Definition
Lymphangitis is the inflammation or infection of lymph nodes. The lymphatic vessels, integral to the body's immune system, play a crucial role in this condition. These vessels, comprising glands and vessels, collaborate in transporting fluid from the lymph nodes to the bloodstream.
Key organs constituting the lymphatic system include:
- Tonsils, situated behind the throat.
- Spleen, located on the left side of the abdomen, functions as a filter for red blood cells.
- Thymus, a gland positioned in the chest cavity's middle, aiding in the development of white blood cells.
Lymphocytes, vital immune cells, mature in the bone marrow before migrating to lymph nodes and other lymphatic organs, where they defend against bacterial and viral infections.
Lymphatic fluid circulates throughout the body via lymphatic vessels, facilitating the elimination of fats, bacteria, and metabolic waste products. This lymph, or lymphatic fluid, filters out harmful substances for expulsion from the body. In response to the detection of harmful foreign substances, the body increases white blood cell production to combat infections.
Lymphangitis occurs when viruses or bacteria infect lymphatic vessels, typically originating from an untreated wound (an infected wound). Prompt treatment can lead to healing without complications. However, if left untreated, lymphangitis can result in various complications and other serious conditions.
Causes
Lymphangitis develops when bacteria or viruses infiltrate the lymphatic system, frequently entering through wounds or from infections elsewhere in the body.
Streptococcus bacteria are common culprits for lymphangitis infections, although Staphylococcus bacteria or a combination of both can also be responsible. These bacteria are typically associated with skin infections.
Additionally, lymphangitis may arise from parasitic or fungal infections. Fungal lymphangitis is particularly prevalent among gardeners, as the fungi causing this condition are often present in the soil.
Other contributing factors include:
- Skin infections like cellulitis
- Wounds from injections
- Insect bites or stings
- Wounds requiring stitches
Risk factor
Several factors and conditions can elevate an individual's risk of developing lymphangitis, including:
- Diabetes
- Crohn Disease
- Chickenpox
- HIV/AIDS
- Weakened immune system (immunodeficiency)
- Certain tumor types, such as breast, lung, pancreatic, prostate, and abdominal tumors
- Prolonged use of steroid medications
- Outdoor occupations like farming and gardening
Read more: Chickenpox (Varirella Zoster) - Definition, Causes, Symptoms, and Management |AI Care (ai-care.id)
Symptoms
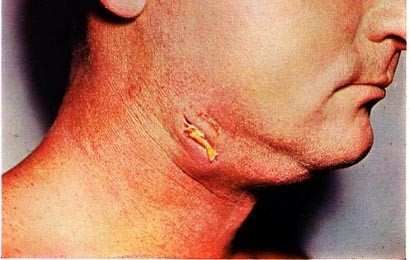
Symptoms of lymphangitis usually present as skin abnormalities, characterized by red rashes on the skin's surface, often forming lines from the infected lymphatic vessels to the nearest lymph nodes.
However, symptoms can vary from person to person. Additional manifestations may include:
- Enlargement of lymph nodes, typically in the groin area or creases of the thigh, armpits, and elbows
- Pain in the infected region
- Fatigue or malaise
- Fever
- Chills
- Headaches
- Loss of appetite
- Muscle pain
Diagnosis
Doctors diagnose lymphangitis primarily through a physical examination, assessing swelling in the lymph nodes.
In cases where the enlargement of lymph nodes persists or feels hardened upon palpation, doctors may recommend a biopsy to ascertain the underlying cause. Blood tests may also be conducted to detect any infections present in the bloodstream.
Additionally, if there are indications of joint swelling or a persistent cough, further tests such as X-rays may be warranted. In such instances, the doctor might refer you to a specialist for comprehensive evaluation and treatment.
Management
Treatment should be promptly initiated to halt the spread of infection. The doctor may prescribe various medications, including:
- Antibiotics, if bacterial infection causes lymphangitis. These antibiotics may be administered via injections or oral medications.
- Antiviral drugs, if lymphangitis stems from a viral infection.
- Antifungal medication, if fungal infection underlies lymphangitis.
- Pain relievers.
- Anti-inflammatory drugs to alleviate inflammation.
- Fever reducers.
In instances where lymphangitis leads to abscess formation, the doctor may perform a minor surgical procedure to drain the abscess fluid. Surgical intervention might also be necessary if there's a blockage in the lymphatic vessels.
At home, you can alleviate pain by applying warm compresses to the area with red rashes up to three times a day or taking warm baths. Warm compresses or baths can enhance blood circulation and expedite healing.
Read more: Abscesc - Definition, Causes, Symptoms, and Management |AI Care (ai-care.id)
Complications
Lymphangitis, if left untreated, can increase rapidly, potentially resulting in complications such as:
- Cellulitis (skin infection).
- Bacteremia (presence of bacteria in the bloodstream).
- Sepsis is a life-threatening condition marked by an exaggerated response to infection.
- Abscess formation is characterized by pus accumulation accompanied by pain, inflammation, and swelling.
Prevention
Preventing lymphangitis is challenging since it can emerge as a complication of other conditions. Nonetheless, several preventive measures can help mitigate the risk of lymphangitis. These include maintaining skin hygiene, as wounds on the skin can serve as entry points for bacteria or viruses into the lymphatic system.
To reduce the risk of developing lymphangitis, consider the following steps:
- Regularly applying lotion if you have dry skin.
- Avoiding skin injuries by wearing protective gear during sports or outdoor activities.
- Opting for long sleeves when hiking to minimize skin exposure.
- Wearing sandals at the beach to prevent skin abrasions.
- Refraining from swimming if you have open skin wounds.
- If you sustain a wound, promptly clean it, apply antibiotic ointment, cover it with a bandage, and seek medical attention if the area shows signs of redness and swelling.
When to see a doctor?
It is important to contact your doctor right away if you have symptoms of lymphangitis or if your symptoms persist despite treatment. Some symptoms require immediate attention, including:
- Severe pain.
- Spreading red rashes in the infected area.
- Fluid or pus discharge from the infected lymphatic vessels.
- High fever (above 38 degrees Celsius).
If you encounter any of these symptoms, seek medical attention without delay. Lymphangitis demands prompt and suitable treatment to avert life-threatening complications.
You can also consult regarding lymphangitis by downloading the Ai Care application on Playstore or Appstore.
Looking for more information about other diseases? Click here!
- dr. Benita Kurniadi
- dr Nadia Opmalina
Pecora F. (2021). Management of Infectious Lymphadenitis in Children. National Library of Medicine. Retrieved 27 March 2023, from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8535130/
WebMD. (2021). What is Lymphangitis. WebMD. Retrieved 27 March 2023, from: https://www.webmd.com/a-to-z-guides/what-is-lymphangitis
Kano Y. (2020). Acute Lymphangitis. Cleveland Journal Clinic of Medicine. Retrieved 27 March 2023, from https://www.ccjm.org/content/87/3/129
Natalie Philips. 2023. Lymphangitis. Available from: https://www.healthline.com/health/lymphangitis
Angelica Bottaro. 2023. Lymphangitis: Overview and More. Available from: https://www.verywellhealth.com/lymphangitis-5224749
Claveland Clinic. 2023. Lymphangitis. Available from: https://my.clevelandclinic.org/health/diseases/25234-lymphangitis