Definisi
Dermatitis herpetiformis (DH, Duhring disease, the gluten rash) adalah kondisi kulit yang bersifat kronis atau terjadi dalam waktu yang lama, berupa benjolan dan luka lepuh yang terasa gatal akibat alergi terhadap gluten. Gluten adalah protein yang terkandung pada biji-bijian, padi, dan gandum (wheat). Berdasarkan asal katanya, "dermatitis" berarti peradangan pada kulit, sedangkan "herpetiformis" mengacu pada bentuk peradangan yang terdiri atas kulit yang melepuh (blister). Sekalipun memiliki nama yang mirip dengan penyakit herpes, dermatitis herpetiformis tidak disebabkan oleh virus. Kesamaan antara keduanya adalah bentuk peradangan pada kulit.
Dermatitis herpetiformis sering ditemukan di Eropa. Salah satu studi menunjukkan bahwa sekitar 75 dari 100.000 orang di Eropa Utara mengalami dermatitis herpetiformis. Dermatitis herpetiformis juga dialami oleh 10–25% pasien dengan penyakit seliak (celiac disease). Penyakit ini jarang dialami oleh keturunan Afrika-Amerika atau Asia.
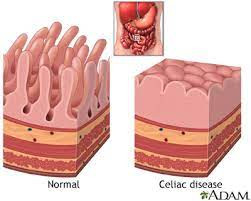
Hampir seluruh pasien dermatitis herpetiformis mengalami penyakit seliak, walaupun tidak bergejala. Dermatitis herpetiformis seringkali disebut sebagai gejala kulit dari penyakit seliak. Gejala utama dari penyakit seliak adalah diare, rasa lelah berkepanjangan, penurunan berat badan, dan nyeri perut berulang.
Penyebab
Pasien dengan dermatitis herpetiformis memiliki reaksi autoimun setiap mengonsumsi gluten. Gluten terdapat pada serealia yang menjadi bahan dasar makanan seperti roti, pasta, kue, dan sereal. Pada kondisi autoimun, tubuh salah mengira suatu senyawa yang biasanya dianggap normal, sebagai sesuatu yang asing dan berbahaya. Di sini, gluten dianggap sebagai senyawa berbahaya oleh tubuh sehingga sistem kekebalan tubuh akan menyerang sel-sel sehat di tubuh. Setiap gluten dicerna oleh tubuh, sistem imun akan aktif dan menghasilkan antibodi (IgA) yang disimpan di kulit. Hal ini menyebabkan rasa gatal, benjolan kemerahan, ruam, atau lepuh pada kulit. Karena disebabkan oleh reaksi sistem kekebalan tubuh terhadap gluten, dermatitis herpetiformis bukan merupakan penyakit yang menular.
Tidak semua orang memiliki sensitivitas tinggi terhadap gluten, sehingga para ahli menduga faktor genetik memiliki peranan yang penting dalam timbulnya dermatitis herpetiformis. Kemungkinan seseorang mengalami dermatitis herpetiformis dan/atau penyakit seliak lebih tinggi jika memiliki keluarga dengan penyakit tersebut. Hal ini dikarenakan penyakit ini berkaitan dengan gen HLA-DQ2 yang diturunkan ke keturunan selanjutnya.
Faktor Risiko
Dermatitis herpetiformis dapat dialami segala usia, namun lebih sering dialami oleh orang-orang di antara usia 30-40 tahun. Laki-laki yang mengalami dermatitis herpetiformis lebih sering mengalami masalah mulut dan kelamin dibandingkan dengan perempuan. Anda juga memiliki risiko yang lebih tinggi untuk mengalami dermatitis herpetiformis jika Anda memiliki anggota keluarga inti dengan dermatitis herpetiformis (risiko meningkat 5% dibandingkan yang tidak memiliki riwayat keluarga).
