Definisi
Melasma adalah kondisi bercak-bercak gelap yang timbul pada kulit wajah sebagai efek perubahan selama kehamilan.
Tubuh akan mengalami perubahan luar biasa selama kehamilan. Perut ibu akan semakin besar dan volume darah turut meningkat seiring pertumbuhan bayi. Ibu juga dapat mengalami kram perut, mual di pagi hari, serta nyeri. Melasma adalah kelainan kulit ketika melanosit atau sel penghasil pigmen memproduksi pigmen kulit secara berlebihan. Kondisi ini tidak memengaruhi bayi atau menyebabkan komplikasi kehamilan lainnya.
Orang yang memiliki lebih banyak pigmen di kulit seperti orang Afrika, Timur Tengah, Latin atau Hispanik, Asia, India, atau keturunan Mediterania lebih mungkin mengalami melasma karena mereka memiliki produksi melanin yang lebih aktif. Secara keseluruhan, sekitar 50-70% wanita akan mengalami beberapa bentuk melasma selama kehamilan.
Penyebab
Hiperpigmentasi atau menggelapnya warna kulit selama kehamilan sangat umum terjadi. Area puting (areola), ketiak, atau alat kelamin dapat menjadi lebih gelap. Dapat juga terbentuk garis gelap di atas perut yang memanjang dari area kemaluan hingga perut bagian tengah atas (linea nigra), atau terjadi penggelapan kulit di seluruh tubuh.
Penyebab munculnya melasma pada kehamilan tidak diketahui selain adanya produksi pigmen melanin yang berlebihan. Diduga produksi pigmen berlebihan ini terjadi karena adanya perubahan hormon pada kehamilan, terutama peningkatan hormon estrogen dan progesteron.
Faktor Risiko
Chloasma dapat muncul kapan saja selama kehamilan, meskipun paling sering dimulai pada trimester kedua atau ketiga. Ada berbagai faktor yang berperan pada terbentuknya melasma selama kehamilan.
Selain itu, flek hitam di wajah dapat diperparah oleh paparan sinar matahari, penggunaan produk atau perawatan kulit tertentu, dan bahkan faktor genetik atau keturunan. Chloasma juga dapat diperburuk oleh ketidakseimbangan hormon yang mungkin terjadi karena menggunakan pil KB atau sedang menjalani terapi penggantian hormon.
Warna dan jenis kulit memengaruhi tampilan melasma, yaitu dapat membuat melasma lebih terlihat jelas atau tidak terlalu terlihat. Semakin banyak seseorang terpapar sinar matahari atau adanya faktor keturunan juga memengaruhi munculnya melasma.
Gejala
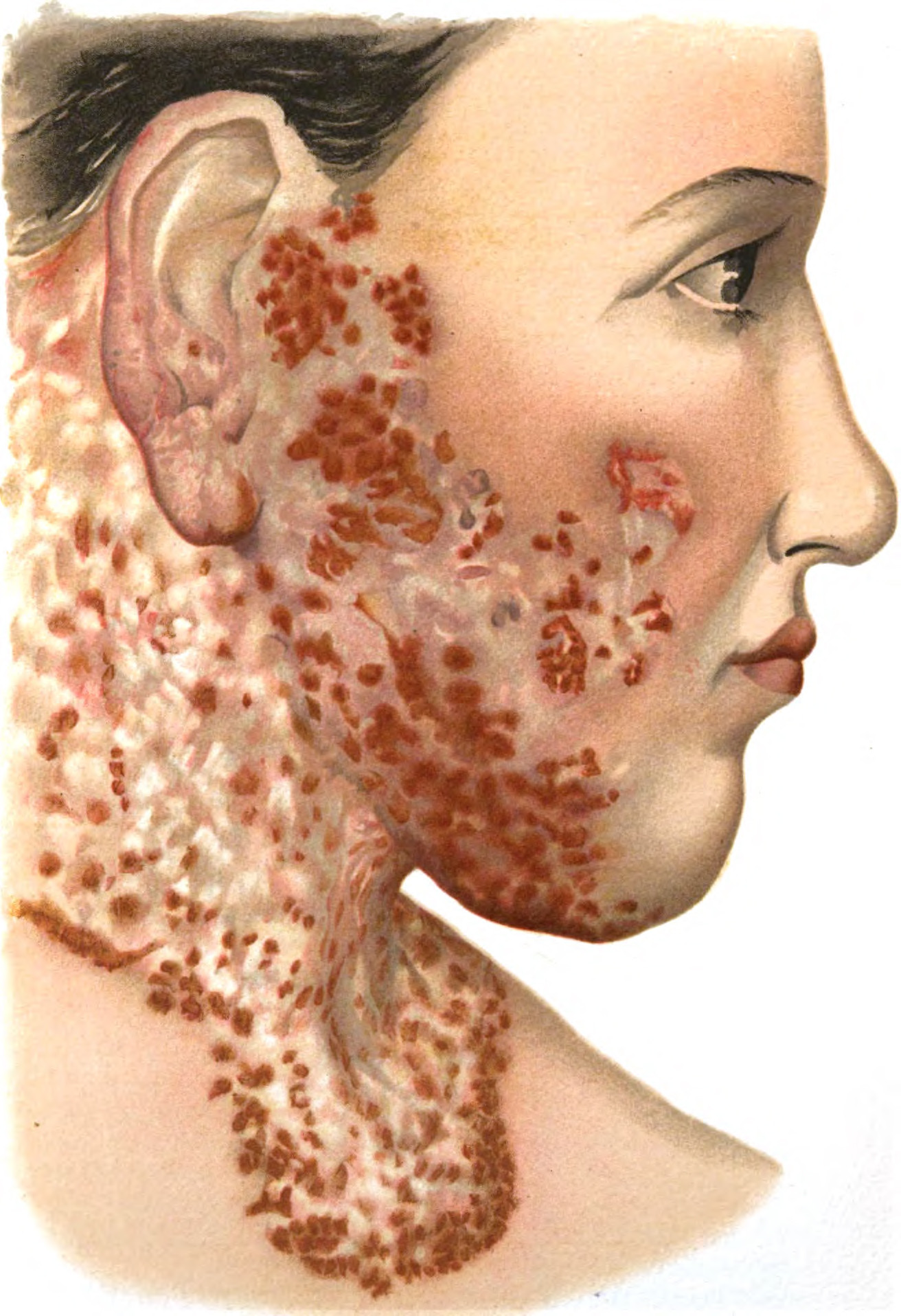
Gejala utama melasma adalah penggelapan kulit di wajah berbentuk bercak. Bercak bisa berwarna cokelat gelap sampai abu-abu pudar, dapat muncul di dahi, pipi, dagu, atau sekitar mulut. Area-area ini dapat menjadi semakin gelap jika Anda terpapar sinar matahari. Nyeri atau gatal bukanlah gejala melasma. Jika Anda mengalami tanda-tanda ini atau mengalami iritasi berat, Anda mungkin mengalami kondisi kulit lain. Konsultasikan semua gejala tambahan yang Anda rasanya pada dokter.
