Definisi
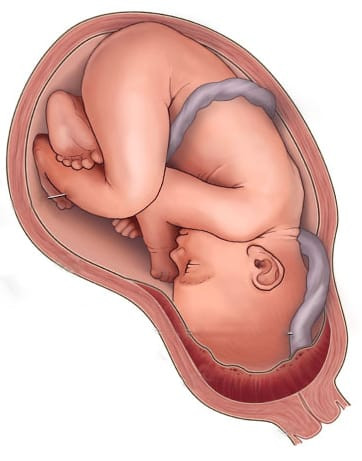
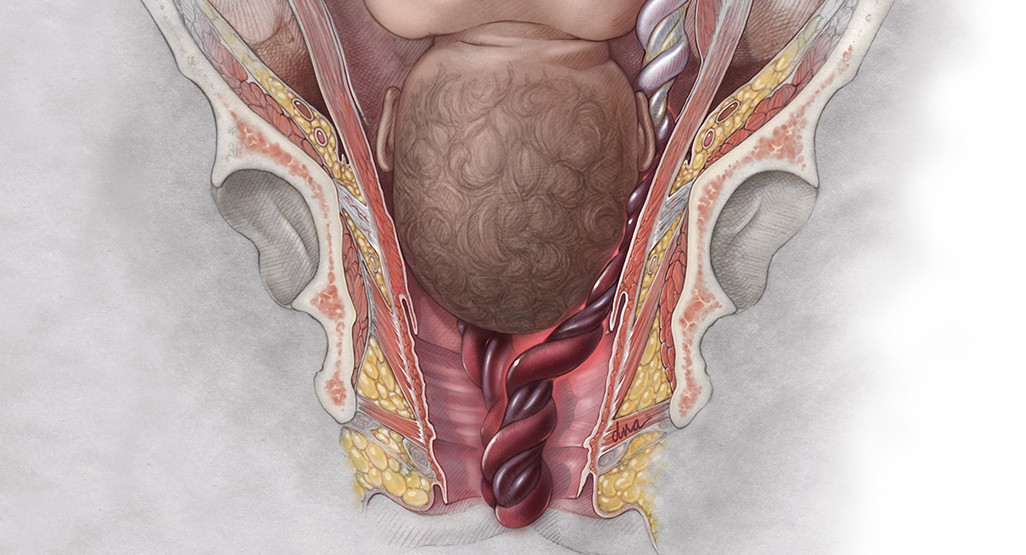
Vasa previa adalah adanya pembuluh darah tali pusat janin yang tidak terbungkus dengan suatu selaput, melintas pada bagian mulut rahim. Apabila memasuki proses persalinan, mulut rahim akan terbuka dan selaput ketuban akan pecah. Kondisi ini mengakibatkan pembuluh darah tali pusat juga pecah dan terjadi perdarahan. Sehingga menyebabkan janin kehilangan banyak darah dan bahkan bisa menyebabkan kematian pada janin, serta komplikasi pada ibu.
Vasa previa jarang terjadi dan menjadi salah satu bentuk komplikasi selama kehamilan. Vasa previa juga menjadi penyebab terjadinya perdarahan selama kehamilan dan mengakibatkan janin dalam kondisi stres karena mengalami perdarahan.
Angka kejadian vasa previa sekitar 1 dari setiap 2.500-5.000 persalinan. Selain itu, vasa previa juga sering terjadi pada kehamilan dengan menggunakan metode bayi tabung (IVF) yaitu sekitar 1 dari setiap 200 persalinan. Kematian janin akibat vasa previa sekitar 56%-60% apabila tidak didiagnosis sejak dini sebelum proses melahirkan.
Oleh karena itu, deteksi sejak dini vasa previa dapat mengurangi angka kematian pada janin dan komplikasi kesehatan bagi ibu. Apabila didiagnosis lebih dini, maka dapat meningkatkan kelangsungan hidup janin sebesar 97%. Pasca persalinan, beberapa bayi membutuhkan perawatan di ruang rawat intensif bayi baru lahir (NICU) untuk menstabilkan kondisi bayi.
Jika Anda juga ingin mengetahui penyulit persalinan lainnya, seperti Plasenta Previa, Anda dapat membacanya di sini: Plasenta Previa - Pengertian, Pengobatan, Gejala, dan Pengobatan.
Penyebab
Secara umum, terdapat 2 penyebab yang mengakibatkan terjadinya vasa previa selama kehamilan yaitu sebagai berikut:
- Vasa previa yang disebabkan oleh adanya pembuluh darah tali pusat yang menyisip pada ketuban. Normalnya pembuluh darah tali pusat berada pada pusat plasenta. Namun pada vasa previa pembuluh darah tali pusat masuk ke dalam bagian ketuban dan keluar dari pusat plasenta menyebabkan pembuluh darah tidak dilindungi oleh selaput Wharton yang terletak dalam tali pusat. Sehingga saat ketuban pecah, pembuluh darah tali pusat yang berada dalam ketuban juga ikut pecah.
