Definisi
Stevens-Johnson Syndrome (SJS) atau yang dulu dikenal dengan nama sindrom Lyell, merupakan reaksi kulit dan selaput lendir yang langka, tidak terprediksi, dan berpotensi fatal. Bentuk yang lebih berat dari kondisi ini adalah nekrolisis epidermal toksik (NET).
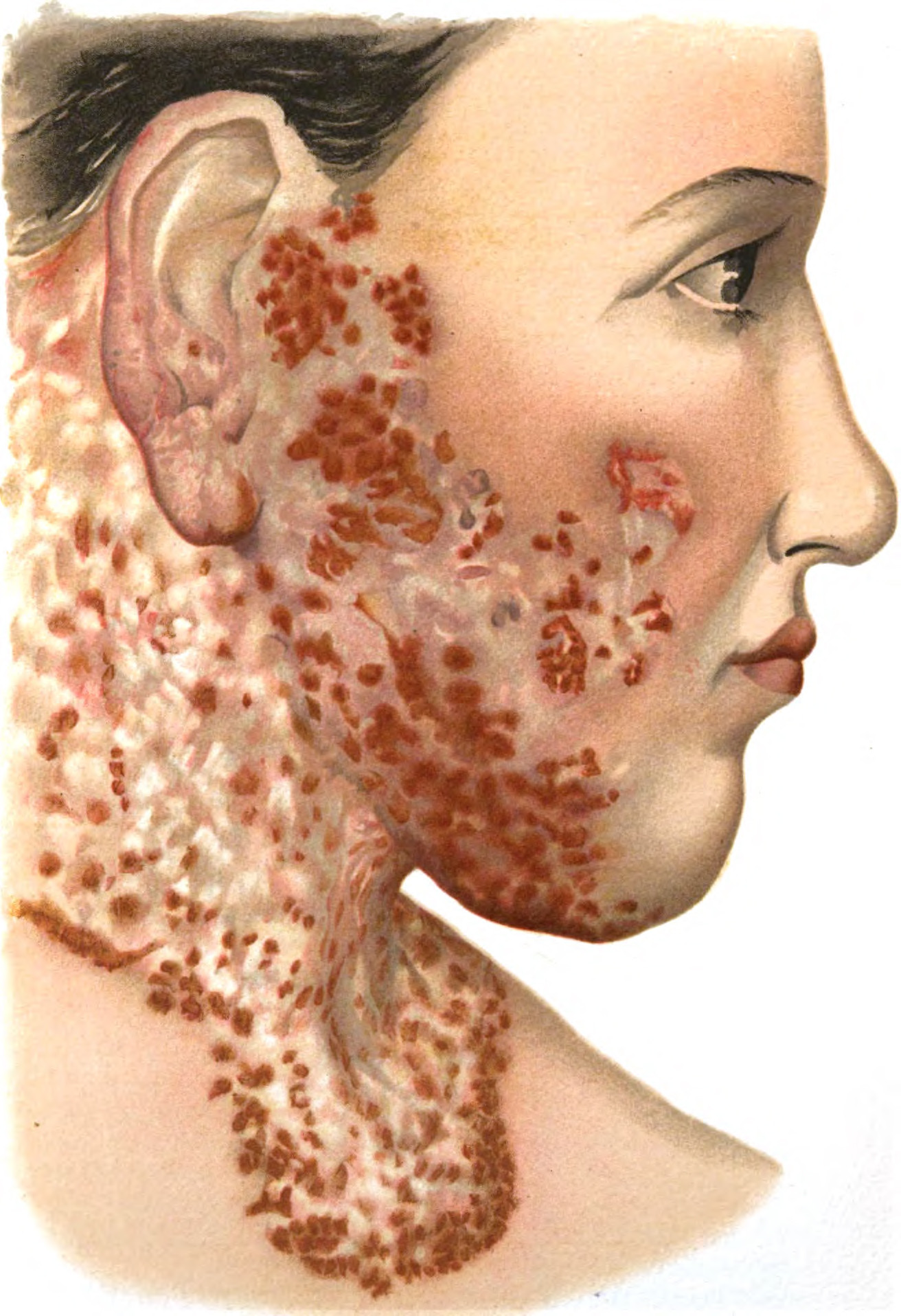
SJS diperkirakan menyerang dua sampai tujuh dari setiap juta orang setiap tahunnya. SJS tiga kali lebih umum ditemukan daripada NET. Obat-obatan umumnya merupakan penyebab pada lebih dari 80% kasus SJS. Reaksi bisa diawali dengan keluhan seperti flu, yang diikuti ruam-ruam menyakitkan dan pengelupasan kulit. Pada sindrom ini, reaksi kulit yang muncul biasanya terjadi pada <10% area permukaan tubuh. Terkadang, SJS dan NET bertumpang-tindih dimana kerusakan permukaan kulit sebesar 10-30% dari area permukaan tubuh.
Stevens-Johnson syndrome merupakan kondisi gawat darurat yang memerlukan penanganan medis segera.
