Definition
Acne vulgaris, commonly known as acne, is a chronic skin condition prevalent among individuals. This condition occurs due to the blockage of hair follicles or pores by excess oil and dead skin cells. Acne typically affects adolescents, though it can also manifest in other age groups.
Causes
Four primary factors contribute to acne:
- Excessive sebum or oil production
- Hair follicles clogged by oil and dead skin cells
- Bacteria
- Inflammation
Acne usually appears on the face, forehead, chest, upper back, and shoulders, areas with the highest concentration of oil glands. Hair follicles connected to these glands can become obstructed by excess oil.
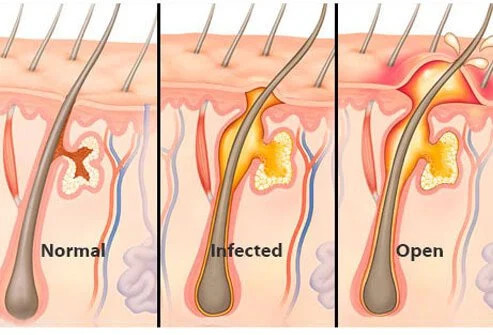
A blocked follicle wall may protrude and result in whiteheads or closed comedones. Alternatively, the blockage may open to the skin's surface, darkening and forming blackheads. These comedones might resemble dirt lodged in pores, but in reality, they are obstructed by bacteria and oil, which darken upon exposure to air.
Acne can also manifest as papules, which are small red bumps, or pustules, red bumps with pus at their tips. Acne develops when hair follicles become blocked, leading to inflammation or bacterial infection. Deeper blockages and inflammation within hair follicles can result in nodules, large, solid, painful bumps under the skin. Other pores on the skin, which are openings of sweat glands, typically do not develop acne.
Certain factors can trigger or exacerbate acne, such as:
- Hormonal changes, particularly during puberty in both boys and girls. This causes enlargement of oil glands and increased sebum production. Hormonal shifts in middle age, particularly in women, can also contribute to acne.
- Certain medications, such as corticosteroids, testosterone, or lithium.
- Diet. Consumption of specific foods, including high-carbohydrate foods, can worsen acne.
- Stress. While stress does not directly cause acne, it can aggravate existing acne.
Risk factor
Risk factors for acne include:
- Age. Acne can affect individuals of all ages but is most commonly experienced during adolescence.
- Hormonal changes. These changes typically occur during puberty or pregnancy.
- Family history. Genetics play a role in acne; if both parents have acne, there is a higher likelihood of developing it.
- Exposure to oily substances. Skin exposed to oily lotions or creams may develop acne.
- Friction or pressure on the skin. This can be caused by items like telephones, cell phones, helmets, tight collars, or backpacks.
Symptoms
Symptoms of acne vary depending on its severity:
- Whiteheads: Closed pores blocked with debris.
- Blackheads: Open pores filled with oxidized debris.
- Papules: Small, red, tender bumps.
- Pustules: Pimples with pus at their tips.
- Nodules: Large, painful, solid lesions under the skin.
- Cysts: Painful, pus-filled lumps under the skin.
Acne typically appears on the face, forehead, chest, upper back, and shoulders.
Diagnosis
Doctors diagnose acne through a skin examination. They also inquire about several risk factors such as experiencing stress or having a family history of acne.
Teenage girls and women will also be asked about their menstrual cycle as it relates to hormonal changes. Sudden and severe acne in older adults may sometimes indicate underlying conditions that require medical attention.
Acne is classified based on its severity into:
- Grade 1 (mild). Predominantly whiteheads and blackheads with some papules and pustules.
- Grade 2 (moderate or pustular acne). Numerous papules and pustules across much of the face.
- Grade 3 (moderately severe or nodulocystic acne). Many papules and pustules along with occasionally inflamed nodules. The back and chest may also be affected.
- Grade 4 (severe cystic nodular acne). Numerous large, painful, and inflamed pustules and nodules.
Management
If you have tried over-the-counter acne products for several weeks without improvement, consult a doctor for further treatment. A dermatologist can assist you in:
- Managing acne
- Preventing the formation of scars or other skin damage
- Reducing the visibility of scars Acne medications work by reducing oil production, inflammation, or treating bacterial infections.
It may take months or even years for your acne to completely disappear. The choice of treatment recommended by your doctor depends on your age, as well as the type and severity of your acne.
Commonly used treatments involve a combination of topical (applied to the skin) and oral medications. Treatment options for pregnant women are limited due to the risk of side effects. Consult with your doctor regarding the risks and benefits of the medications you choose. Make follow-up appointments with your doctor every 3-6 months until your skin improves.
Topical Medications
The most common prescription topical medications for acne include:
- Retinoids and retinoid-like drugs, which are useful for preventing hair follicle blockage in moderate acne. These medications require a doctor's prescription. Do not apply retinoids simultaneously with benzoyl peroxide. Topical retinoids increase skin sensitivity to sunlight and can cause dryness and redness, particularly in individuals with darker skin tones.
