Definisi
Nekrolisis epidermal toksik (TEN) adalah reaksi hipersensitivitas kulit yang umumnya dipicu oleh obat. Reaksi hipersensitivitas adalah respon berlebihan dari sistem kekebalan tubuh terhadap jaringan yang sehat atau zat yang tidak berbahaya. Sistem kekebalan tubuh malah menyerang jaringan yang sehat sehingga menimbulkan kerusakan pada jaringan tubuh kita. TEN termasuk kondisi yang langka dan jarang terjadi, namun bisa mengancam jiwa. TEN ditandai dengan kulit yang melepuh dan mengelupas, dan menyerupai luka bakar.
TEN merupakan kondisi yang lebih berat dari penyakit serupa lainnya, yaitu sindrom Stevens-Johnson (SJS), merupakan reaksi hipersensitivitas pada kulit berupa luka lepuh. Kondisi pengelupasan kulit dianggap sebagai TEN bila reaksi hipersensitivitas kulit terjadi pada lebih dari 30% permukaan tubuh dan selaput lendir mengalami kerusakan yang luas. Sementara pada SJS, luas luka tidak lebih dari 10 persen permukaan tubuh. TEN dapat terjadi pada semua golongan usia.
Karena kulit merupakan pelindung pertama tubuh dari bakteri dan mikroba, TEN dapat menimbulkan komplikasi yang serius akibat kerusakan kulit yang terjadi, seperti infeksi berat pada paru ataupun yang menyebar melalui aliran darah. Oleh karena itu, TEN harus segera ditangani. Pasien umumnya dirawat di rumah sakit karena memerlukan perawatan suportif untuk mengendalikan rasa sakit, merawat luka, dan memastikan pasien mendapatkan cairan yang cukup. Pemulihan bisa memakan waktu berminggu-minggu hingga berbulan-bulan.
Penyebab
Reaksi hipersensitivitas yang terjadi pada TEN biasanya disebabkan oleh obat dan infeksi, walaupun banyak juga kasus yang penyebabnya tidak diketahui. Meski termasuk jarang, imunisasi serta transplantasi organ juga dapat menjadi pemicu TEN. Pada TEN yang disebabkan oleh obat, umumnya gejala mulai muncul sekitar 1 - 4 minggu setelah konsumsi obat baru. Obat-obatan yang dapat memicu reaksi SJS/TEN antara lain:
- Antibiotik golongan sulfonamid, seperti kotrimoksazol
- Antibiotik beta laktam, seperti sefalosporin
- Obat anti kejang, seperti karbamazepin, fenobarbital, fenitoin
- Parasetamol
- Allopurinol yang biasa digunakan dalam terapi asam urat berlebih
