Definition
Lymphadenopathy is the swelling of lymph nodes in response to various medical conditions. Diseases that can cause lymph node enlargement include:
- Infections caused by viruses, bacteria, or fungi.
- Autoimmune diseases affecting the immune system.
- Cancer or malignancies.
The swelling of lymph nodes indicates that the immune system is actively working to clear infections or combat foreign microbes in the body.
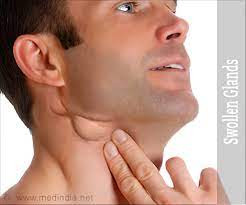
When feeling unwell, you may notice swelling on the sides of your neck, which could be swollen lymph nodes. These nodes serve as filters, aiding in the removal of organisms, cells, or other foreign substances from the lymph fluid. Lymph fluid is a clear or slightly yellowish liquid containing white blood cells, proteins, and fats.
Swollen lymph nodes can occur in various regions of the body, including the neck, armpits, under the jaw, and in the groin creases. While some lymph nodes are palpable externally, many are not. There are over 600 lymph node tissues (though the exact count varies between individuals) distributed throughout areas such as the jaw, chest, arms, abdomen, and legs.
Causes
Upper respiratory tract infections are the most common cause of lymphadenopathy in the neck, and they typically take 10-14 days to resolve fully. As you begin to feel better, the swelling of the lymph nodes should gradually decrease, although it may take several weeks or longer for the swelling to disappear completely.
Other bacterial and viral infections that can lead to lymph node swelling include:
- Sinus infections (sinusitis)
- Skin wounds
- Mononucleosis (viral infection)
As the body fights the ongoing infection, the lymph nodes enlarge as more white blood cells gather to combat the invading pathogens. This accumulation of cells exerts pressure on the nodes, resulting in swelling. Often, the swollen lymph nodes are located near the site of the infection. For instance, if you have a sore throat, you may experience lymphadenopathy in your neck.
Risk factor
Risk factors for lymphadenopathy generally include occupational, environmental, genetic, and viral factors. Other factors that can increase a person's risk of developing lymphadenopathy are:
- High-risk sexual behavior
- Injection drug abuse
- Local soft tissue infections
- Upper respiratory tract infections
- Blood transfusions
- Consumption of undercooked meat
Symptoms
Lymphadenopathy is indeed a symptom that can signal the presence of a specific disease or infection in the body. Doctors can examine swollen lymph nodes to assess the potential underlying cause. During this evaluation, the doctor will typically assess the following:
- The size of the nodes, determining whether they are normal or enlarged.
- Presence of tenderness in the lymph nodes when touched.
- Consistency of the lymph nodes, whether they feel hard or rubbery.
- Mobility of the nodes, assessing whether they can be moved or not.
- Location of the lymph nodes, as certain diseases may be associated with the location of lymph node enlargement in the body.
condition. If the symptoms and physical examination are less characteristic so that it require further evaluation, the supporting examination carried out will depend on the results of clinical findings and the lymph nodes involved.
Most doctors usually choose to monitor initial lymphadenopathy without other clinical findings for 3-4 weeks. However, if there is a suspicion of cancer, further evaluation becomes necessary. In such cases, a CT scan or MRI is commonly performed to assess the extent of lymphadenopathy and identify any associated abnormalities. Based on the imaging results, a biopsy or tissue sampling procedure may be recommended to confirm the diagnosis and guide appropriate treatment.
Diagnosis
If a doctor suspects a specific disease, such as mononucleosis, initial testing will be conducted for that condition. However, if the symptoms and physical examination are not specific and require further evaluation, diagnostic tests will depend on the clinical findings and the lymph nodes involved.
Common diagnostic tests may include:
- Complete blood count
- Chest X-ray
- Infection screening tests such as tuberculosis (TB), serology for HIV, mononucleosis, toxoplasmosis, or syphilis
- Antinuclear antibody testing, particularly if there is suspicion of lupus
Management
In many cases, lymphadenopathy localized to a single area of the body is commonly attributed to a viral infection. Typically, specific treatment is not required, as the condition tends to resolve spontaneously. Over time, the lymph nodes gradually decrease in size and return to their normal state.
However, in some instances of infection, the doctor may prescribe medications to expedite healing. Conversely, if lymph node enlargement is observed in two or more areas of the body, it may indicate a more serious systemic condition, suggesting a widespread infection throughout the body. These systemic conditions may include:
- Autoimmune diseases such as lupus or rheumatoid arthritis
- Toxoplasmosis
- Sexually transmitted infections (STIs) like HIV or syphilis
- Bacterial infections such as Lyme disease or typhoid fever
- Viral infections such as measles or Epstein-Barr virus infection
- Cancers such as lymphoma or leukemia, among others.
Treatment for these medical conditions often requires more aggressive and prolonged therapy. Swollen lymph nodes may also persist after treatment is completed.
For mildly swollen and painful lymph nodes, applying warm compresses and taking over-the-counter pain relievers such as ibuprofen and acetaminophen can provide relief. While these measures may not directly reduce lymph node swelling, they can help alleviate temporary discomfort until the body successfully fights off the infection or disease.
Complications
Lymphadenopathy typically does not cause complications on its own. However, if left untreated, it can exacerbate the underlying disease responsible for lymph node enlargement. In cases of lymphadenopathy associated with progressive autoimmune diseases, this can potentially contribute to the development of cancer or immune system disorders.
Prevention
Lymphadenopathy should not be prevented since it indicates the body's immune response to infection or disease. Since infections can cause lymphadenopathy, it's best to focus on preventive measures against infections. You can take these steps:
- Thoroughly wash your hands
- Avoid touching your eyes and nose
- Maintain distance from sick individuals
- Disinfect surfaces in your home or workplace
- Ensure you get enough sleep, eat healthily, and exercise regularly
When to see a doctor?
Most instances of lymphadenopathy are usually not worrisome and tend to resolve naturally as the infection diminishes. However, doctors may be concerned if the lymph nodes enlarge without an apparent reason. If you notice that your lymph nodes are significantly enlarged but not painful or showing specific signs of infection, it is advisable to consult a doctor.
Contact your doctor if you experience any of the following symptoms, which may indicate a more serious condition:
- Enlarged lymph nodes with a diameter greater than 1 cm.
- Inflammation or redness of the skin above the swollen lymph nodes.
- Lymph nodes that are very painful, hard, fixed to the skin, or rapidly enlarging.
- Discharge of pus or other fluids from the lymph nodes.
- Enlarged lymph nodes are accompanied by symptoms such as weight loss, night sweats, prolonged fever, shortness of breath, or fatigue.
- Lymphadenopathy occurs near the armpits, collarbones, or lower neck (often associated with cancer).
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Swollen lymph nodes (lymphadenopathy/adenopathy): Symptoms & causes (2022) Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/diseases/15219-swollen-lymph-nodes (Accessed: April 17, 2023).
Douketis, J.D. (2023) Lymphadenopathy - cardiovascular disorders, MSD Manual Professional Edition. MSD Manuals. Available at: https://www.msdmanuals.com/professional/cardiovascular-disorders/lymphatic-disorders/lymphadenopathy (Accessed: April 17, 2023).
Lymphadenopathy - StatPearls - NCBI Bookshelf (2022). Available at: https://www.ncbi.nlm.nih.gov/books/NBK558918/ (Accessed: April 17, 2023).