Definition
Osteoarthritis (OA) is an inflammatory joint disease that results in pain and stiffness within the joints. It is the most prevalent form of arthritis, affecting millions globally.
Although OA can potentially damage any joint, it most commonly impacts the hands, hips, knees, and spine. The progression of joint deterioration in osteoarthritis is gradual, with symptoms worsening over time. In some instances, osteoarthritis may lead to diminished joint function and limitations in daily activities.
Read more: Arthritis - Definition, Causes, Symptoms, and Management
Causes
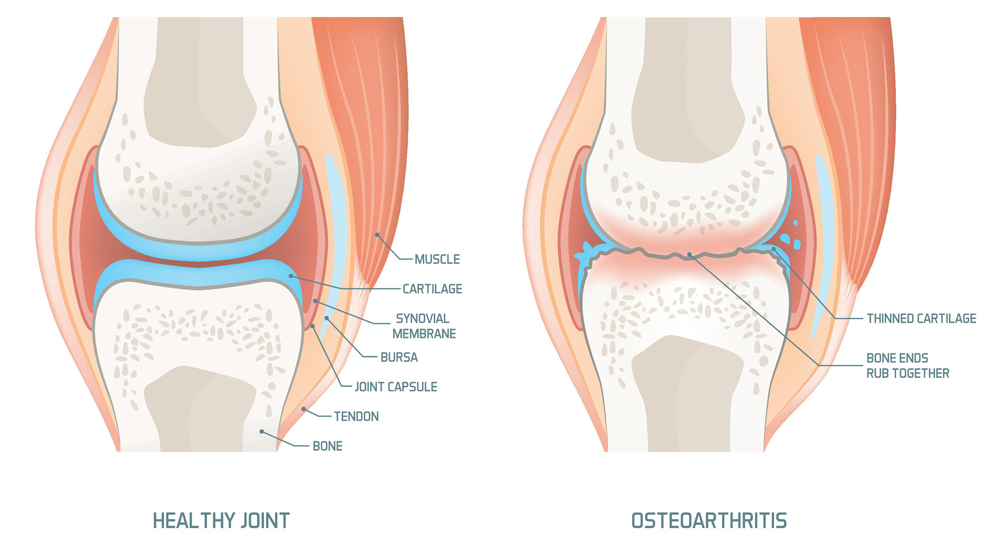
A joint space comprises two bone structures and the cartilage between them. This joint cartilage is a dense, smooth tissue that cushions between the ends of the bones. This structure allows the joint to move with minimal friction between the bones.
OA is caused by the degeneration of the joint cartilage that lies between the ends of two bones. With aging and the continued use of the joint, this cartilage wears away, causing the bone ends within the joint space to rub against each other during movement. In addition to cartilage damage, OA can affect all parts of the joint, leading to damage to the ligaments and tendons.
Risk factor
Some factors that can increase the risk of osteoarthritis are:
- Injury
Injuries can damage joints and increase the risk of osteoarthritis, whether from sports or accidents. Even injuries that occurred years ago and seemed to have healed can still elevate the risk of OA. - Excessive Joint Use
Jobs or sports that involve repetitive stress on the joints can lead to joint damage and increase the risk of osteoarthritis in those joints. - Age
The risk of developing OA increases with age, although not every elderly individual will experience this condition. - Gender
Women are more likely to develop OA compared to men, especially after the age of 50. - Obesity
Excess weight puts more strain on weight-bearing joints, such as the hips and knees. The heavier you are, the greater the pressure on these joints, thereby increasing the risk of OA. Additionally, proteins produced by fat tissue can cause inflammation in and around the joints. - Genetics
Individuals with a family history of osteoarthritis are more likely to develop the condition. Some people also have a genetic predisposition to developing osteoarthritis later in life. - Certain Medical Conditions
Some people are born with joint or cartilage abnormalities. Additionally, other diseases such as diabetes and hemochromatosis (excess iron in the body) can also play a role.
Symptoms
OA symptoms often develop gradually and worsen over time. The signs and symptoms of OA include:
- Joint pain that occurs during or after movement.
- Joint stiffness, is often most noticeable upon waking or after a period of inactivity.
