Definisi
Limfedema merupakan pembengkakan pada berbagai variasi area dari tubuh ketika sistem limfatik terpengaruhi. Sistem limfatik mengumpulkan cairan berlebih, protein dan hasil akhir dari sel dan jaringan lalu mengembalikannya ke dalam aliran darah. Ketika sistem limfatik tidak bekerja dengan baik, tubuh mulai mengumpulkan air dan terjadi pembengkakan. Pembengkakan ini biasanya memengaruhi lengan dan kaki, tetapi dapat memengaruhi area tubuh lainnya.
Kondisi ini juga dapat terjadi setelah operasi tertentu atau kondisi medis atau kondisi genetik tertentu. Limfedema memiliki dua tipe, yaitu limfedema primer dan limfedema sekunder. Limfedema primer jarang terjadi dan biasanya diturunkan dari orang tua. Kondisi ini dapat muncul pada bayi hingga anak remaja hingga orang tua. Pada bayi yang lahir dengan kondisi gangguan Milroy, merupakan kondisi limfedema yang diturunkan.
Limfedema sekunder terjadi ketika sistem limfatik mengalami gangguan, seperti riwayat operasi, trauma atau terapi radiasi. Limfedema umumnya terjadi pada pasien dengan pengobatan kanker payudara, tetapi tidak semua pasien terapi kanker payudara mengalaminya. Limfedema sendiri bukan bentuk dari kanker.
Penyebab
Beberapa penyebab dari limfedema primer pada anak-anak seperti:
- Trauma minor
- Anak-anak dengan limfedema primer memiliki kapasitas yang lebih kecil dalam mengeluarkan cairan limfe. Kapasitas yang mengecil ini baru dapat diketahui setelah adanya trauma minor seperti kaki terkilir sehingga menyebabkan inflamasi akut dan pembengkakan dari sistem limfatik akibat penumpukan cairan. Trauma minor juga dapat menginisiasi limfedema dengan merusak sementara fungsi dari pembuluh darah limfatik.
- Prosedur medis
- Seperti trauma minor, prosedur medis minor dapat menyebabkan pembengkakan dan inflamasi yang menyebabkan muncul gejala limfedema. Gigitan serangga
- Infeksi
- Gigitan serangga dapat menyebabkan pembengkakan lokal dan inflamasi sehingga dapat memicu limfedema
- Gerakan yang terbatas (sedentary periods)
- Tidak bergerak dalam waktu lama seperti selama di pesawat dapat menyebabkan pembengkakan pada kaki
Faktor Resiko
Pasien yang memiliki kanker, terapi radiasi pada area limfe dan tumor memiliki risiko lebih tinggi mengalami limfedema.
Gejala
Perkembangan dari limfedema pada anak memiliki pola yang sama dengan orang dewasa seperti jenis dari limfedema (primer atau sekunder), atau lokasi dimana bagian tubuh terkena. Tahapan dari limfedema dijelaskan melalui skala Foldi.
Gejala dari Limfedema meliputi
- Adanya pembengkakan pada beberapa atau sebagian lengan atau kaki, meliputi jari-jari kaki atau jempol
- Adanya rasa sesak atau ketat
- Gerakan menjadi terbatas
- Infeksi yang kambuh kembali, kulit yang mengeras dan menebal
Gejala tersebut dapat bervariasi dari sedang hingga parah. Limfedema yang disebabkan oleh terapi kanker biasanya bersifat sementara.
Diagnosis
Dokter akan melakukan beberapa pemeriksaan untuk menentukan diagnosis limfedema. Pemeriksaan meliputi anamnesis atau wawancara medis, pemeriksaan fisik dan pemeriksaan penunjang.
Wawancara Medis
Dokter akan bertanya mengenai:
- Gejala yang dialami saat ini
- Riwayat penyakit dahulu
- Riwayat penyakit keluarga
- Riwayat trauma atau operasi
Pemeriksaan Fisik
Setelah wawancara medis, dokter akan melakukan pemeriksaan fisik secara umum seperti pengukuran tekanan darah, denyut nadi, frekuensi napas, dan suhu tubuh. Dokter juga akan memeriksa bagian tubuh yang mengalami pembengkakan.
Pemeriksaan Penunjang
Untuk mendukung diagnosis limfedema, dokter mungkin akan melakukan pemeriksaan penunjang, seperti:
- Lymphoscintiagraphy
- Metode ini merupakan pemeriksaan yang sangat efektif dalam memastikan adanya limfedema baik pada anak-anak maupun orang dewasa serta mengetahui lokasi dan tingkat kerusakan dari limfatik. Penggunaan metode ini untuk anak-anak masih belum jelas karena masih terbagi antara masih diperbolehkan dan tidak.