Penyebab
SJS dapat disebabkan oleh berbagai macam hal dan terkadang penyebabnya tidak dapat diidentifikasi. Namun, SJS biasanya merupakan sebuah reaksi terhadap obat-obatan, infeksi, atau keduanya. Obat-obatan merupakan penyebab lebih dari 80% kasus SJS. Reaksi yang dicetuskan oleh obat dapat timbul dalam beberapa hari sampai delapan minggu setelah mulai konsumsi obat, sampai dengan dua minggu setelah penghentian obat tersebut.
Obat-obatan yang dapat menyebabkan SJS meliputi:
- Obat penurun asam urat, seperti allopurinol, terutama pada dosis lebih dari 100 mg per hari
- Obat anti kejang, seperti lamotigrin, karbamazepin, fenitoin, fenobarbiton
- Obat untuk gangguan jiwa, seperti obat anti kejang dan antipsikotik
- Senyawa sulfonamid, seperti kotrimoksazol, sulfasalazin
- Antibiotik, seperti penisilin, sefalosporin, kuinolon, dan minosiklin
- Antivirus nevirapin
- Obat anti nyeri, seperti asetaminofen, ibuprofen, dan natrium naproxen
- Zat kontras untuk pemeriksaan radiologi
Sementara itu, infeksi seperti pneumonia (infeksi paru) dan HIV juga dapat menyebabkan SJS.
Faktor Risiko
SJS dapat terjadi pada siapapun, namun lebih banyak ditemukan pada orang tua dan wanita. Secara umum, faktor yang dapat meningkatkan risiko seseorang terkena SJS adalah:
- Infeksi HIV, kejadian SJS lebih banyak 100 kali lipat dibandingkan dengan orang yang tidak menderita HIV.
- Kelemahan sistem imun, dapat ditemukan pada orang yang menjalani transplantasi organ, penderita HIV/AIDS, dan penderita penyakit autoimun
- Penderita kanker, terutama kanker darah, memiliki risiko lebih tinggi untuk terkena SJS
- Riwayat SJS sebelumnya, jika Anda pernah menderita SJS akibat obat-obatan, maka Anda berisiko untuk terkena SJS lagi jika mengonsumsi obat yang sama
- Riwayat keluarga dengan SJS seperti ada saudara kandung yang terkena SJS, maka risiko Anda untuk mengalami hal yang sama juga lebih tinggi
- Faktor genetik, beberapa orang memiliki variasi genetik yang membuatnya lebih rentan terkena SJS, terutama jika orang tersebut juga mengkonsumsi obat-obatan seperti antikejang, obat asam urat, atau obat gangguan jiwa lainnya
Gejala
Setelah terpapar dengan penyebab atau pencetus yang spesifik, biasanya SJS diawali dengan gejala seperti flu. Gejala ini timbul satu sampai tiga hari sebelum ruam muncul dan meliputi:
- Demam
- Tidak nafsu makan
- Batuk dan pilek
- Sakit pada mulut dan tenggorokan
- Kelelahan
- Sensasi terbakar atau panas pada mata
- Nyeri otot
Seiring dengan perjalanan penyakit, gejala lainnya akan muncul yaitu:
- Sensasi nyeri pada kulit di semua bagian tubuh yang tidak dapat dijelaskan
- Ruam berwarna kemerahan atau keunguan yang nyeri dan menyebar di seluruh tubuh
- Lepuhan pada kulit dan selaput lendir mulut, hidung, mata, dan alat kelamin. Beberapa hari setelah lepuhan terbentuk, lapisan atas dari kulit yang terkena akan mati, mengelupas, dan akan mulai mengalami penyembuhan dalam beberapa hari.
Diagnosa
Dokter biasanya dapat mengidentifikasi adanya SJS berdasarkan riwayat kesehatan Anda, riwayat obat yang sedang Anda konsumsi maupun yang baru dihentikan, serta dengan melakukan pemeriksaan fisik. Diagnosa SJS umumnya sudah cukup jelas dari tampilan reaksi kulit pada tubuh pasien. Untuk mengonfirmasi diagnosis dan menyingkirkan kemungkinan penyebab lainnya, dokter dapat melakukan pemeriksaan biopsi dengan cara mengambil sampel kulit untuk diperiksa di bawah mikroskop.
Selain itu, untuk mencari adanya infeksi, dokter dapat mengambil sampel dari kulit, jaringan, atau cairan tubuh untuk pemeriksaan kultur di laboratorium. Bergantung dengan gejala yang Anda alami, dokter mungkin juga akan melakukan pemeriksaan radiologi seperti rontgen dada untuk melihat adanya pneumonia. Pemeriksaan darah juga dapat dipakai untuk mengkonfirmasi adanya infeksi atau penyebab lain selain SJS.
Tata Laksana
Terapi SJS berfokus pada menghilangkan penyebabnya, merawat luka, mengontrol nyeri, dan meminimalisir komplikasi saat kulit mengalami penyembuhan. Perawatan untuk SJS biasanya membutuhkan ruangan intensif atau ruang perawatan untuk luka bakar.