Diagnosis
Hal yang terpenting adalah jangan mencoba mendiagnosis kondisi Anda sendiri. Hanya dokter kulit yang dapat memastikan apakah Anda menderita melasma pada kehamilan. Diagnosa melasma tergantung pada waktu munculnya gejala serta lokasi bercaknya. Biasanya munculnya bercak gelap di kulit dimulai pada kehamilan, setelah penggunaan pil KB, atau memburuk saat musim panas. Chloasma jarang terjadi hanya di salah satu sisi wajah.
Dokter kulit juga dapat mendiagnosis melasma dengan menggunakan lampu khusus yang disebut lampu Wood, yang membantu menunjukkan apakah suatu kondisi kulit disebabkan oleh bakteri, jamur, atau lainnya. Pada kondisi yang jarang terjadi, ketika diagnosis pasti belum bisa ditegakkan, dokter dapat melakukan biopsi dengan mengambil sampel jaringan kulit untuk memastikan perubahan warna bukan menunjukkan kondisi kulit lain, seperti melanoma atau kanker kulit.
Tata Laksana
Kabar baiknya adalah hiperpigmentasi ini kemungkinan tidak akan bertambah buruk setelah Anda melahirkan. Mungkin perlu waktu berbulan-bulan agar bercak tersebut benar-benar memudar jika tanpa perawatan khusus.
Perawatan yang Aman pada Kehamilan
Konsultasi dengan dokter tentang cara mengobati melasma selama hamil. Dokter dapat merujuk Anda ke dokter kulit untuk penanganan lebih lanjut bila diperlukan.
Beberapa ahli tidak merekomendasikan pengobatan melasma selama kehamilan. Salah satu alasannya adalah bahwa kondisi tersebut dapat hilang dengan sendirinya setelah melahirkan. Dan beberapa metode pengobatan mungkin tidak aman atau tidak efektif untuk digunakan saat hamil. Perawatan terbaik sebenarnya adalah pencegahan dengan bantuan beberapa perubahan gaya hidup.
Cari Tempat Teduh
Bila berada di luar ruangan, cari tempat yang teduh karena matahari dapat memicu lebih banyak produksi pigmen melanin. Sebaiknya hindari paparan sinar matahari secara langsung, terutama untuk jangka waktu yang lama. Batasi waktu berjemur dan cobalah bersantai di bawah pohon atau payung. Jika Anda ingin berolahraga, cobalah menghindari jam-jam saat matahari sangat terik seperti pada tengah hari. Berolahraga lah pada pagi atau sore hari saat matahari tidak terik.
Gunakan Tabir Surya
Dengan adanya melasma, bukan berarti Anda harus tinggal di dalam rumah terus saat matahari terbit. Gunakan tabir surya yang aman untuk kehamilan dengan SPF 30+ jika harus beraktivitas di luar ruangan.
