Definisi
Granuloma piogenik merupakan tumor jinak pembuluh darah yang tumbuh pada jaringan seperti kulit dan selaput lendir seperti mulut. Walaupun jarang, tumor ini juga bisa ditemukan dalam saluran cerna. Nama lain dari granuloma piogenik adalah hemanigoma kapiler lobularis.
Granuloma piogenik yang timbul pada selaput lendir mulut pada wanita hamil disebut dengan granuloma kehamilan, granuloma gravidarum, atau epulis gravidarum, umumnya terjadi di trimester kedua atau ketiga. Tumor jinak ini terlihat seperti satu benjolan kecil berwarna merah yang halus. Benjolannya mudah berdarah karena terdapat banyak pembuluh darah di dalamnya. Jarang sekali granuloma piogenik dikaitkan dengan infeksi, dan tidak terdapat sel darah putih atau nanah di dalam benjolannya.
Penyebab
Terdapat beberapa penyebab yang diperikarakan dapat menimbulkan granuloma piogenik. Namun, penyebab pastinya belum diketahui sampat saat ini. Faktor seperti riwayat infeksi sebelumnya dan kelainan bentuk pembuluh darah yang sudah ada diduga memiliki kemungkinan untuk menyebabkan penyakit ini.
Granuloma piogenik sering timbul setelah cedera ringan pada tangan, lengan, atau wajah. Cedera ini mencetuskan timbulnya reaksi peradangan pada jaringan. Namun, penelitian yang ada menunjukkan bahwa hanya 7% dari granuloma piogenik yang berhubungan dengan adanya riwayat cedera.
Beberapa hal lain yang juga dapat mencetuskan timbulnya granuloma piogenik adalah:
1. Faktor Hormonal
Hormon tampaknya memiliki peran pada granulomaa piogenik yang terjadi pada wanita hamil. Terdapat kenaikan angka penyakit pada wanita, terutama saat usia hamil. Diperkirakan bahwa estrogen dan hormon seks lainnya mencetuskan respon peradangan yang berlebihan pada jaringan gusi, terutama saat kehamilan, sehingga timbul benjolan pada area mulut.
2. Obat-Obatan
Beberapa varian granuloma piogenik menunjukan adanya kaitan dengan konsumsi obat tertentu, dimana ada penelitian yang menyebutkan kemungkinan hampir 30% kasus diasosiasikan dengan obat-obatan. Obat yang paling sering dikaitkan dengan granuloma piogenik adalah:
-
- Obat yang mengandung retinoid, granuloma piogenik yang menyebar luas (jarang sekali) pernah ditemukan terjadi akibat penggunaan isotretinoin pada pasien dengan jerawat kistik berat
- Obat ARV (antriretroviral) yang digunakan pada infeksi HIV/AIDS, misalnya indinavir
- Antineoplastik yang diberikan pada penderita tumor
- Obat penekan sistem kekebalan tubuh
Faktor Risiko
Granuloma piogenik dapat timbul pada seluruh kelompok usia, namun lebih sering ditemui pada anak-anak dan wanita hamil. Laporan yang ada masih memberikan hasil yang berlawanan terkait pola epidemiologi penyakit. Pada sebuah studi yang dilakukan pada anak-anak, ditemukan usia rata-rata penderita berumur 6 - 10 tahun, dengan kecenderungan jenis kelamin laki-laki. Pada penelitian lainnya, rasio penderita pria dan wanita adalah 1:1,2, dimana penderita pria biasanya mengalami penyakit ketika berusia lebih muda. Sementara itu pada pasien wanita yang mengalami penyakit ini ditemukan berusia 30-40 tahun.
