Definisi
Kelenjar getah bening adalah bagian dari sistem limfatik dengan bentuk bulat dan mengandung sel imun yang bertugas menyerang dan membunuh benda asing seperti virus dan bakteri. Kelenjar getah bening ditemukan pada berbagai bagian tubuh seperti leher, ketiak, dan selangkangan. Setiap kelenjar getah bening tersebut dihubungkan dengan jaringan limfatik yang membawa sel darah putih ke seluruh tubuh. Sel darah putih atau leukosit merupakan sel yang berguna dalam pertahanan tubuh dan merupakan sel utama dari kelenjar getah bening.
Apabila terdapat benda asing atau infeksi dalam tubuh, kelenjar getah bening akan aktif dan menimbulkan kondisi peradangan sebagai respon pertahanan tubuh. Kondisi peradangan yang timbul dapat berupa pembengkakan pada getah bening. Apabila infeksi tidak teratasi dan menyebar hingga kelenjar getah bening itu sendiri maka dapat menyebabkan kondisi yang disebut limfadenitis. Peradangan pada kelenjar getah bening biasanya ditandai dengan rasa sakit atau nyeri dan pembengkakan kelenjar. Umumnya kelenjar getah bening yang mengalami peradangan berjumlah lebih dari satu kelenjar.
Limfadenitis sendiri memiliki 2 tipe, yaitu:
- Limfadenitis lokal, merupakan tipe yang paling umum. Tipe ini melibatkan satu atau lebih kelenjar getah bening yang saling berdekatan dimana infeksi mulai terjadi. Sebagai contoh, pembesaran pada getah bening yang disebabkan oleh infeksi tonsil dapat dirasakan pada bagian area leher
- Limfadenitis umum, merupakan tipe dimana infeksi dari getah bening terjadi pada satu atau lebih kelompok kelenjar getah bening. Hal ini dapat disebabkan oleh adanya penyebaran infeksi melalui pembuluh darah atau penyakit lain yang memengaruhi seluruh tubuh.
Penyebab
Inflamasi pada kelenjar getah bening dapat terjadi karena berbagai penyebab namun terutama apabila infeksi bakteri atau virus mencapai pada kelenjar getah bening terkait dan menyebabkan infeksi. Bakteri Streptococcal dan Staphylococcal merupakan salah satu bakteri penyebab limfadenitis tersering walaupun juga dapat disebabkan oleh infeksi virus seperi HIV dan penyakit khusus seperti tuberkulosis. Kondisi sistem imun tubuh yang rendah atau imunodefisiensi juga meningkatkan risiko terjadinya limfadenitis. Selain akibat infeksi, kondisi keganasan atau kanker juga dapat menyebabkan inflamasi pada getah bening, terutama kanker darah seperti leukimia dan limfoma.
Faktor Resiko
Beberapa hal yang dapat meningkatkan risiko limfadenitis seperti:
- Usia, pada anak - anak memiliki risiko lebih tinggi mengalami limfadenitis dibandingkan orang dewasa
- Infeksi bakteri
- Anoreksia (gangguan makan)
Gejala
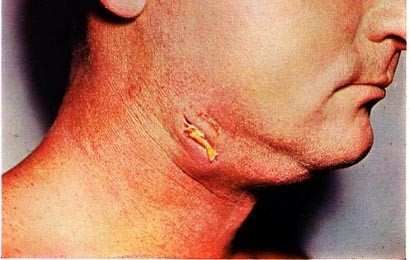
Gejala utama dari limfadenitis yaitu adanya pembengkakan dan rasa nyeri pada kelenjar getah bening yang mengalami peradangan. Getah bening dianggap membengkak atau membesar bila ukurannya bertambah sekitar 0.5 inch atau 1.27 sentimeter. Beberapa gejala lain yang mungkin dirasakan seperti demam, merasa kedinginan atau mengigil, merasa sakit jika kelenjar disentuh, kemerahan pada kulit di area kelenjar getah bening, adanya perasaan seperti mengganjal terutama bila kelenjar sudah lebih membesar atau jika terdapat abses (kumpulan nanah) yang terbentuk ketika mulai terbentuk nanah. Perlu diperhatikan bahwa terkadang gejala dari limfadenitis mirip dengan gangguan kesehatan lainnya sehingga diskusikan kembali dengan dokter Anda terkait gejala dan apa yang Anda rasakan sehingga dokter dapat melakukan diagnosa yang tepat.
