Definisi
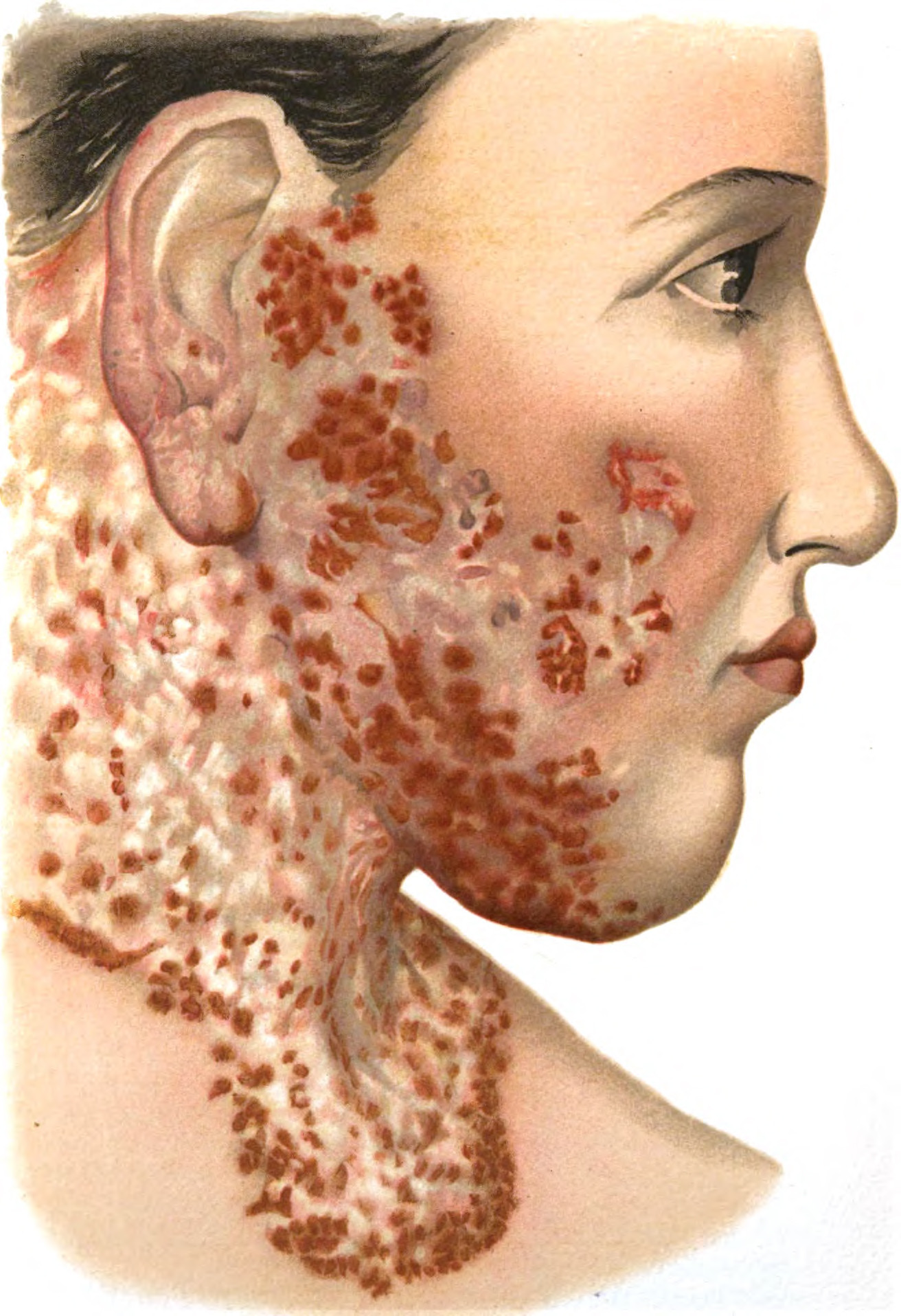
Selulitis merupakan penyakit radang kulit yang mengenai lapisan tengah kulit (dermis) dan disebabkan oleh infeksi bakteri. Selulitis bisa terjadi di area tubuh mana pun, dan biasanya diawali dengan adanya luka pada area kulit dan menjadi tempat masuknya infeksi bakteri. Selulitis dapat menyebabkan area kulit yang terkena menjadi bengkak dan meradang, serta terasa nyeri dan panas saat disentuh. Pembengkakan dan kemerahan yang terjadi dapat melebar dengan cepat. Pada warna kulit yang cerah selulitis tampak berwarna merah, sedangkan pada warna kulit yang gelap selulitis bisa terlihat berwarna abu-abu hingga keunguan.