- Tenderness when applying pressure to or touching the affected joint.
- Loss of flexibility or a reduced range of motion, making it difficult to fully move the joint.
- Swelling due to inflammation of the tissues surrounding the joint.
- Crepitus, a grating sensation, may be felt when moving the joint.
Diagnosis
Your doctor will inquire about your symptoms and medical history in detail. They will then perform a physical examination of the affected joint to check for signs of inflammation and any limitation in joint movement.
To obtain a clear image of the affected joint, the doctor may conduct the following tests:
- Laboratory Tests
There is no specific blood test to diagnose OA, but joint fluid can be analyzed to check for inflammation or signs of infection. - X-ray
Although cartilage is not visible on X-rays, cartilage loss will appear as a narrowing of the space between the bones in the joint. - MRI
This imaging technique uses radio waves and strong magnetic fields to produce detailed images of bones and soft tissues. While an MRI is not typically necessary to diagnose OA, it can provide additional information in more complex cases.
Management
There is no cure for osteoarthritis, so treatment is primarily focused on managing symptoms and preventing disease progression. Your doctor may prescribe pain relievers to address the discomfort. Pain medication should be taken under medical supervision, as excessive use can lead to complications. Assistive devices, such as a cane, may help with walking.
If the above treatments are not effective, your doctor may recommend steroid injections into the affected joint. Surgery may also be an option if other therapies do not provide relief. Discuss your treatment plan with your doctor, especially if you have other medical conditions such as diabetes or heart disease.
In addition to the treatments above, individuals with OA can regain confidence in managing their condition through self-management strategies. These strategies help reduce pain and disability, allowing those with OA to continue engaging in activities that are important to them. Self-management strategies for managing arthritis and its symptoms include:
- Staying Physically Active
Experts recommend that adults engage in low- to moderate-intensity physical activity for 150 minutes each week. Recommended activities include walking, swimming, and cycling. Regular physical activity can also reduce the risk of other diseases, such as heart disease, stroke, and diabetes. - Weight Loss
For those who are overweight or obese, losing weight will reduce the pressure on joints, particularly weight-bearing joints such as the hips and knees. Achieving a healthy weight can reduce pain, improve function, and slow the progression of OA. - Joint Protection
Joint injuries can cause or worsen OA. Choose joint-friendly activities such as walking, cycling, and swimming. These low-impact activities carry a lower risk of injury and do not place excessive pressure or twisting on the joints.
Complications
Osteoarthritis is a condition that can worsen over time and often leads to chronic pain. In some cases, joint pain and stiffness can become so severe that they impair function and cause disability. Some individuals may become unable to perform daily activities or work. Depression and sleep disturbances may arise due to the pain and disability associated with OA.
Read more: Depression - Definition, Causes, Symptoms, And Management.
Prevention
There are several ways to prevent osteoarthritis or reduce its progression:
- Maintain a healthy weight.
- Exercise regularly to strengthen muscles and reduce the risk of osteoarthritis.
- Avoid joint injuries by doing the following:
- Warm up before exercising and cool down afterwards.
- Wear properly fitting and comfortable shoes during activities.
- Exercise on soft, even surfaces to prevent injuries.
- Eat a balanced diet. Although no specific diet has been proven to prevent OA, certain nutrients have been associated with reduced risk or severity of osteoarthritis, such as omega-3 fatty acids and vitamin D.
Read more: Vitamin D - How It Works, Indications, Contraindications, and preparations.
When to see a doctor?
If you experience persistent joint pain or stiffness that does not go away, it is advisable to consult a doctor.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Osteoarthritis. (2020). Retrieved 11 August 2022, from https://www.cdc.gov/arthritis/basics/osteoarthritis.htm.
Osteoarthritis - Diagnosis and treatment - Mayo Clinic. (2021). Retrieved 11 August 2022, from https://www.mayoclinic.org/diseases-conditions/osteoarthritis/diagnosis-treatment/drc-20351930.
Osteoarthritis Prevention. (2020). Retrieved 11 August 2022, from https://www.webmd.com/osteoarthritis/osteoarthritis-prevention-1.