Definisi
Karsinoma sel basal adalah salah satu tipe kanker pada kulit. Karsinoma sel basal berasal dari sel basal, sebuah sel di dalam kulit yang menghasilkan sel-sel baru untuk menggantikan sel-sel yang mati. Karsinoma sel basal merupakan jenis kanker kulit yang paling sering terjadi pada manusia. Jumlah penderita kanker kulit jenis ini meningkat setiap tahunnya.
Penyebab
Karsinoma sel basal terjadi apabila sel basal pada kulit mengalami mutasi atau perubahan struktur genetik. Sel basal ditemukan pada bagian dasar epidermis (bagian terluar kulit). Sel ini berfungsi untuk membelah diri dan menghasilkan sel-sel baru. Setelah sel-sel baru ini dihasilkan, sel-sel ini mendorong sel-sel lama ke permukaan kulit, hingga pada akhirnya sel-sel lama akan mati dan terkelupas dari kulit. Proses pembelahan diri ini dikontrol oleh gen yang terdapat di dalam sel basal. Gen ini memberikan perintah tertentu untuk setiap sel yang berbeda. Apabila terjadi mutasi gen, sel basal mendapatkan perintah untuk membelah diri secara cepat dan terus berkembang meskipun seharusnya sudah mati. Sel-sel yang tidak normal ini dapat membentuk tumor ganas, yang tampak pada kulit.
Mutasi gen yang menyebabkan karsinoma sel basal diduga berasal dari radiasi sinar ultraviolet, terutama ultraviolet B. Sinar ultraviolet ini berasal dari sinar matahari dan lampu khusus untuk membuat warna kulit menjadi coklat (tanning). Namun, tidak semua penderita karsinoma sel basal sering terpapar sinar matahari. Oleh karena itu, penyebab karsinoma sel basal secara pasti belum diketahui.
Faktor Risiko
Faktor yang dapat meningkatkan risiko karsinoma sel basal adalah sebagai berikut:
- Paparan sinar matahari berkepanjangan. Jika Anda terpapar sinar matahari atau lampu tanning dalam jangka waktu lama, Anda berisiko lebih tinggi untuk mengalami karsinoma sel basal. Risiko akan semakin tinggi apabila Anda tinggal di daerah yang cerah atau cukup tinggi, yang menyebabkan paparan sinar ultraviolet lebih tinggi. Kulit yang terbakar juga meningkatkan risiko kanker.
- Terapi radiasi. Terapi radiasi untuk menangani jerawat atau kondisi kulit lainnya dapat meningkatkan risiko karsinoma sel basal pada bagian yang terkena sinar tersebut.
- Kulit berwarna terang. Risiko karsinoma sel basal lebih tinggi pada orang yang memiliki bintik kemerahan (freckle) pada wajah, orang berkulit putih, orang dengan rambut merah atau pirang, serta orang dengan warna selaput pelangi mata terang.
- Pertambahan usia. Karsinoma sel basal membutuhkan waktu berpuluh-puluh tahun untuk terjadi sehingga penyakit ini umumnya terjadi pada orang berusia lanjut. Namun, penyakit ini dapat terjadi pada dewasa muda dan mulai sering terjadi pada orang-orang berusia 20-an hingga 30-an tahun.
- Riwayat keluarga atau pribadi dengan kanker kulit. Jika Anda sudah pernah mengalami karsinoma sel basal sebelumnya, Anda memiliki risiko lebih tinggi untuk mengalaminya ulang. Jika Anda memiliki riwayat keluarga dengan kanker kulit, Anda berisiko tinggi untuk mengalami karsinoma sel basal.
- Obat-obatan penurun kekebalan tubuh. Obat-obatan yang berfungsi untuk menurunkan kekebalan tubuh biasanya diberikan pada orang-orang yang menjalani cangkok organ atau orang dengan penyakit autoimun (kekebalan tubuh yang menyerang sel diri sendiri). Obat-obatan ini dapat meningkatkan risiko karsinoma sel basal.
- Paparan terhadap arsenik. Arsenik merupakan logam beracun yang banyak ditemukan di lingkungan sekitar. Logam ini meningkatkan risiko karsinoma sel basal dan kanker lainnya. Semua orang pernah terpapar logam ini, namun paparan tersebut meningkat apabila seseorang minum air sumur yang mengandung arsenik atau bekerja dengan logam tersebut.
- Sindrom yang menyebabkan kanker kulit. Penyakit genetik tertentu dapat meningkatkan risiko karsinoma sel basal, misalnya Sindrom Gorlin-Goltz dan xeroderma pigmentosum.
Gejala
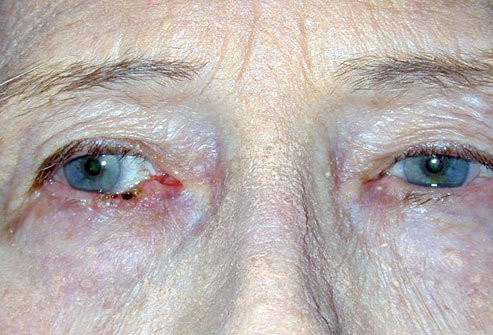
Karsinoma sel basal biasanya terjadi pada kulit yang terpapar sinar matahari, terutama pada bagian wajah dan leher. Karsinoma sel basal tampak berupa perubahan kulit, seperti pertumbuhan atau luka yang tidak kunjung sembuh. Perubahan kulit ini biasanya memiliki ciri sebagai berikut:
- Benjolan sewarna kulit yang berkilau, dan kadang bening. Benjolan ini tampak putih seperti mutiara atau merah mudah pada kulit yang putih. Pada kulit berwarna coklat atau hitam, benjolan ini dapat berwarna coklat atau hitam mengkilat. Pembuluh darah kecil dapat terlihat. Benjolan ini dapat mudah berdarah.