Selulitis biasanya mengenai area kulit kaki dan tungkai bawah, namun dapat juga terjadi pada wajah, lengan, dan area kulit lainnya. Infeksi bakteri dari selulitis dapat menyebar menuju aliran darah dan menjadi berbahaya hingga mengancam jiwa apabila tidak diberikan tata laksana dengan tepat. Angka kejadian selulitis di Amerika Serikat sebanyak 14 juta kasus setiap tahunnya. Selulitis biasanya terjadi pada dewasa muda hingga tua. Tidak ada perbedaan yang bermakna terkait jenis kelamin laki-laki atau perempuan terhadap angka kejadian selulitis.
Penyebab
Penyebab dari selulitis biasanya infeksi dari bakteri streptokokus golongan beta hemolitikus grup A, seperti bakteri Streptococcus pyogenes. Bakteri Staphylococcus aureus juga menjadi salah satu penyebab selulitis. Selulitis diawali dengan adanya kerusakan pada kulit akibat beberapa hal, misalnya:
- Tergores benda tajam
- Gigitan serangga
- Luka pasca pembedahan
- Luka bakar
Adanya luka pada kulit dapat menjadi jalan masuk bakteri ke dalam lapisan dermis kulit. Sistem kekebalan tubuh akan melawan bakteri tersebut dan menimbulkan reaksi peradangan (inflamasi) pada area kulit yang terkena. Selain itu, bakteri streptokokus melepaskan zat kimia toksin yang memungkinkan bakteri untuk memasuki lapisan yang lebih dalam hingga menyebar ke aliran darah dan berpotensi membahayakan jiwa. Walaupun penyakit ini disebabkan oleh bakteri, selulitis biasanya tidak ditularkan dari orang ke orang.
Faktor Risiko
Pengenalan mengenai beberapa faktor risiko sangat berperan penting dalam pencegahan hingga pengobatan selulitis. Semua orang berisiko mengalami selulitis. Namun, ada beberapa faktor yang dapat meningkatkan risiko Anda mengalami selulitis.
Beberapa faktor risiko tersebut di antaranya:
- Luka atau cedera pada kulit
- Gigitan hewan atau serangga
- Luka operasi
- Luka bakar
- Luka gores atau sayat
- Kondisi medis tertentu yang dapat menurunkan kekebalan tubuh, seperti:
- Diabetes
- Leukemia
- HIV/AIDS
- Mengonsumsi obat rutin dengan efek samping penurunan kekebalan tubuh
- Gangguan pembuluh darah pada tangan atau kaki, seperti varises
- Penyakit liver seperti hepatitis atau sirosis
- Penyakit kulit lainnya seperti dermatitis, psoriasis, atau penyakit infeksi kulit seperti varisela atau cacar air
- Berat badan berlebih
- Memiliki riwayat selulitis sebelumnya
- Terdapat pembengkakan pada lengan atau tungkai karena gangguan aliran kelenjar getah bening (limfedema)
Gejala
Gejala muncul sebagai respon zat kimiawi tubuh terhadap invasi bakteri asing di dalam dermis. Gejala yang dapat Anda rasakan bila Anda mengalami selulitis antara lain:
- Kulit kemerahan dan bengkak
- Kulit teraba hangat dan nyeri saat ditekan
Anda disarankan untuk pergi ke unit gawat darurat apabila Anda memiliki beberapa gejala berikut ini:
- Demam tinggi hingga menggigil
- Mual hingga muntah
- Area yang terkena selulitis mengalami pembesaran dan pengerasan
- Nyeri yang dirasa semakin bertambah berat
- Area kulit yang terkena menjadi kebas atau baal
Diagnosis
Diagnosis selulitis merupakan diagnosis klinis, artinya dokter dapat menetepkan diagnosis selulitis melalui wawancara medis khusus dan pemeriksaan fisik pada Anda, yang secara umum bisa dilihat melalui tampilan yang khas pada area kulit yang terkena selulitis. Meskipun demikian, ada beberapa pemeriksaan penunjang yang dapat membantu seorang dokter untuk menetapkan diagnosis pasti dari penyakit selulitis.
Beberapa pemeriksaan penunjang tersebut di antaranya:
- Pemeriksaan darah lengkap (seperti leukosit dan hitung jenisnya) apabila diduga infeksi menyebar ke dalam aliran darah
- Pemeriksaan rontgen apabila diduga ada benda asing pada kulit atau tulang yang ada di bawah area kulit yang terkena selulitis
- Kultur darah apabila dibutuhkan
Sebaiknya Anda beritahu dokter bila Anda pernah mengalami selulitis sebelumnya. Informasi seperti kapan pertama kali gejala muncul juga akan membantu dokter mendiagnosis dan menentukan penanganan terbaik pada saat pasien pertama kali diperiksa oleh dokter.
