Definisi
Melanoma adalah salah satu jenis kanker kulit, di mana terdapat pertumbuhan melanosit (sel yang menghasilkan pigmen warna kulit/melanin) yang tidak terkendali. Melanoma termasuk jenis kanker kulit ganas yang cukup serius. Diperkirakan sekitar 17% hingga 20% penderita melanoma akan mengembangkan lebih dari satu melanoma sehingga disebut juga dengan melanoma multipel. Melanoma multipel biasanya dapat ditemukan dalam kisaran waktu 0 hingga 6 bulan sejak diagnosis melanoma yang pertama dengan yang berikutnya. Risiko terjadinya melanoma multipel tampaknya lebih tinggi pada tahun pertama setelah diagnosis melanoma pertama dan akan tetap meningkat setidaknya selama 20 tahun.
Melanoma pada dasarnya dapat berkembang di mana saja pada kulit, tetapi biasanya lebih cenderung terjadi di batang tubuh (dada dan punggung) pada pria dan di kaki pada wanita. Leher dan wajah juga termasuk lokasi umum ditemukannya melanoma. Selain itu, melanoma juga bisa terbentuk di mata dan pada kasus yang sangat jarang, dapat ditemukan di hidung atau tenggorokan.
Melanoma termasuk kasus kanker kulit yang lebih jarang ditemukan daripada beberapa jenis kanker kulit lainnya, yaitu hanya sekitar 1% dari kanker kulit. Akan tetapi, melanoma bersifat lebih berbahaya karena lebih mungkin menyebar ke bagian tubuh lain jika tidak dideteksi dan diobati sejak dini.
Penyebab
Perkembangan terjadinya melanoma dimulai ketika terdapat gangguan pada sel penghasil melanin (melanosit) yang memberi warna pada kulit Anda. Pada keadaan normal, sel-sel kulit akan berkembang dengan cara yang terkendali dan teratur, di mana sel-sel baru yang sehat akan mendorong sel-sel yang lebih tua ke atas permukaan kulit sehingga pada akhirnya mereka akan mati dan rontok. Akan tetapi, ketika beberapa sel mengalami kerusakan pada DNA, sel-sel baru mungkin akan mulai tumbuh di luar kendali dan pada akhirnya dapat membentuk suatu massa sel kanker.
Kebanyakan ahli setuju bahwa penyebab utama yang mungkin berperan terhadap timbulnya melanoma adalah paparan terhadap sinar matahari yang berlebihan, terutama kulit yang terbakar saat Anda masih muda. Data statistik menunjukkan bahwa sebanyak 86% melanoma disebabkan oleh sinar ultraviolet (UV) matahari. Paparan sinar UV dapat menyebabkan kerusakan pada DNA sel sehingga membuat perubahan pada gen tertentu yang memengaruhi bagaimana sel tumbuh dan membelah di luar kendali. Penggunaan lampu untuk tanning juga diduga berperan terhadap timbulnya kerusakan DNA pada kulit.
Namun, sinar UV tidak selalu menyebabkan semua melanoma, mengingat melanoma dapat terjadi di tempat-tempat di tubuh yang tidak menerima paparan sinar matahari. Hal ini menunjukkan terdapat faktor lain yang mungkin berperan terhadap timbulnya melanoma. Diperkirakan terdapat kombinasi berbagai faktor, termasuk faktor lingkungan dan genetik yang juga berkontribusi dalam perkembangan melanoma.