Hal pertama dan paling penting dalam terapi SJS adalah menghentikan obat yang mungkin menjadi penyebab. Jika ada dua obat atau lebih yang sedang dikonsumsi, dokter mungkin akan menyarankan untuk menghentikan semua obat yang tidak esensial.
Setelah itu, terapi yang akan diberikan di rumah sakit adalah:
1. Terapi penggantian cairan dan nutrisi
Oleh karena kehilangan cairan dapat signifikan, maka penggantian cairan tubuh merupakan bagian terapi yang penting. Cairan dan nutrisi akan dimasukan melalui selang yang dimasukan ke hidung menuju lambung (selang nasogastrik).
2. Perawatan luka
Kompres basah dan sejuk dapat membantu memberi kenyamanan selagi lepuhan mengalami penyembuhan. Dokter juga mungkin akan membuang kulit mati secara lembut dan memberikan petroleum jelly (Vaseline) atau penutup luka yang mengandung obat pada luka kulit.
3. Perawatan mata
Dokter spesialis mata mungkin juga akan terlibat dalam perawatan mata.
Obat-obatan yang digunakan untuk menangani SJS meliputi:
- Obat untuk mengontrol nyeri
- Obat untuk mengurangi peradangan pada mata dan selaput lendir (obat steroid oles atau tetes)
- Antibiotik untuk mengontrol infeksi jika dibutuhkan
- Obat-obatan minum atau suntikan, seperti kortikosteroid dan immunoglobulin suntik
Jika penyebab SJS dapat disingkirkan atau dihilangkan dan reaksi kulit berhenti, maka kulit baru akan mulai tumbuh dalam beberapa hari. Pada kasus yang berat, penyembuhan secara total dapat membutuhkan beberapa bulan.
Komplikasi
SJS dapat menyebabkan komplikasi seperti:
- Pada SJS, terjadi pengelupasan kulit yang dapat menyebabkan tubuh kehilangan cairan. Selain itu, luka pada mulut dan tenggorokan juga menyulitkan proses makan dan minum, sehingga akan timbul dehidrasi.
- Infeksi darah (sepsis). Sepsis terjadi ketika bakteri yang didapatkan dari infeksi masuk ke aliran darah dan menyebar ke seluruh tubuh. Sepsis merupakan kondisi yang dapat memburuk dengan cepat dan mengancam nyawa karena dapat menyebabkan syok dan gagal organ.
- Gangguan pada mata. Ruam yang ditimbulkan oleh SJS dapat menyebabkan peradangan pada mata, mata kering, dan sensitivitas terhadap cahaya. Pada kasus yang jarang, SJS dapat mneyebabkan gangguan penglihatan bahkan kebutaan (jarang).
- Gangguan pada paru. SJS dapat menyebabkan situasi gawat darurat dimana paru tidak dapat menghantarkan oksigen yang cukup ke dalam darah.
- Kerusakan kulit permanen. Ketika kulit tumbuh kembali setelah terkena SJS, pertumbuhan kulit dapat tidak sempurna. Kulit dapat berbenjol-benjol dan berwarna lebih gelap, serta dapat juga disertai dengan bekas luka. Kerusakan kulit ini dapat menyebabkan kerontokan rambut, serta gangguan pertumbuhan kuku jari tangan dan kaki.
Pencegahan
SJS bisa disebabkan oleh obat dan infeksi. Bila penyebabnya merupakan obat-obatan, maka pencegahannya adalah dengan menghindari obat tersebut atau obat yang serupa seumur hidup. Hal ini sangat penting karena kekambuhan biasanya lebih parah dari episode pertama dan dapat bersifat fatal.
Jika Anda memilki keluarga kandung yang menderita SJS setelah mengkonsumsi obat tertentu, Anda juga sebaiknya menghindari obat tersebut karena kondisi ini terkadang diturunkan dalam keluarga.
Kapan Harus ke Dokter?
Penyakit ini merupakan sebuah kegawatdaruratan medis sehingga membutuhkan pertolongan medis seera. Jika Anda mengalami tanda dan gejala SJS, segera cari pertolongan medis.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Hanifa Rahma
Stevens-Johnson syndrome - Diagnosis and treatment - Mayo Clinic. Mayoclinic.org. (2022). Retrieved 20 May 2022, from https://www.mayoclinic.org/diseases-conditions/stevens-johnson-syndrome/diagnosis-treatment/drc-20355942.
Oakley, A., & Krishnamurthy, K. (2022). Stevens Johnson Syndrome. Ncbi.nlm.nih.gov. Retrieved 20 May 2022, from https://www.ncbi.nlm.nih.gov/books/NBK459323/.
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) - Dermatologic Disorders - MSD Manual Professional Edition. MSD Manual Professional Edition. (2022). Retrieved 20 May 2022, from https://www.msdmanuals.com/professional/dermatologic-disorders/hypersensitivity-and-reactive-skin-disorders/stevens-johnson-syndrome-sjs-and-toxic-epidermal-necrolysis-ten.