Diagnosa
Dokter akan mencurigai Anda memiliki limfadentitis berdasarkan gejala dan bentuk kelenjar getah bening Anda. Pada beberapa kasus, dokter mungkin akan melakukan pemeriksaan lebih lanjut seperti ultrasonik yang merupakan metode lini pertama yang direkomendasikan. Pemeriksaan lain yang dapat dilakukan seperti:
- Pemeriksaan laboratorium: melibatkan beberapa pemeriksaan untuk mencari bakteri atau virus spesifik yang dapat limfadenitis. Pemeriksaan ini meliputi pemeriksaan darah lengkap, pemeriksaan fungsi hati dan pemeriksaan darah rutin lainnya. Pemeriksaan darah dilakukan untuk memeriksa adanya tanda dari infeksi (seperti jumlah sel darah putih) atau inflamasi (seperti ESR dan protein C reaktif). Pemeriksan kultur darah dilakukan untuk mengetahui dan mengidentifikasi bakteri spesifik penyebab dari infeksi tersebut.
- Pemeriksaan radiologi: pemeriksaan CT scan dapat menyediakan gambaran lebih detail mengenai getah bening dan struktur sekitarnya, seperti saraf atau pembuluh darah dibandingkan ultrasonik. Dokter juga mungkin dapat menemukan adanya abses apabila sudah terbentuk di kelenjar getah bening yang terinfeksi.
- Aspirasi jarum: prosedur ini melibatkan memasukkan jarum ke dalam getah bening dan mengambil sampel cairan. Hal ini berguna dalam menentukan penyebab infeksi pada kultur darah ataupun kemungkinan penyebab pembengkakan kelenjar getah bening lainnya.
Tata Laksana
Pengobatan biasanya melibatkan antibiotic dan obat sesuai gejala lainnya. Pasien juga mungkin menerima antibiotik intravena di rumah sakit apabila infeksi sudah meluas. Dokter akan meresepkan antibiotik spektrum luas sebagai lini pertama pengobatan. Antinyeri dan obat peradangan juga mungkin diresepkan untuk membantu mengurangi gejala. Pada beberapa kasus, infeksi dapat menjadi parah atau menyebabkan abses. Abses tersebut dapat menyebar, menyebabkan nyeri yang hebat hingga berisiko sepsis. Dokter mungkin memerlukan operasi untuk mengeluarkan abses. Bila limfadentitis menjadi kronis, pasien tersebut memerlukan pemeriksaan tambahan untuk mengetahui penyebab dari kondisi tersebut. Dokter mungkin akan merekomendasikan pemantauan lebih lanjut atau pemberian antibiotik lainnya.
Komplikasi
Komplikasi dapat terjadi bila limfadentis tidak diobati, adapun komplikasi yang terjadi seperti pembentukan abses (kumpulan nanah yang nyeri), selulitis (infeksi serius pada bagian dalam kulit), sepsis (infeksi yang menyebar dengan aliran darah), maupun komplikasi lain terkait dengan operasi pengeluaran abses ataupun kondisi infeksi lainnya.
Pencegahan
Salah satu pencegahan terbaik dari limfadenitis dengan menemui dokter bila Anda merasakan gejala dari infeksi apapun atau adanya pembengkakan yang diikuti rasa nyeri serta terasa seperti ada benjolan pada bagian bawah kulit anda. Pastikan anda membersihkan dan menggunakan antiseptik pada semua luka atau goresan pada kulit anda. Lakukan praktik kebersihan dan sering mencuci tangan.
Kapan Harus ke Dokter?
Hubungi dokter bila Anda membutuhkan pengobatan segera terhadap gejala dari limfadenitis atau bila gejala Anda memburuk atau memiliki gejala baru lainnya yang mengganggu kegiatan Anda sehari - hari.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr. Benita Kurniadi
URMC. (2023). Lymphadenitis. Retrieved 10 April 2023, from: https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=134&contentid=80
Myhre J. (2022) What is Lymphadenitis?. Verywell Health. Retrieved 10 April 2023, from https://www.verywellhealth.com/lymphadenitis-4780872#toc-diagnosis
Lymphadenitis : What to Know. (2022). Retrieved 10 April 2023, from https://www.medicalnewstoday.com/articles/lymphadenitis#vs-lymphadenopathy
Medical News Today. (2022). Lymphadenitis. Retrieved 10 April 2023, from: https://www.medicalnewstoday.com/articles/swollen-lymph-nodes-covid
Partridge E. (2019). Lymphadenitis. Retrieved 10 April 2023, from: https://emedicine.medscape.com/article/960858-overview
Kemenkes RI. (2022). Limfadenitis. Retrieved 10 April 2023, from: https://yankes.kemkes.go.id/view_artikel/36/limfadenitis