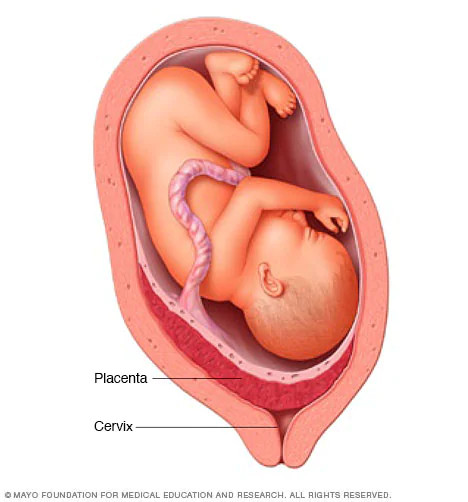
- Vasa previa juga dapat terjadi pada plasenta yang terbelah menjadi dua bulatan. Dengan tali pusat menghubungkan satu bulatan plasenta satu dengan bulatan plasenta lainnya. Apabila terdapat pembuluh darah tali pusat yang terbuka dan tidak dilindungi oleh suatu selaput melintas di antara dua bulatan plasenta tersebut dan terletak didekat rahim. Maka pembuluh darah tersebut akan mudah pecah saat proses persalinan terjadi.
Faktor Risiko
Faktor risiko yang meningkatkan terjadinya vasa previa seperti di bawah ini:
- Letak plasenta yang rendah di dalam rahim, berada didekat mulut rahim atau bahkan menutupi serviks.
- Riwayat menjalani operasi caesar sebelumnya
- Riwayat kehamilan dengan menggunakan metode bayi tabung (IVF)
- Kehamilan kembar atau lebih dari 3
- Riwayat operasi pada bagian organ rahim sebelumnya
- Merokok
- Kehamilan usia tua (usia ibu saat hamil lebih dari 35 tahun)
- Mengalami penyakit kronik seperti diabetes
- Riwayat menjalani prosedur kuretase
Gejala
Gejala Pada Ibu
Umumnya vasa previa tidak menunjukkan gejala hingga persalinan terjadi. Namun beberapa ibu hamil mengalami keluhan nyeri ringan pada vagina.
Selain itu, terdapat perdarahan pada vagina dengan berwarna merah gelap yang terjadi pada trimester 2 dan 3 kehamilan. Kondisi ini menunjukkan bahwa janin dalam kandungan mengalami kekurangan oksigen (hipoksia), sehingga warna darah tampak lebih gelap.
Gejala Pada Janin
Sedangkan gejala yang dapat ditemui pada janin adalah adanya detak jantung yang lebih lambat (bradikardia). Oleh karena itu, karena vasa previa tidak langsung menunjukkan gejala. Sebaiknya Ibu selalu rutin melakukan pemeriksaan kehamilan untuk mendeteksi adanya komplikasi dalam kehamilan seperti vasa previa. Deteksi dini vasa previa lebih awal dapat mengurangi angka kematian pada bayi saat persalinan.
Diagnosa
Diagnosis dari vasa previa dapat ditegakkan melalui pemeriksaan penunjang USG (ultrasonografi) perut yang dapat dilakukan saat pemeriksaan rutin kehamilan. Adanya vasa previa saat hamil dapat dideteksi pada usia kehamilan memasuki 18-26 minggu. Hal ini dikarenakan pada awal kehamilan atau trimester pertama belum bisa mendeteksi adanya vasa previa atau tidak.
Apabila dari hasil pemeriksaan USG perut ditemukan adanya vasa previa, biasanya dokter akan merekomendasikan untuk dilakukan pemeriksaan USG transvaginal. Pemeriksaan ini dilakukan dengan cara memasukkan alat USG khusus yang dimasukkan ke vagina (jalan lahir). Langkah ini dilakukan untuk konfirmasi dari hasil pemeriksaan USG perut yang menemukan adanya vasa previa.
Melalui pemeriksaan USG transvaginal, dapat menggambarkan secara detail bagian pembuluh darah tali pusat yang melintas pada bagian vagina. Sebagai tambahan juga dapat dilakukkan pemeriksaan USG doppler yang menggambarkan aliran darah tali pusat lebih jelas.
