Definition
Cervical cancer is a type of cancer that develops in the cervix, the lower part of the uterus that connects the uterus to the vagina. Cervical cancer is one of the most common types of cancer worldwide. Data from the Global Cancer Observatory (Globocan) shows that cervical cancer ranks fourth among the most common causes of cancer in women and resulted in around 600,000 deaths worldwide in 2020. In Indonesia, Globocan data shows that cervical cancer was the second most common cause of cancer in 2020, with about 36,000 cases, accounting for 9% of all cancer cases. Cervical cancer does not affect women who have undergone a total hysterectomy (complete removal of the uterus).
Research indicates that the highest incidence of cervical cancer occurs in young adults before the age of 25, while the highest mortality rate from this disease occurs between the ages of 40 and 50. Cervical cancer primarily develops when risk factors increase the likelihood of cancer from HPV infection.
Causes
Cervical cancer occurs when healthy cells in the cervix undergo changes or mutations in their DNA. DNA contains the information that instructs cells on how to function. Mutations cause cells to grow and divide uncontrollably, resulting in the formation of a mass known as a tumor. Cancer cells can invade other tissues and spread to surrounding parts of the body.
The exact cause of cervical cancer is unknown, but almost all cases (99%) are related to human papillomavirus (HPV) infection. In most cases, HPV infections resolve on their own and do not cause symptoms. However, in persistent infections, HPV can lead to cervical cancer in women. For women with a normal immune system, it takes about 15-20 years for an HPV infection to develop into cancer. In cases of weakened immunity, such as HIV, the time required for cancer to develop is reduced to 5–10 years.
HPV is commonly found in sexually active individuals. There are more than 130 types of HPV, with 20 types capable of causing cancer. HPV types 16 and 18 are the most frequently associated with cervical cancer, causing over 75% of cases.
Risk Factor
Several risk factors can increase a woman’s likelihood of developing cervical cancer, including:
- Age under 45 years old
- Multiple sexual partners, which increases the risk of HPV infection and cervical cancer
- Early sexual activity and pregnancy, especially under the age of 17, which increases the risk of HPV infection
- History of sexually transmitted infections (STIs), such as gonorrhea, syphilis, or HIV/AIDS
- Immunocompromise, or weakened immune system
- Smoking
- A history of vaginal, kidney, or bladder cancer
Symptoms
In the early stages, cervical cancer usually does not show any signs or symptoms. However, symptoms of more advanced stages include:
- Bleeding after sexual intercourse, between menstrual periods, or after menopause
- Vaginal discharge that is bloody and foul-smelling
- Pelvic pain or pain during intercourse (dyspareunia)
Diagnosis
Your doctor will take a medical history and perform a series of examinations to diagnose cervical cancer. They may ask questions about the age of first sexual intercourse, the number of sexual partners, menstrual history, history of diseases such as HPV or HIV infection, and history of HPV vaccination.
A physical examination involves inspecting the external and internal genitalia. Internal examination is performed using a speculum to visualize the cervix, allowing any lesions, erosion, or masses to be identified. However, in early-stage cervical cancer, the cervix usually appears normal.
To confirm a diagnosis, additional tests may be required. One such test is the Papanicolaou (Pap) smear, where a sample is taken from the cervix and examined in a laboratory for abnormalities. Another test that may be conducted is an HPV DNA test to detect the presence of HPV in cervical cells.
If a Pap smear indicates abnormal cervical cells, further investigation is needed. The doctor may perform a colposcopy, where a speculum is inserted into the vagina and a colposcope is used to examine the cervix closely. A biopsy, which involves taking a tissue sample from the cervix for further examination, is often performed during this procedure. A pathologist examines the biopsy tissue under a microscope to determine if there are abnormal cells in the cervix.
