrining medis penting untuk menilai kondisi fisik yang mungkin berperan pada kegawatdaruratan psikiatri. Rangkaian pemeriksaan skrining dilakukan untuk melihat bila seseorang berisiko mengalami penyakit tertentu.
Beberapa penyebab psikosis akut dan mania adalah delirium, infeksi, gangguan metabolisme, obat-obatan, penyalahgunaan/putus obat, dan gangguan otak atau sistem saraf pusat.
Faktor Risiko
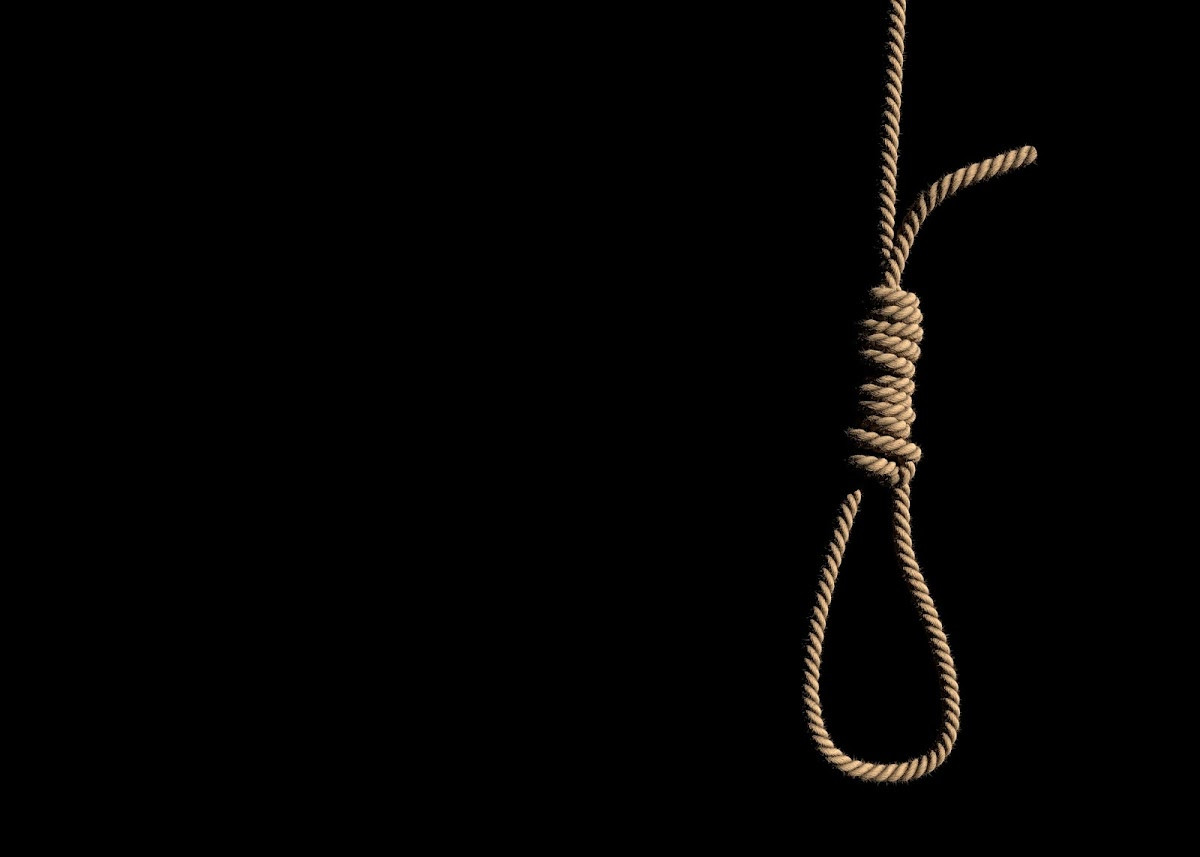
Pada penderita gangguan jiwa, adanya pikiran bunuh diri pada dirinya merupakan salah satu kondisi gawat darurat yang harus segera ditangani. Faktor-faktor yang dapat meningkatkan risiko terjadinya bunuh diri antara lain:
- Jenis kelamin laki-laki
- Usia lebih dari 60 tahun
- Janda atau bercerai
- Ras kulit putih
- Hidup sendiri
- Pengangguran atau memiliki masalah keuangan
- Korban perundungan
- Riwayat kejadian traumatis
- Penyakit medis jangka panjang
- Gangguan kejiwaan seperti depresi, skizofrenia, serangan panik, gangguan cemas berat
- Penyalahgunaan zat
- Perasaan keputusasaan
- Anhedonia berat atau tidak tertarik untuk bergembira
- Kemudahan akses alat bunuh diri
- Adanya ide atau riwayat percobaan bunuh diri
Gejala
Pasien dengan psikosis akut dan mania menunjukkan perilaku eksentrik dan berlebihan, pemikiran yang tidak biasa, tidak teratur, paranoid, serta perilaku yang tidak pantas atau berbahaya. Gejala darurat lainnya yang memerlukan penanganan segera adalah berpikiran atau mencoba bunuh diri, membunuh, menyakiti, atau merusak.