- Nevirapine yang digunakan dalam pengobatan HIV
- Obat anti inflamasi nonsteroid (OAINS), seperti meloksicam atau piroxicam
Penyebab lain yang berpotensi menimbulkan reaksi hipersensitivitas pada TEN adalah infeksi atau keganasan, seperti:
- Infeksi virus:
- Cytomegalovirus
- Herpes simplex
- Hepatitis A
- Covid-19
- Infeksi bakteri Mycoplasma pneumoniae
- Kanker paru
- Kanker hati
Faktor Risiko
TEN dapat dialami oleh siapa saja. Namun, risiko lebih besar terjadi pada kelompok orang berikut, yaitu:
- Sistem kekebalan tubuh yang lemah
- Pasien transplantasi organ
- HIV/AIDS
- Penyakit autoimun
- Sedang menjalani terapi yang menurunkan sistem kekebalan tubuh
- Kanker
- Riwayat SJS/TEN sebelumnya
- Riwayat keluarga
- Faktor genetik
Gejala
Gejala dari TEN biasanya diawali dengan gejala mirip infeksi saluran pernapasan atas. Gejala ini bisa bertahan selama 1 hari hingga 3 minggu. Beberapa gejala tersebut yaitu:
- Demam dengan suhu >38 oC
- Kelelahan
- Sakit tenggorokan
- Batuk dan pilek
- Nyeri otot dan sendi
- Mata merah dan perih
- Nafsu makan menurun
- Mual dan muntah
Selanjutnya, akan terjadi reaksi pada selaput lendir seperti rasa nyeri dan panas. Bisa juga muncul gejala tambahan tergantung lokasi selaput lendir yang terkena, seperti:
- Mata, berupa mata merah atau sensitif terhadap cahaya
- Mulut atau bibir, berupa bibir kemerahan, kering dan mengelupas, atau sariawan
- Tenggorokan dan kerongkongan, berupa sulit menelan
- Saluran kencing dan kelamin, berupa luka pada kelamin dan sulit buang air kecil
- Saluran pernapasan, berupa batuk dan sesak napas
- Saluran pencernaan, berupa diare
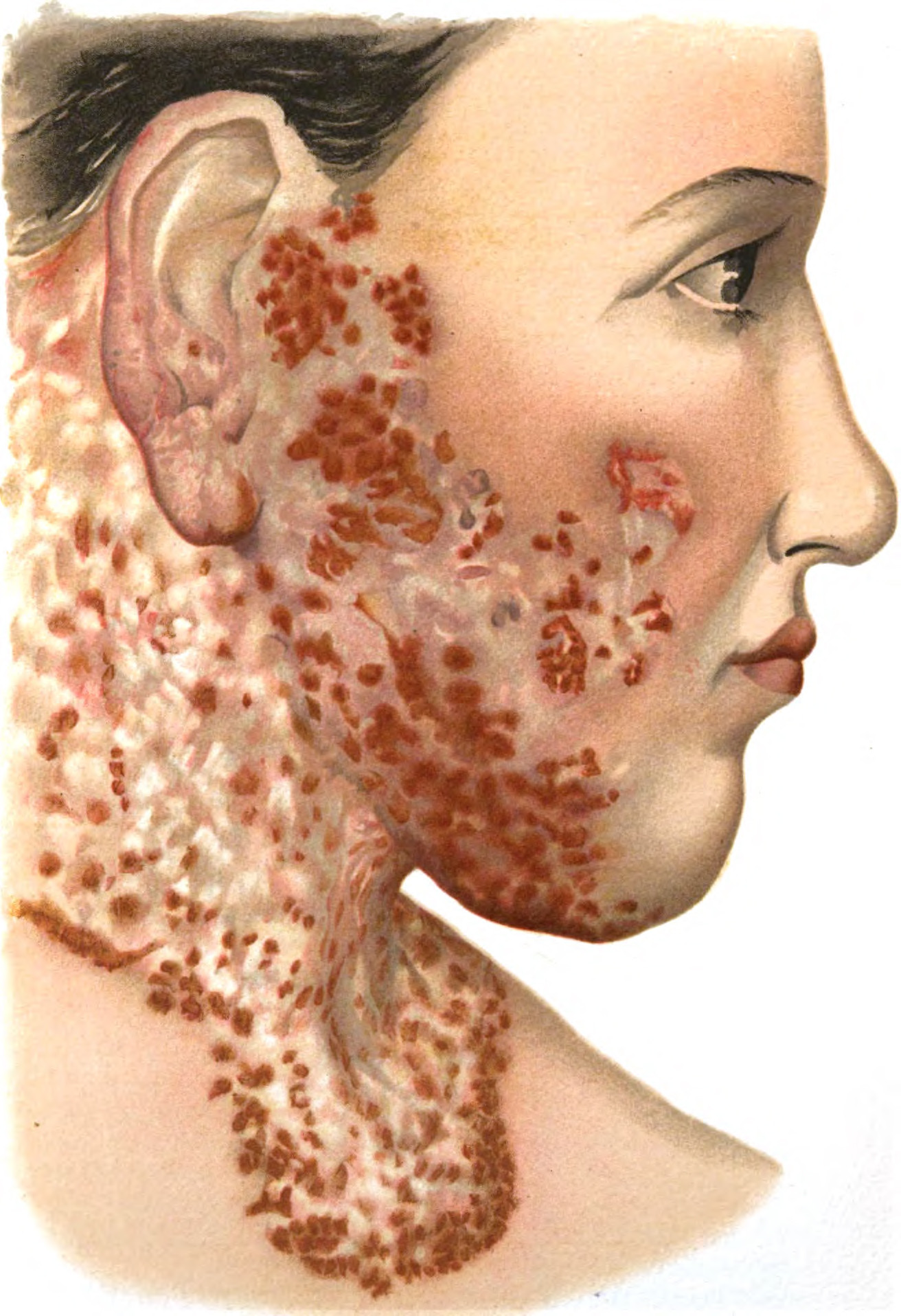
Umumnya, gejala pada kulit akan muncul pada 1–3 hari setelah gejala selaput lendir. Ruam kulit bisa muncul dengan tiba-tiba pada bagian dada, perut, atau punggung, kemudian menyebar dengan cepat ke wajah, lengan, dan kaki. Ruam dapat menyebar ke seluruh tubuh dalam waktu sekitar 4 hari. Ruam dapat berupa kulit memerah, bentol-bentol merah, bercak-bercak merah berbentuk lingkaran, lepuhan berisi air yang mudah pecah, atau kombinasi semua bentuk yang ada. Semua jenis ruam ini terasa nyeri.