Gejala
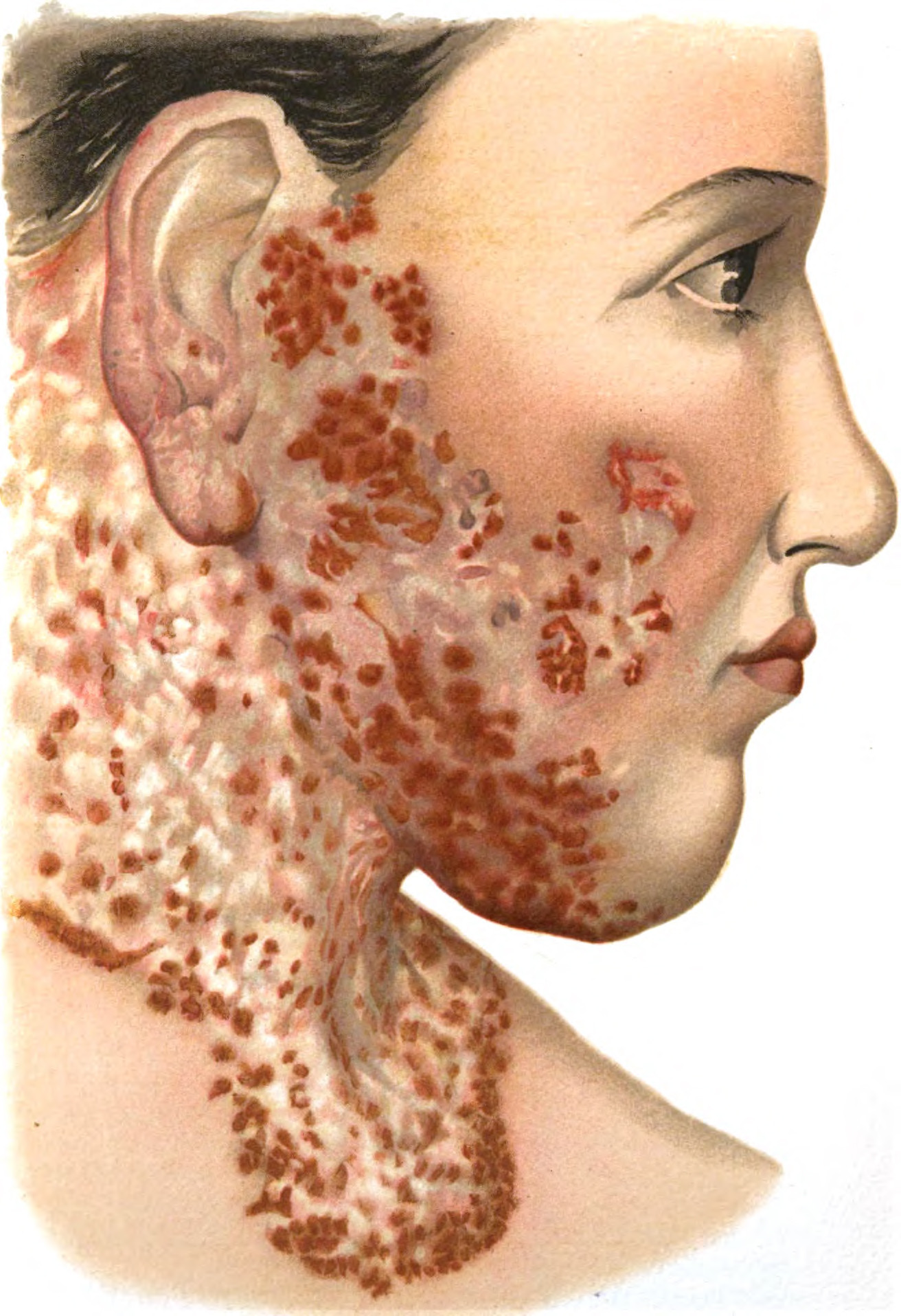
Granuloma piogenik awalnya terlihat sebagai satu benjolan yang kecil, padat, dan berwarna kemerahan, kadang bisa ditemukan anakan benjolan di sekitarnya. Meskipun sangat jarang, dapat timbul benjolan yang menyebar luas di seluruh tubuh.
Benjolan ini kemudian akan mengalami perubahan yang bervariasi, terkadang bertumbuh dengan cepat dalam beberapa minggu sampai beberapa bulan, yang disertai dengan tangkai. Ciri-ciri dari benjolan ini adalah:
- Ukuran dari benjolan biasanya stabil, biasanya berukuran beberapa milimeter sampai sentimeter
- Warnanya dapat bervariasi, dari kemerahan sampai merah kecokelatan atau keunguan
- Pada dasar benjolan dapat ditemukan adanya sisik yang melingkar
- Mudah berdarah
Permukaan granuloma ini sangat rapuh dan mudah berdarah jika terkenda cedera ringan karena terdapat banyak pembuluh darah disitu. Perdarahan ini biasanya mudah kambuh karena adanya cedera yang tidak dapat dihindari maupun dikontrol. Pada beberapa kasus yang jarang, permukaan benjolan dapat mengalami luka (ulkus).
Granuloma piogenik dapat timbul pada bagian kulit atau selaput lendir manapun yang normal. Area yang dapat terkena adalah:
- Badan
- Lengan atas
- Kepala
- Leher
- Tungkai
- Kaki
- Bibir
- Gusi
- Lidah
- Selaput lendir hidung
- Selaput bening mata
- Leher rahim
- Vagina juga
Pada wanita hamil, lokasi paling sering adalah pada pipi bagian dalam dan gusi. Saluran cerna juga dapat terkena, namun jarang. Jika ada, dapat tidak bergejala atau menyebabkan perdarahan tersembunyi (tidak kasa mata) dan menyebabkan kekurangan sel darah merah (anemia). Terkadang, granuloma piogenik tumbuh di bawah kulit, terutama pada wanita, atau di dalam pembuluh darah. Granuloma seperti ini akan tampak sebagai benjolan di bawah kulit yang memiliki batas tegas.