Pasien dermatitis herpetiformis juga seringkali memiliki keluarga dengan riwayat penyakit autoimun lainnya, seperti:
- Gangguan Tiroid
- Vitiligo, bercak-bercak putih pada kulit karena kulit kehilangan sel pigmen melanosit
- Diabetes Tipe 1
- Alopesia Areata, kebotakan rambut akibat penyakit autoimun
- Penyakit Addison, gangguan yang terjadi ketika kelenjar adrenal tidak menghasilkan hormon yang cukup di tubuh
Gejala
Gejala dari dermatitis herpetiformis antara lain:
1. Kondisi Kulit
Perubahan pada kulit merupakan gejala utama dari dermatitis herpetiformis. Perubahan kulit tersebut adalah adanya bagian kulit yang bentol-bentol, gatal, terasa panas, dan melepuh. Tampilan kulit ini dapat ditemukan di area siku, bokong, lutut, dan kulit kepala. Karena gatal dan digaruk, tampilan kulit pada dermatitis herpetiformis dapat berubah menjadi kerak kuning akibat pecahnya lepuhan atau bekas luka. Sekitar 10-25% pasien dermatitis herpetiformis juga mengalami kerontokan rambut.
2. Kondisi Mulut
Dermatitis herpetiformis dapat menyebabkan masalah pada enamel gigi (selubung tipis yang melapisi gigi), seperti perubahan warna gigi, lekukan horizontal pada gigi, dan sariawan berulang.
3. Gangguan Pencernaan
Penyakit seliak menyebabkan peradangan dan merusak usus halus Anda. Hampir seluruh penderita dermatitis herpetiformis alergi terhadap gluten dan memiliki penyakit seliak. Penyakit seliak dapat menyebabkan keluhan terkait saluran cerna, seperti diare berulang, kram, kembung, begah, konstipasi, dan nyeri.
Gejala dermatitis herpetiformis akan terus muncul selama penderitanya mengonsumsi gluten. Lodium, atau makanan yang mengandung yodium, seperti rumput laut atau beberapa produk kosmetik, dapat memperparah ruam kemerahan pada kulit. Beberapa ahli menganjurkan untuk menghindari konsumsi garam.
Gejala dermatitis herpetiformis juga dapat hilang timbul secara spontan. Hanya sekitar 12% pasien dengan dermatitis herpetiformis yang mengalami remisi atau perbaikan gejala (2 tahun tanpa gejala kulit apapun) secara spontan (tanpa pengobatan). Sekalipun telah mengalami remisi, pasien dermatitis herpetiformis tetap dianjurkan untuk mengonsumsi diet bebas gluten. Kemerahan dan melepuh pada kulit dapat meninggalkan bekas yang lebih gelap atau lebih pucat dibandingkan warna kulit asli.
Diagnosis
Karena tampilan pada kulit yang tidak khas, dermatitis herpetiformis dapat terlihat seperti herpes, skabies, atau berbagai jenis dermatitis lainnya. Oleh karena itu, untuk menegakkan diagnosis dermatitis herpetiformis, Anda perlu melakukan beberapa pemeriksaan yang dilakukan oleh tenaga profesional.
Dokter akan menanyakan beberapa hal mengenai gejala yang dialami, riwayat keguguran berulang yang kadang ditemukan pada penderita penyakit seliak, riwayat sariawan berulang, gangguan kulit dan kuku, dan gejala lain yang juga dapat muncul pada penyakit seliak.
Setelah melihat bentuk dan pola tampilan kulit Anda, dokter Anda dapat melakukan pemeriksaan biopsi kulit dan/atau pemeriksaan darah untuk menentukan apakah Anda mengalami dermatitis herpetiformis atau tidak. Pemeriksaan biopsi kulit dilakukan dengan mengambil beberapa sampel kulit untuk diperiksa di laboratorium. Pewarnaan khusus akan diberikan untuk membantu pemeriksa melihat kumpulan antibodi yang berperan dalam dermatitis herpetiformis. Sementara pemeriksaa darah bertujuan untuk melihat adanya penanda penyakit seliak, yaitu antibodi anti-endomysial dan anti-tissue transglutaminase. Dokter juga dapat memantau kadar vitamin dan mineral pada darah yang biasanya menurun pada penyakit seliak.
