Defnisi
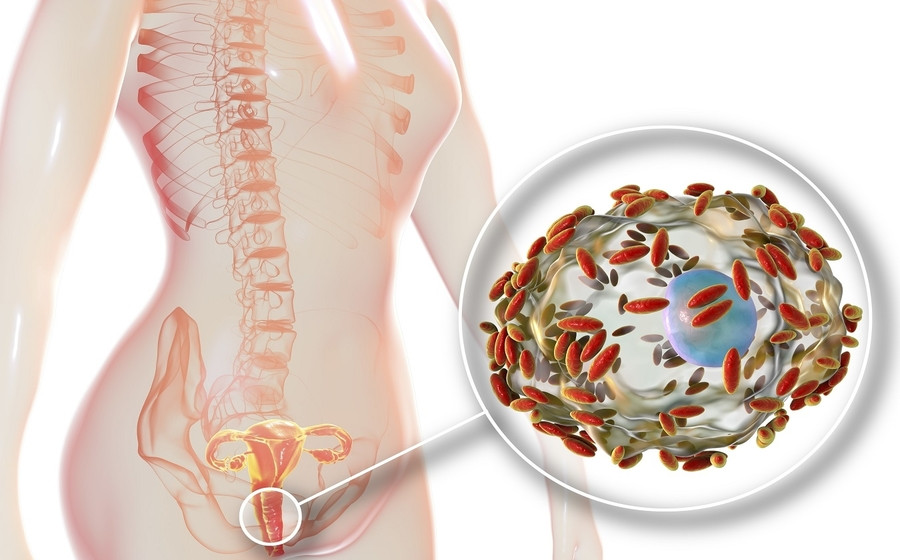
Lymphogranuloma venereum (LGV) is a sexually transmitted disease caused by Chlamydia.
Causes
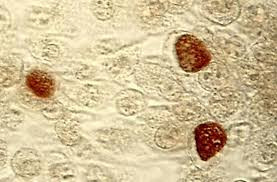
LGV is caused by Chlamydia trachomatis serotypes L1, L2, and L3. These serotypes differ from the chlamydia serotypes that cause eye, urinary tract, and cervical infections because serotypes L1, L2, and L3 can invade and reproduce in the surrounding lymph nodes.
The main mode of transmission of LGV is through unprotected anal, vaginal, or oral sex (such as without the use of a condom).
Risk factor
LGV most commonly occurs in men who have sex with men. LGV in women is very rare.
Additionally, your risk of contracting LGV may increase if you:
- Engage in sexual activity under the influence of illicit drugs
- Engage in sexual activity within groups
- Use sex toys that are not cleaned or covered with a new condom each time they are used
LGV is endemic in some parts of Africa, India, Southeast Asia, South America, and the Caribbean. However, LGV rates are also increasing in North America, Europe, and Australia.
Symptoms
LGV occurs in 3 stages:
- The first stage begins after the incubation period (the period from acquiring the infection to the onset of symptoms), which lasts around 3 days. This stage is marked by small skin abnormalities at the site where the bacteria entered. Ulcer-like sores may form on the skin, healing quickly and often going unnoticed.
- The second stage typically begins in men after about 2 to 4 weeks. It is characterized by enlargement of the lymph nodes in one or both groin folds. This enlargement develops into a large, painful, and sometimes fluctuating lump called an abscess (bubo). Buboes can extend into deeper tissues, causing inflammation of the overlying skin, sometimes accompanied by fever and loss of appetite. In women, back pain or pelvic pain often occurs. The initial abnormalities may appear on the cervix or upper vagina, causing enlargement and inflammation of the lymph nodes around the rectum and pelvis. Tunnel-like passages may form and discharge pus or blood.
- The third stage marks the beginning of healing, characterized by scar tissue formation. However, the formed tunnels may persist or recur. Persistent inflammation due to untreated infection can block lymphatic vessels, leading to swelling and skin ulcers
People who engage in anal intercourse may experience inflammation of the rectum and/or intestines (proctitis and/or proctocolitis), which can be severe and accompanied by the discharge of pus and blood. Additionally, they may experience pain in the anus, constipation, fever, or a feeling of dissatisfaction after bowel movements.
Outbreaks of LGV proctocolitis have been reported in groups of men who have sex with men with high rates of HIV infection.
