Definisi
Moluskum kontagiosum (molluscum contagiosum) adalah infeksi kulit yang disebabkan oleh poxvirus. Infeksi ini menyebabkan terbentuknya bintil kecil yang bulat seperti kubah dengan lekukan di bagian tengahnya (delle), padat, dan tidak nyeri. Bintil ini memiliki ukuran yang bervariasi, mulai dari sebesar jarum pentul hingga sebesar biji jagung. Jika bintil ditekan, benda putih akan keluar dari dalam bintil. Benda putih ini disebut badan moluskum.
Moluskum kontagiosum dapat menular dari kontak langsung dengan kulit seseorang yang mengalami infeksi atau secara tidak langsung melalui benda-benda yang terkontaminasi virus.
Moluskum kontagiosum lebih sering terjadi pada anak-anak. Pada dewasa, moluskum kontagiosum sering dialami oleh orang-orang yang memiliki gangguan imunitas, seperti HIV/AIDS atau diabetes. Orang dewasa dengan sistem imun yang sehat dapat mengalami moluskum kontagiosum setelah berhubungan seksual dengan orang yang terinfeksi.
Jika tidak diobati, bintil tersebut akan hilang dalam kurun waktu 6 bulan hingga 2 tahun.
Penyebab
Poxvirus adalah virus DNA yang dapat menyebar melalui kontak langsung. Virus ini menginfeksi jaringan terluar kulit (epidermis) dan akan membelah diri di dalam sel-sel tersebut. Jarak antara paparan virus pertama dan munculnya gejala (masa inkubasi) adalah sekitar 2-8 minggu.
Virus ini paling sering menyebar melalui cara berikut:
- Kontak langsung dengan kulit penderita moluskum kontagiosum
- Kontak dengan barang-barang yang digunakan penderita moluskum kontagiosum, seperti handuk, sprei, atau pakaian
- Berenang di kolam atau pemandian air hangat yang terkontaminasi virus
- Berhubungan seksual dengan penderita moluskum kontagiosum
- Menggaruk atau memecahkan bintil yang dapat menyebar ke kulit sekitarnya
Faktor Risiko
Moluskum kontagiosum cukup sering terjadi, terutama pada anak-anak berusia 1-10 tahun.
Kelompok lain yang memiliki risiko tinggi mengalami moluskum kontagiosum adalah:
- Kelompok dengan masalah imunitas, seperti mengalami HIV/AIDS atau menjalani kemoterapi. Tampilan moluskum kontagiosum pada populasi ini dapat berbeda dibandingkan populasi sehat–lebih berat dan lebih sulit ditangani