Tata Laksana
Selulitis memerlukan penanganan yang komprehensif. Anda disarankan untuk:
- Mengistirahatkan area yang terkena
- Meninggikan atau mengangkat area kulit yang terkena untuk meredakan bengkak dan rasa nyeri
- Mengonsumsi obat pereda nyeri yang dijual bebas, seperti parasetamol atau ibuprofen untuk meringankan rasa nyeri dan juga meredakan demam bila ada
Apabila infeksi yang ada tidak serius, Anda akan diminta oleh dokter untuk mengonsumsi antibiotik dalam waktu minimal 5 hari. Apabila infeksi Anda merupakan infeksi yang serius, maka Anda perlu dirawat inap dan akan mendapatkan obat-obatan melalui suntikan sampai infeksi terkendali sekitar 2 – 3 hari. Setelah pengobatan di rumah sakit atau fasilitas kesehatan, akan dilanjutkan dengan obat minum di rumah.
Komplikasi
Saat seseorang mengalami selulitis, komplikasi akan muncul apabila selulitis tersebut tidak ditangani dengan tepat. Beberapa komplikasi yang dapat timbul antara lain:
- Infeksi yang menyebar melalui darah dan menyebabkan kegagalan organ (sepsis)
- Infeksi pada tulang (osteomyelitis)
- Infeksi pada pembuluh darah limfe (limfangitis)
- Peradangan lapisan dalam jantung (endokarditis)
- Infeksi pada selaput pembungkus otak dan tulang belakang (meningitis)
- Kematian jaringan pada area yang mengalami selulitis (gangren) juga bisa terjadi
Selain itu, komplikasi seperti necrotizing fasciitis juga dapat timbul, yang merupakan kondisi emergensi akibat infeksi kulit pada lapisan terdalamnya. Kejadian selulitis berulang dapat merusak aliran drainase limfatik yang dapat menyebabkan bengkak yang kronis pada area kaki yang mengalami selulitis.
Pencegahan
Setelah mengenali beberapa faktor risiko yang anda miliki, langkah berikutnya adalah perbaikan faktor risiko yang dapat diperbaiki. Berikut langkah-langkah yang dapat anda lakukan, yaitu:
- Jaga kulit tetap lembap dengan losion atau krim pelembap agar kulit tidak mudah rusak
- Gunakan sepatu yang cocok dengan kaki dan berikan ruangan yang cukup untuk kaki saat menggunakan sepatu
- Potong kuku kaki secukupnya tanpa melukai area kulit sekitarnya
- Gunakan alat pelindung khusus apabila berolahraga
- Bersihkan dengan sabun dan air yang mengalir dengan perlahan disertai pemberian petroleum jelly apabila ada kerusakan pada kulit
- Tutup kulit yang terluka dengan plaster dan diganti tiap hari
- Perhatikan tanda-tanda infeksi, seperti kemerahan, nyeri, atau bengkak
- Jangan lupa untuk mengikuti regimen obat Anda sesuai arahan dokter
Selain langkah-langkah di atas, apabila Anda tidak pernah memeriksakan diri ke dokter, sebaiknya lakukan pemeriksaan umum dan bila ditemukan kondisi atau penyakit dapat meningkatkan risiko Anda mengalami selulitis, maka dapat dimulai pengobatan sedini mungkin sebelum kondisi semakin parah.
Kapan Harus ke Dokter?
Jika Anda mengalami gejala yang menyerupai selulitis, atau sedang mengobati sendiri dari selulitis namun muncul gejala tambahan seperti demam berkepanjangan, mudah mengantuk, lemas, ada lenting di sekitar selulitits, atau kemerahan yang makin melebar, sebaiknya Anda memeriksakan diri lebih lanjut ke dokter spesialis kulit dan kelamin (Sp.KK) atau spesialis dermatologi dan venerologi (Sp.DV). Dokter akan melakukan wawancara medis, pemeriksaan fisik, hingga pemeriksaan penunjang tertentu untuk menetapkan diagnosis pasti dan tata laksana yang tepat.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Hanifa Rahma
Mayo Clinic. Cellulitis. May 2022. Available from: https://www.mayoclinic.org/diseases-conditions/cellulitis/symptoms-causes/syc-20370762
Web MD. Cellulitis. July 2020. Available from: https://www.webmd.com/skin-problems-and-treatments/guide/cellulitis
Medscape. Cellulitis. April 2022. Available from: https://emedicine.medscape.com/article/214222-overview#a1
Brown BD, Hood Watson KL. Cellulitis. [Updated 2021 Dec 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549770/
Healthline. Cellulitis. March 2022. Available from: https://www.healthline.com/health/cellulitis
Medline Plus. Cellulitis. April 2020. Available from: https://medlineplus.gov/cellulitis.html
Medline Plus. Cellulitis. April 2021. Available from: https://medlineplus.gov/ency/article/000855.htm