Pemeriksaan penunjang di atas akan membantu menegakkan diagnosis dermatitis dan menentukan jenis dermatitis yang Anda alami. Jika pada pemeriksaan biopsi kulit dermatitis herpetiformis dapat ditegakkan dan pada pemeriksaan darah didapatkan antibodi tersebut, kemungkinan besar Anda memiliki penyakit seliak dan dermatitis herpetiformis.
Tata Laksana
Untuk meredakan gejala gatal dan terbakar, Anda dapat mengonsumsi obat pereda peradangan (kortikosteroid, dapsone) yang diresepkan oleh dokter. Obat antiradang ini dapat membantu mengurangi gejala gatal dalam 48 jam. Anda perlu mengonsumsi obat tersebut setidaknya selama 1-2 tahun untuk mencegah dermatitis herpetiformis kembali muncul. Selama pengobatan, Anda perlu melakukan pemeriksaan darah rutin untuk melihat efek samping pengobatan.
Pengobatan utama dari dermatitis herpetiformis adalah mengonsumsi diet bebas gluten. Efek dari diet bebas gluten dapat terlihat setelah beberapa bulan. Anda perlu berkonsultasi dengan ahli gizi untuk menyusun menu diet khusus tersebut. Diet bebas gluten dapat membantu dalam beberapa hal berikut:
- Membantu Anda lepas dari obat kortikosteroid
- Menurunkan risiko mengalami penyakit autoimun lainnya
- Menurunkan risiko mengalami limfoma (kanker kelenjar getah bening)
- Mengurangi gejala
- Memperbaiki nutrisi dan meningkatkan kepadatan tulang
Komplikasi
Dermatitis herpetiformis dapat meninggalkan bekas pada kulit setelah gejala mereda. Bekas luka ini dapat berwarna lebih gelap atau lebih terang dibandingkan kulit asli.
Secara umum, dermatitis herpetiformis dapat terkontrol dengan diet bebas gluten dan obat antiradang. Namun, penyakit seliak yang menyertai dermatitis herpetiformis seringkali mengalami perburukan menjadi kanker usus. Dengan diet bebas gluten yang ketat selama 5-10 tahun, Anda dapat mencegah timbulnya kanker kelenjar getah bening (limfoma).
Pencegahan
Anda perlu memperhatikan komposisi pada setiap makanan yang Anda konsumsi. Anda dapat mencegah timbulnya dermatitis herpetiformis dengan tidak mengonsumsi makanan yang mengandung gluten, seperti:
- Gandum
- Bir
- Pasta dan mie
- Roti (croissant, bagel)
- Kue (muffin, brownies)
- Donat
- Pancake dan makanan lainnya
Kapan Harus ke Dokter?
Segera kunjungi fasilitas kesehatan terdekat jika Anda mengalami gejala-gejala yang mengarah ke dermatitis herpetiformis. Kasus ini akan ditangani oleh dokter spesialis kulit dan kelamin. Dermatitis herpetiformis dapat menyebabkan rasa gatal dan sensasi terbakar yang mengganggu aktivitas sehari-hari. Dokter akan memeriksakan kondisi Anda dan memberikan obat-obatan untuk meredakan gejala.
Jika Anda sudah terdiagnosis dermatitis herpetiformis dan mengalami perburukan walaupun telah mengkonsumsi diet bebas gluten serta obat-obatan, segera periksakan diri ke dokter.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Hanifa Rahma
Antiga, E., Maglie, R., Quintarelli, L., Verdelli, A., Bonciani, D., Bonciolini, V., & Caproni, M. (2019). Dermatitis Herpetiformis: Novel Perspectives. Frontiers in immunology, 10, 1290. https://doi.org/10.3389/fimmu.2019.01290
Cleveland clinic. (2020). Dermatitis herpetiformis. Available from: https://my.clevelandclinic.org/health/diseases/21460-dermatitis-herpetiformis
Nazario B. (2020). Dermatitis herpetiformis. WebMD. Available from: https://www.webmd.com/skin-problems-and-treatments/what-is-dermatitis-herpetiformis
Peraza DM. (2022). Dermatitis herpetiformis. MSD Manual Consumer version. Available from: https://www.msdmanuals.com/home/skin-disorders/blistering-diseases/dermatitis-herpetiformis