Gejala kulit yang khas pada TEN adalah lepuhan kulit yang dapat membesar dan menyatu. Hal ini menyebabkan lapisan kulit terluar bisa terkelupas, sehingga lapisan tengah kulit yang merah dan basah akan terpapar ke udara luar. Dapat juga timbul luka, pembengkakan dan pengerasan kulit pada selaput lendir, termasuk mulut, mata dan vagina.
TEN menimbulkan gejala yang berat. Pasien dapat mengalami nyeri hebat hingga menimbulkan rasa gelisah. Selain itu, organ lain seperti hati, ginjal, paru-paru, sumsum tulang, dan sendi juga dapat mengalami gangguan.
Diagnosis
TEN didiagnosis ketika reaksi SJS mengenai lebih dari 30% permukaan tubuh. Pada awalnya, dokter akan menanyakan gejala, riwayat kesehatan pasien serta keluarganya, dan obat-obatan yang sedang dikonsumsi. Setelah itu, dokter akan melakukan pemeriksaan fisik, melihat bagaimana tingkat keparahan penyakit dan luas luka pada pasien.
Umumnya, TEN sudah dapat didiagnosis hanya melalui wawancara gejala serta pemeriksaan fisik. Namun, dokter juga dapat melakukan beberapa pemeriksaan penunjang berikut untuk mendukung diagnosis, yaitu:
- Biopsi kulit, untuk memastikan diagnosis dengan mengambil sampel kulit dan diperiksa di bawah mikroskop
- Pemeriksaan darah dan urine, dilakukan untuk mendeteksi komplikasi seperti adanya kekurangan nutrisi, serta untuk memperkirakan kesembuhan pasien
Tata Laksana
Jika dokter mencurigai penyebab TEN adalah obat, pasien harus menghentikan konsumsi obat tersebut secara permanen. Pasien biasanya akan dirawat di rumah sakit, tepatnya di ruang rawat intensif. Pemulihan total penyakit bisa memakan waktu beberapa bulan.
Perawatan suportif
Perawatan suportif pada pasien TEN selama di rumah sakit antara lain:
1. Terapi Cairan dan Nutrisi
Rusaknya lapisan kulit dapat menyebabkan hilangnya cairan dari tubuh, sehingga terapi cairan dan ion tubuh sangat penting untuk diberikan. Pasien mendapatkan cairan dan nutrisi melalui selang makanan yang dimasukkan ke perut melalui hidung (tabung nasogastrik). Cairan dan nutrisi juga bisa diberikan melalui pembuluh darah (infus).
2. Perawatan Luka
Tenaga kesehatan akan membersihkan luka dan kulit yang terkelupas, lalu menutup luka dengan pembalut khusus yang mengandung petroleum jelly atau obat-obatan. Pasien juga akan mendapatkan terapi antibiotik jika terdapat infeksi pada luka.
3. Bantuan Pernapasan
Pasien mungkin memerlukan pemeriksaan dan prosedur tertentu untuk mengevaluasi jalan napas dan menjaga agar jalan napas tetap bersih. Pada kondisi yang lebih berat, mungkin diperlukan tindakan intubasi atau pemberian bantuan napas melalui selang yang dimasukkan ke tenggorokan melalui mulut.
4. Mengontrol Rasa Sakit
Pasien akan diberikan obat anti nyeri untuk mengurangi rasa tidak nyaman. Untuk rasa sakit di mulut, pasien akan diberikan obat kumur yang mengandung obat mati rasa.
5. Perawatan Mata
Untuk gejala mata ringan, pasien akan diberikan tetes air mata buatan sekitar 4 kali sehari. Tetes mata dengan kortikosteroid dapat digunakan untuk mengontrol peradangan mata.