Faktor Risiko
Faktor-faktor yang dapat meningkatkan risiko Anda mengalami melanoma multipel meliputi:
- Memiliki riwayat melanoma sebelumnya
- Bertambahnya usia
- Memiliki kulit putih, rambut pirang atau merah, dan mata biru
- Memiliki riwayat kulit yang terbakar sinar matahari
- Paparan sinar ultraviolet (UV) yang berlebihan, baik yang berasal dari matahari dan dari lampu tanning
- Tinggal di tempat yang berlokasi lebih dekat dengan garis khatulistiwa atau di ketinggian yang lebih tinggi
- Memiliki banyak tahi lalat, terutama yang bentuknya tidak beraturan
- Memiliki riwayat melanoma dalam keluarga, seperti orang tua, anak, atau saudara kandung
- Memiliki sistem kekebalan tubuh yang melemah, seperti pada penerima transplantasi organ, penderita AIDS, atau sedang mengonsumsi obat-obatan penurun sistem kekebalan tubuh
Gejala
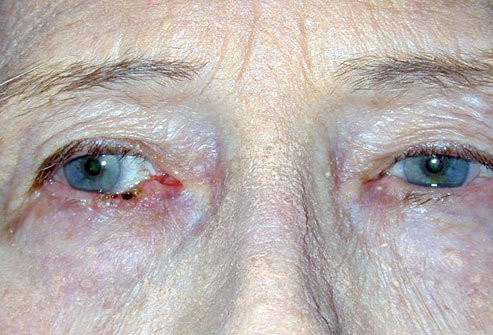
Melanoma dapat berkembang di mana saja di tubuh Anda, dan paling sering terjadi di area yang sering terpapar sinar matahari, seperti punggung, kaki, lengan, dan wajah. Namun, melanoma juga dapat terjadi di area yang tidak banyak terpapar sinar matahari, seperti telapak kaki, telapak tangan, dan di bawah kuku. Melanoma yang terjadi pada lokasi yang tersembunyi ini lebih sering ditemukan pada orang dengan kulit lebih gelap.
Pada melanoma multipel dapat ditemukan lebih dari satu melanoma secara bersamaan pada tubuh Anda. Beberapa melanoma mungkin tidak langsung ditemukan bersamaan dan biasanya dapat ditemukan dalam kurun 6 bulan sejak diagnosis melanoma yang pertama. Beberapa tanda dan gejala awal melanoma yang sering timbul adalah perubahan pada tahi lalat yang sudah ada sebelumnya dan adanya pertumbuhan yang tampak tidak biasa atau perubahan warna pada kulit Anda. Tahi lalat yang tidak biasa mungkin mengindikasikan adanya suatu melanoma. Beberapa karakteristik dari melanoma dapat dilihat dari:
- A (asymmetric) yaitu bentuk tahi lalat yang asimetris dan tidak beraturan, seperti dua bagian yang tampak sangat berbeda.
- B (border) yaitu tahi lalat yang memiliki batas tidak beraturan, berlekuk, atau bergergigi.
- C (colour) yaitu tahi lalat yang mengalami perubahan warna, memiliki banyak warna, atau distribusi warna yang tidak merata. Melanoma dapat tampak berwarna cokelat, hitam, abu-abu, merah, atau putih.
- D (diameter) yaitu tahi lalat yang memiliki diameter lebih besar dari 1/4 inci (sekitar 6 milimeter).
- E (evolving) yaitu tahi lalat yang mengalami perubahan secara terus-menerus, seperti tahi lalat yang semakin melebar atau yang berubah warna atau bentuk. Tahi lalat juga dapat menimbulkan tanda dan gejala baru, seperti rasa gatal atau perdarahan.
Diagnosis
Dalam mendiagnosis melanoma multipel, dokter akan mulai dengan melakukan wawancara dengan Anda. Dokter akan menanyakan gejala-gejala apa saja yang Anda alami, sejak kapan gejala dirasakan, di mana saja timbulnya gejala, faktor-faktor yang mungkin berperan terhadap timbulnya melanoma, serta riwayat melanoma sebelumnya atau pada anggota keluarga. Kemudian, dokter akan melanjutkan dengan melakukan pemeriksaan fisik. Dokter akan melihat langsung tampilan dari area kulit yang terkena. Pada umumnya, melanoma memiliki tampilan klinis yang cukup khas. Untuk membantu menegakkan diagnosis melanoma, dokter akan melakukan pemeriksaan biopsi sebagai gold standard. Pada pemeriksaan biopsi, dokter akan mengambil sedikit sampel jaringan kulit yang terkena untuk diperiksa di bawah mikroskop. Dari hasil pemeriksaan biopsi dapat ditemukan sel-sel melanosit yang mengalami perubahan menjadi ganas. Selain itu, dokter juga mungkin menyarankan beberapa pemeriksaan penunjang, seperti pemeriksaan darah, CT-scan, MRI, atau PET scan untuk menilai penyebaran melanoma ke organ tubuh lainnya.