Tata Laksana
Ketika dokter sudah menegakkan diagnosis vasa previa dalam kehamilan Ibu. Maka dokter akan merekomendasikan beberapa langkah terapi dan pengobatan terhadap vasa previa yang dialami oleh Ibu. Dokter akan melakukan pemantauan terhadap kehamilan Ibu secara ketat untuk memaksimalkan waktu keberlangsungan kehamilan sebelum risiko melahirkan sudah tiba.
Secara keseluruhan, tujuan dari terapi dan pengobatan vasa previa adalah memperpanjang masa hamil dengan aman dan melahirkan bayi lebih awal sebagai bentuk pencegahan pembuluh darah pecah. Berikut ini adalah beberapa langkah tatalaksana yang dapat dilakukan:
- No-stress test, meliputi pemeriksaan untuk menilai detak jantung janin yang dilakukan 2 kali dalam seminggu secara teratur. Pemeriksaan ini aman dilakukan untuk janin.
- Obat kortikosteroid, pemberian obat ini bertujuan untuk membantu paru-paru janin berkembang dan matang sebelum persalinan melalui operasi caesar dilaksanakan.
- Dokter akan merekomendasikan Ibu untuk rawat inap di rumah sakit lebih awal sebelum waktu persalinan. Sehingga, dokter dapat memantau secara ketat kondisi Ibu dan janin menjelang melahirkan.
- Tindakan operasi mungkin dilakukan pada waktu usia kehamilan 34-37 minggu.
- Operasi caesar darurat juga segera dilakukan jika ketuban pecah lebih awal atau janin dalam kondisi gawat serta terdapat perdarahan yang keluar dari vagina.
- Dokter juga akan menjelaskan kepada Ibu mengenai risiko dan manfaat pengaturan waktu persalinan sebagai langkah mengurangi risiko komplikasi kehamilan yang dapat terjadi pada kondisi vasa previa.
- Pada kondisi vasa previa, dokter dapat menyarankan untuk menghindari hubungan seksual sementara waktu.
Langkah tatalaksana di atas dapat dilakukan dengan menyesuaikan kondisi kehamilan Ibu, riwayat kesehatan Ibu, kondisi janin dan beberapa faktor lainnya.
Komplikasi
Komplikasi yang paling dikhawatirkan pada vasa previa yaitu pecahnya selaput ketuban. Kondisi ini menyebabkan pembuluh darah yang tidak dilindungi oleh selaput juga akan pecah, sehingga terjadi perdarahan pada janin.
Jika Anda tertarik untuk membaca lebih lanjut mengenai pecahnya ketuban, Anda dapat membacanya di sini: Ketuban Pecah Dini (KPD) - Pengertian, Penyebab, Gejala, dan Pengobatan.
Selain itu, vasa previa yang tidak terdeteksi lebih dini saat kehamilan hingga proses persalinan meningkatkan terjadinya perdarahan jalan lahir dan terjadi kondisi gawat pada janin. Ketika perdarahan pada janin sudah terjadi, maka meningkatkan risiko kematian janin akibat banyaknya kehilangan darah yang dialami oleh janin. Kematian janin selama kehamilan juga sangat tinggi terjadi apabila vasa previa tidak didiagnosis hingga persalinan tiba.
Pencegahan
Risiko terjadinya vasa previa tidak dapat dicegah. Namun Ibu dapat mencegah komplikasi yang dapat terjadi dari vasa previa dengan melakukan pemeriksaan kehamilan secara rutin. Deteksi dini vasa previa selama hamil dapat meningkatkan kelangsungan hidup bayi.
Kapan Harus ke Dokter?
Apabila Ibu sedang hamil dan mengalami perdarahan dari vagina berwarna merah gelap disertai dengan nyeri ringan pada vagina. Sebaiknya Ibu segera ke Instalasi Gawat Darurat (IGD) terdekat untuk memperoleh penanganan segera.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Anita Larasati Priyono
Diagnosis and management of vasa previa – Society for maternal fetal medicine (2022). Retrieved 5 November 2022, from https://www.smfm.org/publications/215-diagnosis-and-management-of-vasa-previa
Vasa Previa – Clevelandclinic. (2022). Retrieved 5 November 2022, from https://my.clevelandclinic.org/health/diseases/23465-vasa-previa
Brennan D. What Is Vasa Previa? – WebMD. (2022). Retrieved 5 November 2022, from https://www.webmd.com/baby/what-is-vasa-previa
Dulay AT. Vasa Previa – MSD Manual Professional Version. (2022). Retrieved 5 November 2022, from https://www.msdmanuals.com/professional/gynecology-and-obstetrics/abnormalities-of-pregnancy/vasa-previa
Rainfod M. What Is Vasa Previa? – Verywellhealth. (2022). Retrieved 5 November 2022, from https://www.verywellhealth.com/vasa-previa-5176482