Prosedur Operasi
Jika obat belum bisa menyembuhkan pasien, dokter dapat melakukan beberapa tindakan operasi seperti debridement dan pencangkokan kulit. Debridement adalah operasi kecil untuk membersihkan jaringan mati pada luka. Sementara itu, pencangkokan kulit merupakan prosedur penempelan kulit sehat ke area tubuh yang mengalami kerusakan kulit berat. Kulit yang sehat diambil dari bagian tubuh lain atau dari donor.
Perawatan Mandiri
Setelah diperbolehkan pulang, pasien perlu melakukan perawatan mandiri di rumah, meliputi:
- Merawat luka sesuai anjuran dokter untuk mempercepat penyembuhan dan mencegah infeksi
- Menjaga kesehatan mulut, seperti rutin menyikat gigi dengan sikat yang lembut atau menggunakan obat kumur
- Minum air putih yang cukup untuk mencegah kekurangan cairan tubuh
- Melakukan terapi fisik untuk meningkatkan fungsi dan kekuatan otot serta meredakan nyeri
Umumnya, proses penyembuhan membutuhkan waktu 3–6 minggu.
Komplikasi
Pasien yang paling berisiko mengalami komplikasi adalah orang-orang yang berusia di atas 70 tahun, penderita sirosis hati (terdapatnya jaringan parut pada hati), atau menderita kanker stadium akhir yang sudah menyebar ke organ-organ lain di tubuh.
Komplikasi TEN meliputi:
- Infeksi yang meluas melalui darah (sepsis) dan berpotensi menyebabkan kegagalan organ
- Gangguan paru-paru berupa batuk, kesulitan bernapas, hingga gagal nafas
- Gangguan penglihatan seperti mata kering, bulu mata tumbuh ke dalam, terbentuk jaringan parut pada kornea, hingga kebutaan
- Kerusakan kulit permanen dan masalah kulit yang berkepanjangan
- Luka pada vagina
- Penderitaan emosional yang berdampak pada kondisi psikologis pasien dalam jangka panjang
- Gangguan indera pengecap
- Malnutrisi
- Tukak lambung atau saluran pencernaan lain
- Koagulopati atau gangguan pembekuan darah
Pencegahan
Untuk mencegah kekambuhan TEN, ketahui apakah kondisi tersebut disebabkan oleh obat. Jika telah diketahui obat adalah pemicunya, ganti dan hindari konsumsi obat tersebut. Kekambuhan dapat lebih buruk dan mengancam jiwa. Selain itu, beri tahu petugas kesehatan tentang riwayat reaksi obat atau alergi Anda terhadap obat tertentu setiap kali harus mendapatkan pertolongan medis.
TEN belum dapat sepenuhnya dicegah. Namun, risikonya dapat diminimalisir dengan berhati-hati dan selalu berkonsultasi dengan dokter mengenai obat yang akan dikonsumsi, terutama jika Anda memiliki risiko TEN.
Kapan Harus ke Dokter?
Penanganan sedini mungkin adalah kunci pengobatan TEN. Reaksi kulit yang terjadi pada TEN sangatlah jelas, sehingga bila Anda memiliki gejala TEN seperti yang sudah disebutkan di atas, segera cari pertolongan medis ke instalasi gawat darurat terdekat.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Hanifa Rahma
TEN. (2020). Retrieved 27 April 2022, from https://www.mayoclinic.org/diseases-conditions/toxic-epidermal-necrolysis/symptoms-causes/syc-20491903
Cohen SPJ. (2021). Toxic epidermal necrolysis (TEN). Retrieved 27 April 2022, from https://emedicine.medscape.com/article/229698-overview
Toxic epidermal necrolysis: causes, symptoms, and treatments. (2021). Retrieved 27 April 2022, from https://www.webmd.com/skin-problems-and-treatments/what-is-toxic-epidermal-necrolysis#
Nunez K. (2019). What is toxic epidermal necrolysis (TEN)?. Retrieved 27 April 2022, from https://www.healthline.com/health/toxic-epidermal-necrolysis#
Labib A, Milroy C. (2021). Toxic epidermal necrolysis. Retrieved 27 April 2022, from https://www.ncbi.nlm.nih.gov/books/NBK574530/
Toxic epidermal necrolysis (TEN). Retrieved 27 April 2022, from https://my.clevelandclinic.org/health/diseases/21616-toxic-epidermal-necrolysis-ten