Diagnosa
Dokter akan menanyakan riwayat kesehatan dan gejala yang Anda alami, serta melakukan pemeriksaan fisik untuk mendiagnosa granuloma piogenik. Pada beberapa kasus, dapat dilakukan pemeriksaan dermoskopi. Jika diagnosis belum bisa ditegakkan dengan pemeriksaan tersebut, maka akan dilakukan biopsi kulit untuk mengonfirmasi diagnosa dan menghapus kemungkinan penyakit lain seperti kanker kulit. Pemeriksaan biopsi dengan mengambil sampel jaringan dapat dilakukan dengan prosedur pengangkatan seluruh benjolan dan kemudian diperiksa di laboratorium.
Tata Laksana
Granuloma piogenik sering berdarah dan mengalami luka atau tukak sehingga perlu diobati. Pilihan terapi yang berbeda memberikan tingkat kesuksesan dan kemungkinan kambuh yang bervariasi. Namun begitu, pada terapi apapun tetap ada kemungkinan benjolan ini kambuh.
Granuloma piogenik yang berukuran kecil dapat hilang dengan sendirinya. Namun, benjolan yang berukuran besar perlu diobati. Pilihan terapi tersebut antara lain:
- Bedah eksisi total, yaitu pengangkatan total benjolan granuloma, biasanya dilakukan pada area tubuh yang tidak terlihat. Metode ini memiliki tingkat kekambuhan yang rendah
- Prosedur kuretase yang diikuti dengan elektrokauterisasi, merupakan bedah listrik yang menghancurkan benjolan dan bisa menjadi pilihan untuk area wajah. Namun, tingkat kekambuhannya lebih tinggi.
- Kauterisasi kimia dengan larutan perak nitrat atau krioterapi (terapi beku)
- Terapi laser
Terapi dengan obat-obatan tidak direkomendasikan. Banyak obat oles atau obat suntik yang diberikan langsung pada benjolan namun memberikan respon yang bervariasi. Pada kehamilan atau granuloma yang disebabkan oleh obat, tingkat kekambuhan setelah terapi lebih tinggi. Obat-obatan yang diduga menyebabkan munculnya benjolan ini harus berhenti digunakan, kecuali pada orang yang sedang mendapatkan pengobatan pada tumor dimana terapi tersebut tidak dapat dihentikan.
Kebanyakan granuloma piogenik dapat diangkat dengan prosedur bedah. Bekas luka dapat menetap setelah prosedur. Terdapat risiko tinggi untuk kekambuhan jika tidak seluruh benjolan yang diangkat. Jika kekambuhan terjadi, prosedur eksisi total merupakan terapi yang bisa dipilih.
Komplikasi
Komplikasi yang mungkin terjadi akibat granuloma piogenik adalah:
- Perdarahan
- Luka atau tukak
- Infeksi
- Kekambuhan
- Gangguan kosmetik, yang dapat menjadi sumber stres psikologis pada penderita, terutama jika benjolan terdapat di wajah
Pencegahan
Penyebab pasti granuloma piogenik memang belum diketahui, namun dihubungkan dengan beberapa faktor. Oleh karena itu, hal yang dapat dilakukan untuk mengurangi risiko menderita granuloma piogenik adalah:
- Menghindari atau menghentikan obat-obatan yang berkaitan dengan granuloma piogenik
- Menghindari mencederai kulit, misalnya tindik
- Menjaga kebersihan mulut
- Bersihkan dan tutup luka untuk mencegah infeksi
Kapan Harus ke Dokter?
Jika Anda memiliki benjolan pada kulit yang mudah berdarah, sebaiknya Anda berkonsultasi dengan dokter atau spesialis kulit untuk mendapatkan pengobatan.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Hanifa Rahma
Pyogenic granuloma Information | Mount Sinai - New York. (2022). Retrieved 10 June 2022, from https://www.mountsinai.org/health-library/diseases-conditions/pyogenic-granuloma
Sarwal, P., & Lapumnuaypol, K. (2022). Pyogenic Granuloma. Retrieved 10 June 2022, from https://www.ncbi.nlm.nih.gov/books/NBK556077/
Pyogenic Granuloma: Symptoms, Causes & Treatment. (2022). Retrieved 10 June 2022, from https://my.clevelandclinic.org/health/diseases/22717-pyogenic-granuloma