Carilah produk yang mengandung seng oksida, titanium dioksida, atau pelindung fisik lainnya (tabir surya mineral) dibandingkan dengan produk yang mengandalkan pelindung kimia. Tabir surya dengan pelindung fisik cenderung menawarkan perlindungan yang lebih luas dan tidak terlalu mengiritasi kulit.
Gunakan Produk Perawatan Kulit yang Lembut
Pembersih wajah, losion, dan serum yang mengiritasi kulit Anda dapat memperburuk melasma. Pilih produk yang memiliki label "non komedogenik," "sensitif," "bebas pewangi," atau "disetujui dokter kulit" saat membeli produk kecantikan.
Hal yang sama berlaku juga untuk riasan yang mungkin Anda gunakan untuk menyembunyikan bercak gelap. Cari alas bedak, concealer, bedak, atau produk lainnya yang bersifat non komedogenik dan hipoalergenik. Gunakan riasan dengan warna kuning atau putih untuk menutupi bercak hitam jika mengganggu penampilan Anda.
Makan dan Istirahat Teratur
Karena melasma juga dapat disebabkan oleh ketidakseimbangan hormon, Anda dapat memperbaiki keadaan tersebut dengan melakukan pola hidup sehat secara teratur. Pastikan kebutuhan cairan Anda cukup, makan makanan kaya buah dan sayuran segar, serta tidur dengan cukup.
Pastikan Anda melengkapi diet dengan suplemen asam lemak omega-3. Serta konsultasi pada dokter mengenai potensi kekurangan vitamin. Beberapa penelitian menunjukan ada hubungan antara melasma dengan kekurangan zat besi dan vitamin B12.
Setelah melahirkan, Anda mungkin akan konsultasi ke dokter kulit mengenai perawatan lain jika melasma tidak kunjung memudar dengan sendirinya. Perawatan dengan obat topikal dapat meliputi penggunaan hidrokuinon, tretinoin, atau kortikosteroid sesuai dengan aturan dokter. Dokter mungkin juga merekomendasikan zat asam tertentu yang dapat mencerahkan kulit. Ada juga beberapa prosedur seperti chemical peeling, mikrodermabrasi, perawatan laser, dan terapi cahaya khusus yang dapat dilakukan sesuai dengan anjuran dokter.
Komplikasi
Belum ada komplikasi medis yang diketahui terkait melasma. Melasma juga tidak meningkatkan risiko kanker kulit. Yang mungkin terjadi adalah komplikasi psikososial akibat warna kulit yang berubah dan tidak merata.
Pasien dapat merasa malu hingga stres akibat perubahan warna kulit ataupun karena proses pengobatan yang tidak sebentar. Selain itu, adanya kecenderungan melasma untuk kambuh jika tidak dilakukan tindakan pencegahan yang tepat. Untungnya, melasma umumnya memudar dalam beberapa bulan setelah melahirkan.
Selalu konsultasikan dengan dokter mengenai manfaat dan risiko masing-masing pilihan pengobatan yang aman untuk kehamilan Anda.
Pencegahan
Beberapa cara mencegah melasma adalah:
- Membatasi paparan sinar matahari
- Gunakan tabir surya dengan perlindungan UVA dan UVB serta minimal SPF 30 atau lebih. Tabir surya yang mengandung seng atau titanium oksida adalah pilihan yang baik. Oleskan tabir surya 20 menit sebelum berada di bawah sinar matahari dan oleskan ulang setiap 2 jam. Gunakan lebih banyak tabir surya jika akan berenang
- Kenakan topi yang lebar dan kacamata hitam untuk melindungi dari terik matahari
- Batasi waktu berjemur sekitar pukul 10 pagi
- Gunakan pembersih wajah dan krim yang lembut untuk menghindari iritasi pada kulit yang dapat memperburuk melasma
Kapan Harus ke Dokter?
Konsultasi ke dokter jika:
- Tampak bintik hitam atau tahi lalat baru, terutama yang berubah dengan cepat
- Terasa nyeri, nyeri tekan, kemerahan, atau pendarahan dengan perubahan warna kulit pada bercak atau area sekitarnya
Mau tahu informasi seputar penyakit kulit dan rambut lainnya? Yuk, baca lebih banyak artikelnya di sini!
- dr Hanifa Rahma
Marcin, A. (2021). How is melasma treated during pregnancy?. Retrieved 14 March 2022, from https://www.healthline.com/health/pregnancy/melasma-pregnancy
Melasma ("Pregnancy mask') on cheek. (2021). Retrieved 14 March 2022, from https://www.webmd.com/skin-problems-and-treatments/picture-of-melasma-pregnancy-mask-on-cheek
Matta, C. (2021). What is pregnancy melasma? exactly how to treat the skin discoloration. Retrieved 14 March 2021, from https://www.verywellfamily.com/what-is-pregnancy-melasma-pregnancy-mask-definition-symptoms-traits-causes-treatment-5206946#toc-how-is-pregnancy-melasma-diagnosed
Peri, C. (2021). Pregnancy mask. Retrieved 14 March 2022, from https://www.webmd.com/baby/pregnancy-mask