- Pemeriksaan genetik
- Pemeriksaan genetik berguna dalam menentukan adanya sindrom genetik terkait dengan limfedema primer pada anak-anak
- MRI (Magnetic Resonance Imaging )
- Pemeriksaan ini berguna dalam meenentukan adanya limfedema pada bayi dan anak anak muda ketika lymphoscintiagraphy tidak disarankan
- Xray, ultrasonik
- Pemeriksaan ini membantu dokter dalam mengetahui sumber pembengkakan pada anak. Pemeriksaan ultrasonik dapat membantu mengetahui pembengkakan tersebut disebabkan oleh cairan dan tipe cairan apa atau mencari gumpalan vaskular sebagai penyebab alternatif.
Tata Laksana
Tujuan dari pengobatan limfedema bergantung pada kondisi dan penyebab serta tahap limfedema. Pengobatan yang disarankan mungkin melibatkan terapi fisik atau pengobatan lain yang membantu cairan limfatik bergerak dan mengurangi pembengkakan dan nyeri.
Dokter juga akan meresepkan antibiotik untuk mengatasi infeksi atau obat nyeri untuk mengurangi rasa nyeri. Pengobatan limfedema pada anak dengan orang dewasa secara esensial sama, tetapi terdapat 3 kunci modifikasi untuk memastikan hasil pengobatan yang baik seperti keterlibatan orang tua dan dokter dalam mengawasi dan menangani gejala dai limfedema.
Orang tua dan dokter sebaiknya secara aktif mendukung anak dalam penanganan mandiri dan mendukung dalam partisipasi anak dalam aktivitas normal sehari hari serta dukungan moral dan fisik. Intervesi operasi mungkin diperlukan bila terdapat kerusakan yang disebabkan oleh pembengakan dan kondisi lainnya yang dipertimbangkan oleh dokter sebagai tahapan perlu dilakukan operasi.
Komplikasi
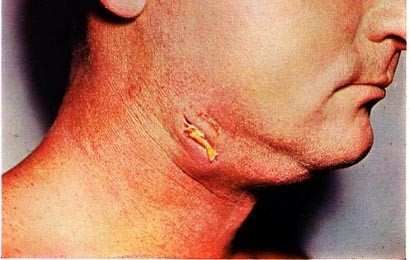
Pada beberapa kasus, komplikasi yang terjadi seperti perubahan pada kulit dan jaringan. Selain itu, adanya komplikasi infeksi seperti selulitis merupakan salah satu komplikasi yang umumnya terjadi. Kondisi tersebut dirasakan seperti terdapat area kemerahan yang lembut dan hangat dan biasanya dapat sembuh dengan bantuan antibiotik. Komplikasi lain terkait dengan psikologis, perubahan kulit, gangguan saluran air kecil.
Jika Anda ingin mengetahui selengkapnya mengenai selulitis, Anda dapat membacanya di sini: Selulitis - Definisi, Penyebab, Gejala, dan Pengobatannya
Pencegahan
Beberapa cara untuk mengurangi risiko mengalami limfedema, yaitu:
- Menggerakan kaki atau lengan secara ringan, jika anak Anda baru menjalani operasi pengangkatan kelenjar getah bening
- Menggunakan air hangat untuk membasuh atau membersihkan kulit
- Menggunakan tabir surya saat keluar rumah agar terhindar dari paparan sinar matahari yang berlebihan
- Menghindari berjalan tanpa menggunakan alas kaki
- Mengistirahatkan kaki atau lengan saat masa pemulihan, dengan menaikkan kaki atau lengan melebihi posisi jantung menggunakan alas bantal yang lembut
- Menjaga kebersihan, agar infeksi dari luar tidak memperparah bagian yang mengalami masalah
Kapan Harus ke Dokter?
Hubungi dokter bila Anda menyadari adanya tangan atau lengan dari anak Anda yang membengkak atau kemungkinan adanya infeksi.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr. Monica Salim
Lymphedema. (2022). Retrieved 27 March 2023, from https://www.childrenshospital.org/conditions/lymphedema
Pediatric Lymphedema. (2022). Retrieved 27 March 2023, from https://my.clevelandclinic.org/pediatrics/departments/lymphedema
Lymphedema Surgery & Lymphatic Reconstriction. (2022). Retrieved 27 March 2023, from https://my.clevelandclinic.org/departments/dermatology-plastic-surgery/depts/lymphedema-surgery-lymphatic-reconstruction
Lymphedema. (2022). Retrieved 27 March 2023, from https://www.ncbi.nlm.nih.gov/books/NBK537239/
Lymphedema in Children. (2021). Retrieved 27 March 2023, from https://www.ncbi.nlm.nih.gov/books/NBK537239/
Lymphedema Therapy. (2018). Retrieved 27 March 2023, from https://www.healthline.com/health/lymphedema-therapy
Lymphedema. (2022). Retrieved 27 March 2023, from https://www.cdc.gov/cancer/survivors/patients/lymphedema.htm
Lymphedema. (2023). Retrieved 27 March 2023, from https://my.clevelandclinic.org/health/diseases/8353-lymphedema