- Mengalami dermatitis atopik. Dermatitis atopik menyebabkan pertahanan kulit lebih lemah dan lebih mudah terinfeksi virus
- Tinggal di lingkungan yang hangat, lembab, dan padat penduduk
Gejala
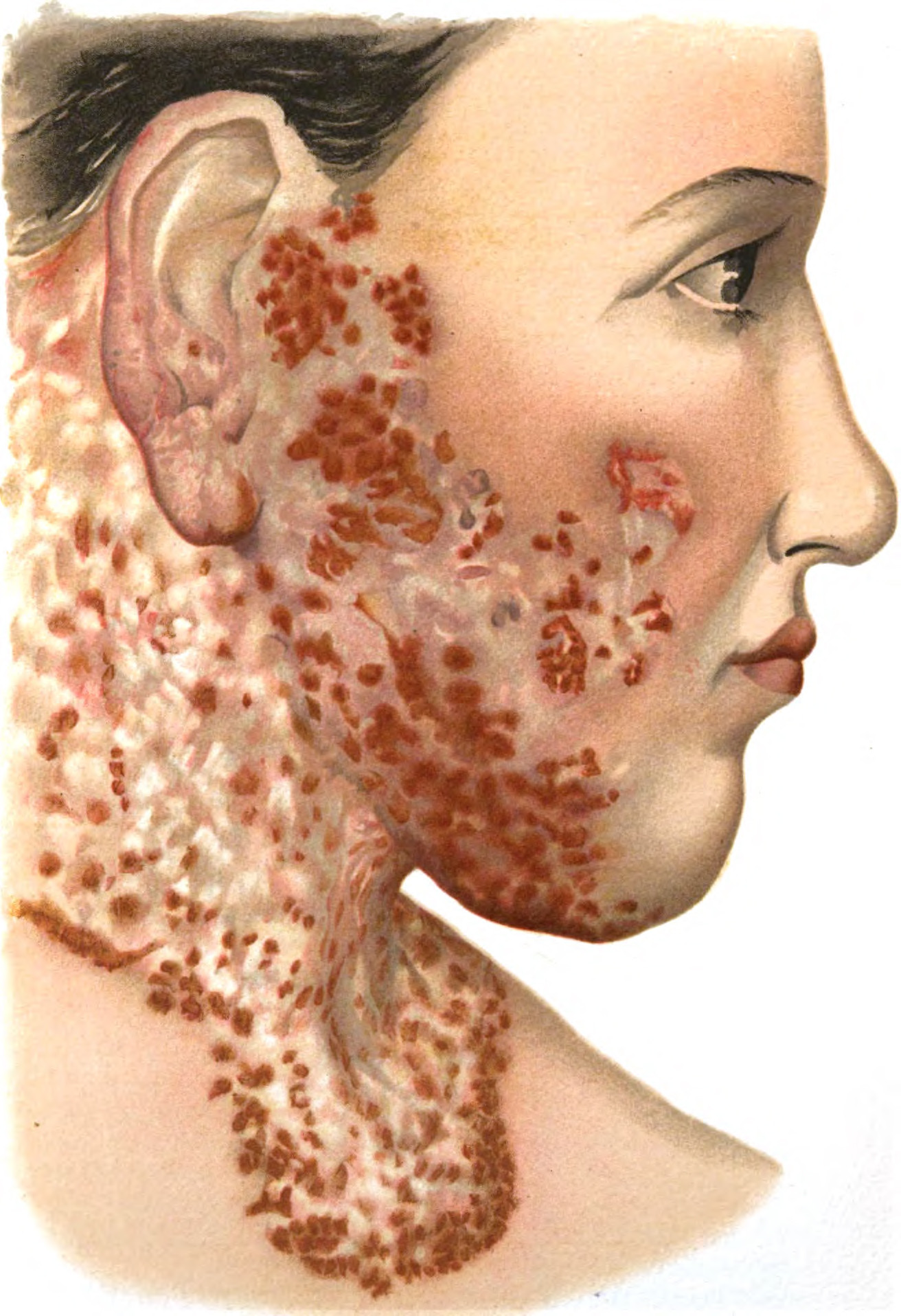
Gejala yang muncul jika mengalami moluskum kontagiosum adalah:
- Munculnya bintil bulat berbentuk kubah dengan lekukan di tengahnya
- Bintil sewarna kulit dan menimbul
- Bagian tubuh tempat bintil sering muncul adalah wajah, batang tubuh atau badan, dan tangan serta kaki
- Ukuran bintil sekitar 1-5 mm serta bertangkai. Beberapa bintil dapat berukuran lebih besar (sekitar 10-15 mm)
- Gatal pada bagian yang berbintil
- Bintil dapat timbul pada alat kelamin, bagian bawah perut, dan paha dalam pada infeksi menular seksual (IMS)
Diagnosis
Dokter mendiagnosis moluskum kontagiosum berdasarkan tampilan kulit. Tampilan moluskum kontagiosum cukup khas, yaitu bintil sewarna kulit dengan lekukan pada bagian atasnya.
Jika diperlukan pemeriksaan lebih lanjut, dokter dapat melakukan:
- Pemeriksaan giemsa. Pemeriksaan ini menggunakan badan moluskum (massa putih di dalam bintil). Dokter akan mencari badan inklusi, yaitu virus yang bersembunyi di dalam sel
- Pemeriksaan histopatologis. Pemeriksaan ini menggunakan sampel kulit yang diambil dari kerokan atau biopsi di daerah yang terinfeksi. Dokter akan mencari virus pox pada jaringan epidermis
- Pemeriksaan PCR untuk mencari partikel virus
Tata laksana
Moluskum kontagiosum dapat sembuh tanpa pengobatan dalam waktu 6 bulan hingga 2 tahun. Setelah bintil hilang, Anda tidak lagi dapat menularkan virus ke orang lain. Jika Anda pernah mengalami moluskum kontagiosum, Anda dapat terinfeksi kembali (reinfeksi). Tindakan lebih lanjut untuk mengobati moluskum kontagiosum secara umum tidak direkomendasikan, karena:
- Infeksi dapat sembuh dengan sendirinya
- Infeksi tidak menyebabkan gejala lain selain bintil
- Infeksi tidak mengganggu aktivitas sehari-hari, seperti bekerja, berenang, dan berolahraga
- Pengobatan umumnya dapat menimbulkan rasa nyeri dan bekas luka
Pengobatan umumnya direkomendasikan untuk anak yang lebih besar atau orang dewasa dengan gejala berat, memiliki gangguan sistem imun, dan mengganggu aktivitas sehari-hari.