Tanda waspada seseorang dapat melakukan percobaan bunuh diri antara lain:
- Sering berbicara atau menulis tentang kematian, sekarat, atau bunuh diri
- Membuat komentar tentang putus asa, tidak berdaya, atau tidak berharga
- Ekspresi tidak memiliki alasan untuk hidup, tidak ada tujuan dalam hidup, mengatakan hal-hal seperti "akan lebih baik jika saya tidak di sini"
- Peningkatan penyalahgunaan alkohol dan/atau narkoba
- Penarikan diri dari teman, keluarga, dan komunitas
- Berperilaku sembrono atau berisiko, seolah-olah tanpa berpikir
- Perubahan suasana hati yang dramatis
- Merasa menjadi beban orang lain
Sedangkan tanda krisis emosional yang dapat berkembang menjadi kegawatdaruratan psikiatri meliputi:
- Mengabaikan kebersihan, misalnya tidak mandi
- Perubahan kebiasaan tidur, kurang tidur atau justru tidur berlebihan
- Kenaikan atau penurunan berat badan yang signifikan
- Penurunan kinerja di tempat kerja atau sekolah
- Perubahan ekstrem pada suasana hati, seperti merasa lebih mudah tersinggung, marah, cemas, atau sedih
- Menarik diri dari aktivitas, pekerjaan, atau hubungan
- Gejala mengkhawatirkan lainnya termasuk paranoid atau halusinasi
Diagnosis
Pada kondisi kegawatdaruratan psikiatri seperti gejala psikosis akut dan mania, atau percobaan bunuh diri, dokter akan menangani kondisi darurat yang ada terlebih dahulu dan mengamankan situasi. Setelah suasananya sudah aman dan kondusif, baru dilakukan wawancara dan pemeriksaan pada pasien dan keluarga atau orang terdekat pasien.
Biasanya dokter akan bertanya mengenai apa yang terjadi saat kejadian berlangsung, menilai status mental pasien, aktivitasnya sehari-hari, serta riwayat kesehatannya, termasuk kesehatan jiwa, konsumsi obat-obatan tertentu, dan bila ada riwayat penggunaan zat. Wawancara juga disertai dengan pemeriksaan fisik pada tubuh pasien.
Pada kasus dimana pasien yang memiliki ide bunuh diri, setelah situasi aman dan terkendali, dokter akan mencari tahu faktor-faktor yang meningkatkan atau menurunkan risiko bunuh diri. Biasanya akan ditanyakan juga bila pasien pernah melakukan percobaan bunuh diri atau adanya ide bunuh diri sebelumnya. Penting untuk memperoleh informasi rinci tentang pasien agar mudah membina hubungan baik dengan pasien.
Penilaian pasien dengan ide pembunuhan mirip dengan pasien bunuh diri. Belum diketahui pasti faktor risiko dari gangguan ini. Faktor risiko yang harus dinilai oleh dokter adalah riwayat kekerasan dan akses senjata. Saat menilai pasien ini, harus tersedia jalur keluar yang dapat diakses dengan cepat dan tidak dapat dihalangi pasien sebagai antisipasi jika pasien berperilaku berbahaya di tengah pemeriksaan.
Diagnosis sementara yang didapatkan dari hasil pemeriksaan di atas akan memandu pemeriksaan dan penanganan lebih lanjut. Dokter juga akan mempertimbangkan pemeriksaan penunjang tertentu untuk menyingkirkan penyebab medis umum atau penggunaan zat, seperti:
- Pemeriksaan narkoba melalui urine
- Tes kadar alkohol dalam darah
- Pungsi lumbal atau pemeriksaan cairan otak dilakukan bila dicurigai ada kondisi peradangan selaput otak dan sumsum tulang (meningitis) atau peradangan pada otak (ensefalitis)
- CT scan atau pencitraan lain tidak menambahkan banyak informasi jika tidak ada temuan abnormal pada pemeriksaan, kecuali pada pasien lanjut usia
Tata laksana
Psikosis akut, mania, agitasi, atau ide pembunuhan
Tujuan utama pengobatan adalah menstabilkan dan memastikan keselamatan pasien serta lingkungan sekitar. Pendekatan awal untuk pasien yang mengalami agitasi atau kegelisahan akut adalah membantu mengelola stresnya, seperti melalui terapi perilaku, obat-obatan, atau keduanya.
Ketika pasien memiliki penyakit medis penyerta yang berperan pada kegawatdaruratan psikiatrinya, penting untuk mengobati penyakit medis tersebut. Pada beberapa kasus, penyakit medis merupakan penyebab kedaruratan psikiatri dan oleh karena itu harus dapat dibedakan dengan gangguan kejiwaan murni.
Saat memeriksa pasien dengan agitasi akut, dokter harus membantu pasien merasa aman dengan menciptakan lingkungan yang tidak mengancam dan berbicara dengan tenang serta nada rendah. Sehingga, pasien dapat mengendalikan emosinya dan mau terlibat dalam pengobatan. Perlu disiapkan juga dokter atau pemeriksa cadangan.