Tata Laksana
Tata laksana melanoma multipel akan tergantung pada stadium melanoma dan kesehatan umum Anda. Beberapa pilihannya antara lain:
- Pembedahan biasanya merupakan pengobatan utama untuk melanoma. Prosedur ini melibatkan pemotongan area kulit yang terkena dan beberapa kulit normal di sekitarnya. Jumlah kulit sehat yang diangkat akan tergantung pada ukuran dan lokasi melanoma. Pada tahap awal, pembedahan memiliki kemungkinan besar untuk dapat menyembuhkan melanoma.
- Terapi kanker yang ditargetkan. Dalam tata laksana ini, obat digunakan untuk menyerang sel kanker tertentu. Pendekatan "bertarget" ini akan mengejar sel-sel kanker saja dan membiarkan sel-sel sehat tidak terpengaruh.
- Terapi radiasi mencakup tata laksana dengan sinar berenergi tinggi untuk menyerang sel kanker dan mengecilkan tumor.
- Imunoterapi dengan merangsang sistem kekebalan tubuh Anda sendiri untuk membantu melawan kanker.
Komplikasi
Jika ditemukan dan segera ditata laksana dengan tepat, melanoma dapat teratasi dengan cukup baik. Namun, risiko untuk terjadinya melanoma kembali masih akan tetap ada. Selain itu, melanoma juga termasuk kanker kulit yang dapat menyebar ke organ tubuh lainnya jika tidak segera ditangani.
Pencegahan
Beberapa cara yang dapat Anda lakukan untuk mencegah timbulnya melanoma multpel, antara lain:
- Deteksi dini dan tata laksana awal adalah kunci utama untuk mencegah perkembangan melanoma multipel.
- Hindari paparan sinar matahari belebihan, khususnya antara jam 10 pagi hingga 4 sore.
- Jangan gunakan lampu tanning.
- Jika memungkinkan, kenakan topi dengan pinggiran, kacamata hitam, kemeja lengan panjang, dan celana panjang ketika berpergian ke luar rumah.
- Gunakan tabir surya spektrum luas dengan faktor perlindungan kulit (SPF) 30 atau lebih tinggi dan aplikasikan ulang sesering mungkin, biasanya setiap 1,5 jam atau lebih sering jika Anda berenang atau berkeringat.
- Gunakan pelembab bibir dengan kandungan tabir surya.
- Jangan lupa untuk mengoleskan tabir surya pada anak kecil dan bayi di atas 6 bulan.
Kapan Harus ke Dokter ?
Konsultasikan diri Anda ke dokter jika mengalami perubahan pada kulit atau tahi lalat Anda yang tidak biasa.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Nadia Opmalina
American Cancer Society. Melanoma Skin Cancer. (2019). Retrieved 15 Mei 2022, from https://www.cancer.org/cancer/melanoma-skin-cancer.html
CJ Rowe, et al. Survival Outcomes in Patients with Multiple Primary Melanomas. (2015). J Eur Acad Dermatol Venereol.
Claeson, Magdalena, et al. Multiple Primary Melanomas: A Common Occurrence in Western Sweden. (2016). Retrieved 15 Mei 2022, from https://www.medicaljournals.se/acta/content/html/10.2340/00015555-2598
Melanoma. (2022). Retrieved 15 Mei 2022, from https://www.mayoclinic.org/diseases-conditions/melanoma/symptoms-causes/syc-20374884
Melanoma. (2021). Retrieved 15 Mei 2022, from https://my.clevelandclinic.org/health/diseases/14391-melanoma
Oakley, Amanda. Melanoma. (2015). Retrieved 15 Mei 2022, from https://dermnetnz.org/topics/melanoma
Shih, Shawn, et al. Multiple Primary Melanomas Occuring Around the Same Time: A Review of Terminology and Implications. J Drugs Dermatol. 2020;19(5): doi:10.36849/JDD.2020.4953
Ungureanu, Loredana, et al. Multiple Primary Melanomas: Our Experience. (2020). Retrieved 15 Mei 2022, from https://doi.org/10.3892/etm.2020.9520