- Antibiotics kill excess skin bacteria and reduce inflammation. In the first few months, they can be used in conjunction with retinoids. Antibiotics are applied in the morning and retinoids at night. Antibiotics are often combined with benzoyl peroxide to reduce antibiotic resistance. Topical antibiotics alone are not recommended.
- Azelaic acid and salicylic acid. Azelaic acid is a natural acid produced by fungi and has antibacterial properties. A 20% azelaic acid cream or gel is effective when used twice daily. Azelaic acid is a preferred option for pregnant and breastfeeding patients. This medication is also used to address skin discoloration that occurs with certain types of acne. Meanwhile, salicylic acid can prevent hair follicle blockage. Side effects of both include skin color changes and mild skin irritation.
Oral medication
- Antibiotics, for moderate to severe acne. They should be used for as short a duration as possible and must be combined with other medications, such as benzoyl peroxide, to reduce the risk of antibiotic resistance. Severe side effects are rare. These medications increase skin sensitivity to sunlight.
- Combined oral contraceptives, which are a combination of progesterone and estrogen hormones. Effects may not be noticeable for several months, so additional acne medications may be needed in the first few weeks. Side effects include weight gain, breast tenderness, and nausea. This medication is also associated with an increased risk of heart problems, breast cancer, and cervical cancer.
- Isotretinoin, a derivative of vitamin A, for moderate to severe acne that does not respond to other treatments. Side effects include inflammatory bowel disease, depression, and severe birth defects. Individuals taking isotretinoin should have regular check-ups with a doctor to monitor side effects.
Therapies
For some individuals, the following therapies can help, either alone or in combination with medications:
- Light therapy. Most require several visits.
- Chemical skin peels, used for mild acne. This is done by applying chemical solutions, such as salicylic acid, glycolic acid, or retinoic acid.
- Drainage and extraction, used to remove blackheads or cysts that have not responded to topical treatment. This technique can cause scarring in some individuals.
- Steroid injections, usually for nodular and cystic types. This therapy provides rapid improvement and reduces pain. Side effects include skin thinning and changes in skin color in the treated areas.
Lifestyle and Home Treatments
Several simple steps can help prevent worsening acne:
- Cleanse acne-prone areas with lukewarm water and a gentle cleanser twice daily. If your hair is oily, shampoo daily. Avoid products like facial scrubs, astringents, and masks as they can irritate the skin and worsen acne. Overwashing and scrubbing the face can also irritate the skin. Use over-the-counter acne products to dry excess oil and promote exfoliation.
- Look for products containing benzoyl peroxide, salicylic acid, glycolic acid, or alpha hydroxy acids. These non-prescription acne treatments may cause initial side effects such as redness and dryness, which may improve after the first month of use.
- Avoid irritants such as oily cosmetics, sunscreen, hair styling products, or acne concealers as they can exacerbate acne. Use water-based or non-comedogenic labeled products as they are less likely to cause acne.
- Protect your skin from the sun. Sunlight can worsen skin discoloration after acne clears. Some acne medications also make the skin more susceptible to sunburn. Use non-comedogenic moisturizers and sunscreen regularly.
- Avoid friction or pressure on the skin. Protect acne-prone skin from contact with phones, helmets, tight collars or straps, and backpacks. Avoid touching acne-prone areas as it can trigger more acne, infections, or scarring.
- Shower after strenuous activity as sweat and oil on the skin can lead to acne outbreaks.
Complications
Complications include psychological problems and skin changes. Skin changes that occur include:
- Acne scars, can be in the form of pitted or thickened skin (keloids). Can last long after acne heals.
- Changes in skin color, such as skin color becoming darker (hyperpigmentation) or lighter (hypopigmentation) than before acne.
Prevention
Preventing acne tends to be difficult during hormonal changes. However, the following can help reduce the risk:
- Wash your face every day with warm water and a gentle facial cleanser
- Regularly use moisturizer
- You don't have to stop using makeup, but use non-comedogenic products and remove makeup after use
- Keep your hands away from your face and don't pick at acne
When to see a doctor?
If self-treatment is not effective, consult a doctor or dermatologist to get more appropriate medication. Seek emergency medical help if you experience the following after using a skin product:
- Fainting
- Difficulty breathing
- Swelling of the eyes, face, lips or tongue
Looking for more information about other diseases, Click here!
- dr Anita Larasati Priyono
Acne. (2020). Retrieved 23 March 2022, from https://www.mayoclinic.org/diseases-conditions/acne/symptoms-causes/syc-20368047
Rao J. (2020). Acne vulgaris. Retrieved 23 March 2022, from https://emedicine.medscape.com/article/1069804-overview
Acne. (2020). Retrieved 23 March 2022, from https://my.clevelandclinic.org/health/diseases/12233-acne#prevention
Sutaria AH, Masood S, Schlessinger J. (2021). Acne Vulgaris. Retrieved 23 March 2022, from https://www.ncbi.nlm.nih.gov/books/NBK459173/
Palmer A. (2022). An overview of acne vulgaris. Retrieved 23 March 2022, from https://www.verywellhealth.com/what-is-acne-vulgaris-15492