Jika dokter Anda menyarankan untuk melakukan pengobatan lebih lanjut, pengobatan yang dilakukan berupa tindakan dan obat-obatan luar. Tindakan yang dilakukan bertujuan untuk mengeluarkan badan moluskum. Hal ini dilakukan dengan menggunakan ekstraktor komedo, jarum suntik, atau bedah beku. Setelah tindakan, dokter Anda akan meresepkan antibiotik topikal (oles). Prosedur ini dapat menimbulkan nyeri sehingga dokter Anda akan melakukan pembiusan lokal terlebih dahulu.
Selain tindakan, obat-obatan yang membantu penyembuhan, antara lain:
- Obat yang dapat menyebabkan iritasi lokal pada bintil, seperti benzoil peroksida
- Obat yang menyebabkan kulit melepuh sehingga bintil dapat terangkat dan diambil dengan lebih mudah, seperti kantaridin
Pengobatan yang disarankan juga dapat berupa kombinasi dari tindakan dan obat-obatan luar.
Dokter akan merujuk ke spesialis jika Anda memiliki:
- Bintil pada daerah mata disertai dengan mata yang merah atau nyeri
- Penyakit komorbid lainnya, seperti HIV, dengan gejala berat
- Memiliki gangguan sistem imun akibat hal lain, seperti dalam kemoterapi
Komplikasi
Moluskum kontagiosum jarang menyebabkan komplikasi lanjutan, namun pada beberapa kasus dapat menyebabkan hal-hal di bawah ini:
- Bintil terinfeksi oleh bakteri sehingga membutuhkan antibiotik
- Iritasi kulit dan peradangan dalam jangka waktu lama sehingga meninggalkan bekas. Setelah bintil hilang, bintil akan meninggalkan bagian kecil yang lebih pucat dibandingkan kulit lainnya. Hal ini sering terjadi terutama setelah pengobatan
- Masalah penglihatan. Infeksi pada mata dapat terjadi terutama jika bintil berada di sekitar kelopak mata. Infeksi ini dapat berupa konjungtivitis dan keratitis. Gejala yang ditimbulkan antara lain adalah mata berair, merah, dan sensitif terhadap cahaya
- Selulitis adalah komplikasi yang sering terjadi pada orang yang memiliki gangguan imunitas, seperti HIV/AIDS. Infeksi sekunder oleh bakteri dapat menyebabkan abses
Pencegahan
Untuk mencegah penyebaran virus, Anda dapat melakukan hal-hal di bawah ini:
- Cuci tangan. Jaga kebersihan tangan Anda dengan mencuci tangan menggunakan sabun
- Jangan menyentuh bintil. Menyentuh dan menggaruk bintil dapat menyebarkan virus ke bagian kulit yang sehat atau ke benda yang Anda sentuh
- Hindari menggunakan barang personal secara bergantian dengan orang lain. Barang personal tersebut termasuk pakaian, handuk, sisir, dan lain-lain
- Hindari kontak seksual. Jika Anda memiliki bintil moluskum kontagiosum di sekitar perut bawah atau di daerah kemaluan, hindari berhubungan seksual hingga Anda sembuh
- Tutupi bintil ketika keluar rumah. Tutupi bintil dan area kulit yang sakit ketika Anda berada di sekitar orang lain untuk menghindari kontak langsung. Jika Anda sedang tidak bertemu dengan orang lain, Anda dapat membuka bagian kulit tersebut untuk mempercepat penyembuhan.
- Menggunakan kondom ketika berhubungan seksual
Kapan Harus ke Dokter?
Jika Anda menduga Anda atau anak Anda mengalami moluskum kontagiosum, segera periksakan diri ke fasilitas kesehatan terdekat. Hindari menggaruk, memencet, dan berkontak dengan bintil secara langsung. Jika Anda mengalami gejala komplikasi dari moluskum kontagiosum seperti mata merah, berair, infeksi di sekitar bintil, segera periksakan diri ke dokter untuk mendapatkan pemeriksaan dan pengobatan lebih lanjut.
- dr Nadia Opmalina
Badri T, Gandhi GR. Molluscum Contagiosum. [Updated 2022 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441898/
Biggers A. (2022). Everything you need to know about molluscum contagiosum. Healthline. Available from: https://www.healthline.com/health/molluscum-contagiosum
Bhatla AC. (2020). What are the complications of molluscum contagiosum. Medscape. Available from: https://www.medscape.com/answers/910570-30353/what-are-the-complications-of-molluscum-contagiosum
Mayo Clinic. (2022). Molluscum contagiosum. Available from: https://www.mayoclinic.org/diseases-conditions/molluscum-contagiosum/diagnosis-treatment/drc-20375230
National Health Service. (2020). Molluscum contagiosum. Available from: https://www.nhs.uk/conditions/molluscum-contagiosum/
Oakley A. (2021). Molluscum contagiosum. DermNet NZ. Available from: https://dermnetnz.org/topics/molluscum-contagiosum