It's important to note that people with LGV who are asymptomatic can still transmit the infection to their partners.
Diagnosis
A definitive diagnosis of LGV can only be established through specific molecular testing, such as PCR-based genotyping for LGV. This test can differentiate between C. trachomatis LGV and non-LGV C. trachomatis. However, this examination is not widely available, and results are generally not promptly accessible.
Therefore, the diagnosis is typically based on clinical suspicion, geographic location, detection of C. trachomatis at symptomatic sites, and excluding other possible causes.
To check for LGV, swab samples will be taken from the rectum, vagina, throat, or from any sores if present. Urine samples can also be used.
If these samples test positive for chlamydia and the doctor suspects you may have LGV, they will be used for further LGV testing. However, this testing may take up to 3 weeks.
If the only symptom is swollen lymph nodes and sample collection is not feasible, other supportive tests can be conducted, such as chlamydia serology (to detect antibodies to chlamydia). This test can support the diagnosis of LGV but cannot be used as the primary tool for diagnosis.
If you have been diagnosed with LGV, your doctor will recommend a comprehensive STI screening, including tests for gonorrhea, syphilis, and HIV.
Read more : Syphilis - Definition, Causes, Symptoms, and Management
Management
LGV therapy aims to cure the infection and prevent further tissue damage.
LGV is usually treated with doxycycline, which is taken twice daily for three weeks. In some cases, different antibiotics may be used.
People with HIV infection and LGV should receive the same therapy regimen as those without HIV. However, they may potentially require longer therapy because symptom improvement may occur more slowly.
Since LGV test results may take up to 3 weeks, doctors may advise you to start therapy before final results are available.
Tissue swelling and damage in the advanced stage of LGV may not improve even after the bacteria have been killed with antibiotics. Buboes, which are swollen lymph nodes, can be treated by draining the fluid using a needle or with minor surgery if necessary. However, most people respond quickly to antibiotics. Buboes, tunnel-like passages, and rectal narrowing due to scar tissue may require surgery.
Everyone treated for LGV should undergo retesting for chlamydia at least 3 months after completing therapy.
To prevent spreading LGV to your partners, you should avoid sexual activity until you and your partner have completed antibiotic therapy. This includes oral sex and sex with condoms.
Complications
If left untreated, LGV can cause scar tissue and swelling on the skin and permanent swelling of the genital organs. Rectal infections can also result in swelling and scar tissue formation, leading to long-term gastrointestinal complications.
Although rare, the infection can spread through the bloodstream, causing inflammation in the joints or liver.
If your infection is not treated, you can transmit it to your other sexual partners.
Prevention
The best way to prevent all STIs is by practicing safer sexual activities, which include using condoms for vaginal, anal, or oral sex.
If you have a new partner, it's important to ensure that both of you have undergone sexual health screenings before engaging in unprotected sexual intercourse.
When to see a doctor?
If you suspect you may have LGV, contacting a doctor for evaluation and testing is important.
Individuals who have had sexual contact with someone diagnosed with LGV within 60 days before the onset of the person's symptoms should also receive evaluation and testing for chlamydia infection, depending on their exposure. If present, sexual partners will be treated with antibiotics, even if they have no symptoms or if subsequent testing results show negative results.
Looking for more information about other diseases? Click here!
- dr. Monica Salim
Lymphogranuloma Venereum (LGV) (2022) NHS inform. Available at: https://www.nhsinform.scot/illnesses-and-conditions/sexual-and-reproductive/lymphogranuloma-venereum-lgv#:~:text=Lymphogranuloma%20venereum%20(LGV)%20is%20a,in%20women%20is%20very%20rare. (Accessed: April 27, 2023).
Morris, S.R. (2023) Lymphogranuloma Venereum (LGV) - infectious diseases, MSD Manual Professional Edition. MSD Manuals. Available at: https://www.msdmanuals.com/professional/infectious-diseases/sexually-transmitted-infections-stis/lymphogranuloma-venereum-lgv (Accessed: April 27, 2023).
Lymphogranuloma Venereum (LGV) - STI treatment guidelines - CDC (2021). Available at: https://www.cdc.gov/std/treatment-guidelines/lgv.htm (Accessed: April 27, 2023).