- Luka berwarna coklat, hitam, atau biru atau luka yang memiliki bintik kehitaman, dengan pinggiran meninggi dan bening.
- Plak datar dan bersisik dengan pinggiran meninggi. Seiring waktu, plak ini dapat melebar.
- Penampakan kulit mirip bekas luka, putih, mirip lilin tanpa batas jelas.
Diagnosis
Karsinoma sel basal dapat terdiagnosis pasti dengan bantuan biopsi kulit. Biopsi merupakan pengambilan jaringan kulit dari bagian yang diduga mengalami kanker. Kemudian, jaringan tersebut akan diamati di bawah mikroskop. Dokter dapat menentukan jenis kanker berdasarkan jaringan yang diamati. Selain itu, dokter juga dapat menentukan stadium kanker berdasarkan pemeriksaan pada berbagai organ.
Pemeriksaan yang dapat dilakukan dapat berupa pencitraan. Pencitraan yang disarankan adalah Magnetic Resonance Imaging (MRI), yang sangat baik untuk melihat jaringan. Pemeriksaan ini dapat membantu mencari adanya penyebaran kanker ke kelenjar ludah, otot, jaringan ikat, tulang wajah, mata, atau saraf.
Tata Laksana
Tata laksana karsinoma sel basal tergantung dari usia dan jenis kelamin pasien serta tempat, ukuran, dan tipe luka. Meskipun sama-sama menderita karsinoma sel basal, dua pasien dapat menjalani dua terapi yang berbeda, tergantung subtipe karsinoma sel basal yang dialami. Tujuan utama tata laksana karsinoma sel basal adalah untuk mengangkat tumor sepenuhnya agar tidak terjadi sakit ulang, memperbaiki gangguan fungsi akibat tumor, dan memberikan hasil kosmetik (penampilan) terbaik untuk pasien, karena kanker ini paling banyak terjadi pada wajah.
Karsinoma sel basal biasanya ditangani dengan pembedahan, obat-obatan atau kemoterapi, atau terapi radiasi. Jika pembedahan tidak dapat dilakukan, terapi radiasi dapat menjadi alternatif. Namun, terapi ini lebih mahal, hasil kosmetik yang kurang baik, waktu terapi yang lebih panjang (15-30 kali kunjungan), dan peningkatan risiko kanker kulit di masa depan.
Selain itu, alternatif tata laksana lainnya adalah krioterapi. Krioterapi adalah sebuah prosedur yang dilakukan dengan membekukan jaringan kanker agar jaringan tersebut mati.
Komplikasi
Karsinoma sel basal merupakan tumor ganas, namun penyebarannya ke organ lain cukup sedikit. Komplikasi karsinoma sel basal dapat berupa:
- Risiko sakit ulang. Karsinoma sel basal sering terjadi ulang, meskipun terapi sebelumnya telah berhasil.
- Peningkatan risiko kanker kulit lainnya. Riwayat karsinoma sel basal dapat meningkatkan risiko kanker kulit lainnya, seperti karsinoma sel skuamosa.
- Penyebaran kanker ke daerah selain kulit (metastasis). Pada karsinoma sel basal, hal ini sangat jarang terjadi. Namun, kanker memiliki kemungkinan untuk menyebar ke organ lainnya seperti kelenjar getah bening, tulang, dan paru.
Pencegahan
Beberapa langkah pencegahan karsinoma sel basal adalah sebagai berikut:
- Menghindari sinar matahari di tengah hari. Pada banyak tempat, sinar matahari terkuat terjadi pada jam 10 pagi hingga jam 4 sore. Anda dapat menjadwalkan aktivitas di luar rumah saat musim dingin atau ketika langit berawan.
- Menggunakan tabir surya. Gunakan tabir surya dengan Sun Protection Factor (SPF) 30 atau lebih. Anda dapat mengoleskan tabir surya setiap dua jam sekali, atau lebih sering lagi jika Anda berenang atau berjemur.
- Menggunakan baju tertutup. Anda dapat menutupi kulit Anda dengan pakaian panjang yang menutupi tangan dan kaki, serta menggunakan topi bertepi lebar.
- Menghindari penggunaan mesin tanning.
- Memeriksakan kulit secara rutin dan melaporkan perubahan kepada dokter. Periksalah kulit Anda secara rutin untuk mencari adanya pertumbuhan kulit atau perubahan tahi lalat yang sudah ada.
Kapan Harus ke Dokter?
Anda dapat berkonsultasi kepada dokter jika Anda mengamati adanya perubahan pada kulit Anda, misalnya seperti pertumbuhan kulit baru, perubahan pada benjolan kulit yang sudah ada sebelumnya, atau luka yang tidak kunjung sembuh.
Mau tahu informasi seputar penyakit pada kulit lainnya? Yuk, baca lebih banyak artikelnya di sini!
- dr Ayu Munawaroh, MKK
Bader, R. (2022). Basal Cell Carcinoma: Practice Essentials, Background, Pathophysiology. Retrieved 19 March 2022, from https://emedicine.medscape.com/article/276624-overview
Basal cell carcinoma - Symptoms and causes. (2021). Retrieved 19 March 2022, from https://www.mayoclinic.org/diseases-conditions/basal-cell-carcinoma/symptoms-causes/syc-20354187
McDaniel, B., Badri, T., & Steele, R. (2021). Basal Cell Carcinoma. Retrieved 19 March 2022, from https://www.ncbi.nlm.nih.gov/books/NBK482439/