Jika penanganan cepat atau terapi sedasi diperlukan, harus diberikan melalui obat suntikan. Jika pasien memiliki penyakit medis penyerta, perlu adanya penyesuaian obat untuk mencegah komplikasi.
Ide bunuh diri
Perawatan pasien dengan ide bunuh diri bertujuan mengurangi risiko dan penguatan faktor pelindung. Faktor dan risiko tersebut antara lain keselamatan pasien, stres psikologis atau sosial, dukungan sosial, dan gangguan kejiwaan yang dapat diobati.
Ketika menangani pasien dengan ide bunuh diri, dokter harus membina hubungan baik dan mengikutsertakan pasien serta keluarga pada pengobatan. Dokter perlu menentukan tempat yang aman sebagai lokasi perawatan. Sebelum menempati tempat perawatan, pasien harus dibebaskan dari benda-benda yang dapat membahayakan.
Pada keadaan depresi, psikoterapi dan terapi perilaku kognitif dapat membantu. Selain itu, terapi perilaku kognitif dapat mengurangi keputusasaan dan upaya bunuh diri pada pasien rawat jalan. Untuk pasien dengan gangguan kepribadian ambang dan ide bunuh diri, terapi psikodinamik dan terapi perilaku dialektis mungkin berguna.
ECT (Electroconvulsive Therapy) atau terapi kejut listrik telah terbukti bermanfaat pada pasien dengan ide bunuh diri, bahkan aman untuk ibu hamil. Namun, terapi tersebut tidak cukup untuk pemeliharaan kondisi pasien dalam jangka panjang dan harus dikombinasikan dengan obat.
Komplikasi
Komplikasi dari kegawatdaruratan psikiatri adalah dapat membahayakan diri sendiri dan lingkungan sekitar. Dapat timbul cedera fisik, atau bahkan kehilangan nyawa baik diri sendiri maupun orang lain. Komplikasi lain berupa efek samping obat seperti obat golongan benzodiazepin yang dapat menyebabkan penekanan pada pernapasan, dan obat antipsikotik dapat menyebabkan gangguan saraf.
Orang yang gelisah atau melakukan kekerasan sering datang ke fasilitas kesehatan dengan kondisi diikat oleh polisi. Terkadang, pasien bisa meninggal dalam pengekangan sebelum atau segera setelah tiba di rumah sakit. Penyebabnya diperkirakan akibat kombinasi dari gangguan metabolisme dan peningkatan suhu tubuh saat mengamuk, penggunaan narkoba, aspirasi isi lambung ke saluran napas, emboli akibat pengekangan untuk waktu yang lama, dan terkadang akibat gangguan medis serius yang mendasari.
Kematian lebih mungkin terjadi jika orang ditahan dalam posisi pergelangan tangan diikat ke pergelangan kaki di belakang punggung. Jenis pengekangan ini dapat menyebabkan asfiksia (kondisi kekurangan oksigen) dan kondisi ini harus dihindari.
Pencegahan
Penting untuk mengetahui tanda waspada percobaan bunuh diri agar dapat mencegah dan membantu pasien. Pencegahan yang dapat dilakukan antara lain:
- Tanyakan kepada orang yang Anda khawatirkan apakah mereka berpikir untuk bunuh diri. Meskipun orang lain ragu menanyakan ini, namun penelitian menunjukan kalau tindakan ini berguna
- Jaga agar mereka tetap aman. Kurangi akses pasien pada alat bunuh diri, seperti senjata, benda tajam, korek api, atau insektisida
- Menemani dan mendengarkan apa yang mereka butuhkan
- Bantu mereka mendapatkan dukungan yang berkelanjutan
- Tetap terhubung dengan mereka untuk memantau perkembangannya
Kapan harus ke dokter?
Jika Anda atau orang yang Anda kenal memiliki salah satu gejala kegawatdaruratan psikiatri di atas, segera beritahu orang terdekat untuk mendapatkan pertolongan. Mintalah untuk dibawa ke unit gawat darurat jika gejala tidak dapat dikontrol. Penanganan segera dapat mencegah komplikasi yang merugikan diri sendiri maupun orang lain.
- dr Hanifa Rahma
Wheat, S., Dschida, D., & Talen, M. R. (2016). Psychiatric Emergencies. Primary Care: Clinics in Office Practice, 43(2), 341–354. DOI: 10.1016/j.pop.2016.01.009
Purse, M. (2020). When to call your psychiatrist or go to the ER for emergent symptoms. Retrieved 14 February 2022, from https://www.verywellmind.com/urgent-and-emergent-psychiatric-symptoms-and-signs-378825
Zeller, S. (2021). Retrieved 13 february 2022, from https://www.psychiatrictimes.com/view/10-most-common-presentations-emergency-psychiatry





/62d244a608bfb.jpg)