Management
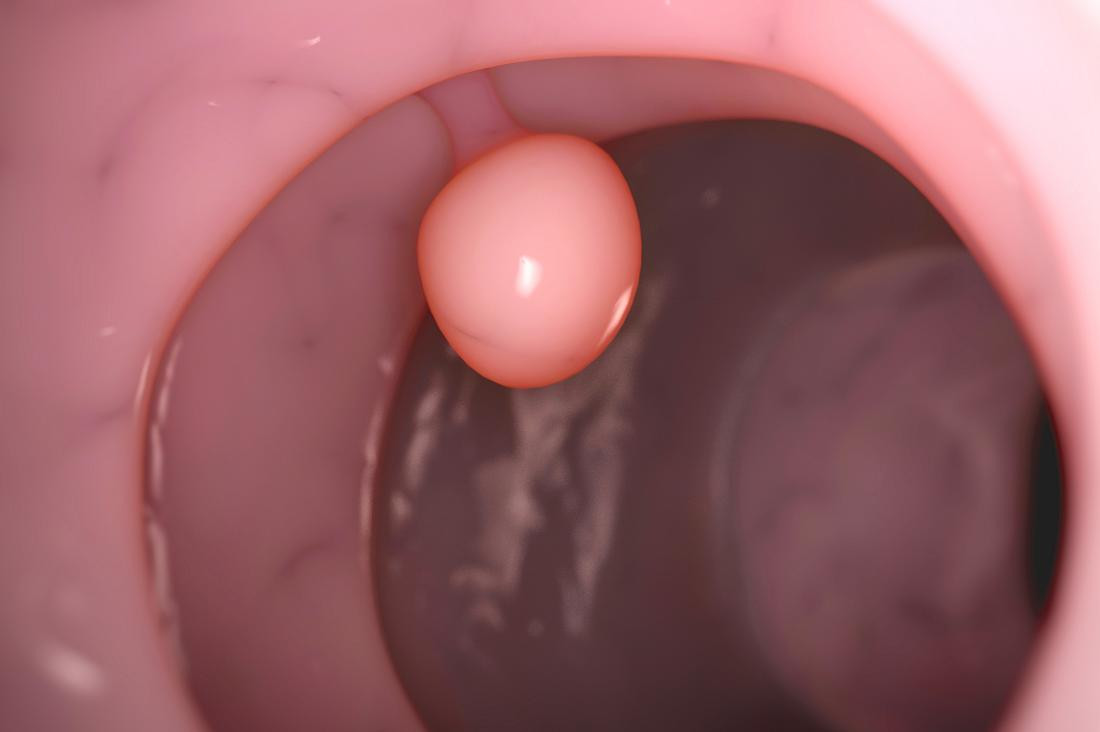
The treatment for cervical cancer depends on the severity of the cancer. According to the 2021 WHO guidelines, if testing indicates the presence of precancerous cells and treatment is needed, an ablation procedure should be performed. Ablation is minimally invasive, meaning it does not involve general anesthesia or large incisions. The doctor inserts a device into the vaginal cavity and uses a camera to perform ablation on the tumor mass, using either high or low temperatures.
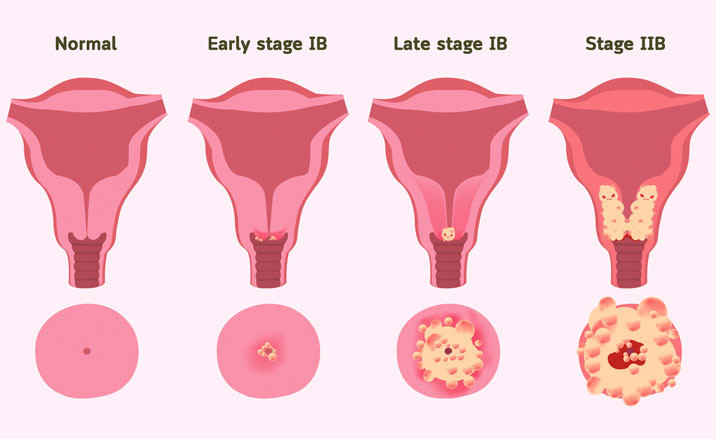
If malignant cells are detected, the doctor will determine the stage of cervical cancer. The cancer stage is determined by the size of the cancer mass and whether it has spread to other parts of the body. Treatment options for malignant cervical cancer depend on the cancer stage and may include surgery, radiotherapy, and chemotherapy.
Complications
The complications of advanced cervical cancer and its treatment are similar to those of other types of cancer. Potential complications include:
- Kidney failure
- Hydronephrosis
- Pain
- Lymphedema
- Bleeding disorders
- Severe complications, such as blindness
Prevention
Several measures can be taken to prevent cervical cancer, including:
- HPV Vaccination: The HPV vaccine is more effective if given before exposure to HPV. WHO recommends that girls aged 9–14 receive the HPV vaccine.
- Routine screening: Tests such as Pap smears, visual inspection with acetic acid (VIA), and HPV DNA testing can be conducted. WHO recommends using HPV DNA tests over VIA and Pap smears due to their objectivity and lower cost. Screening should start at age 30 and be repeated every 5–10 years, while women with HIV/AIDS should be screened every 3-5 years.
- Safe sexual activities: Use condoms to prevent sexually transmitted infections and limit the number of sexual partners.
- Avoid smoking: If you do not smoke, do not start. If you want to quit smoking, consult your doctor for strategies to help you stop.
When to See a Doctor?
You should see a doctor if you experience symptoms of cervical cancer, such as bloody and foul-smelling vaginal discharge, pain during intercourse, or pelvic pain. You should also visit a doctor to receive the HPV vaccine and to undergo cervical cancer screening as recommended.
Looking for more information about other diseases? Click here!
- dr Vivian Keung
Worldwide Cancer Research Fund International. Worldwide cancer data. Retrieved 16 October 2022, from https://www.wcrf.org/cancer-trends/worldwide-cancer-data/
Global Cancer Observatory. (2021). Indonesia - Global Cancer Observatory. Retrieved 16 October 2022, from https://gco.iarc.fr/today/data/factsheets/populations/360-indonesia-fact-sheets.pdf
World Health Organization. (2022). Cervical cancer. Retrieved 16 October 2022, from https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
Fowler, J., Maani, E., & Jack, B. (2022). Cervical Cancer. Retrieved 16 October 2022, from https://www.ncbi.nlm.nih.gov/books/NBK431093/
National Cancer Institute. (2022). Cervical Cancer Diagnosis. Retrieved 16 October 2022, from https://www.cancer.gov/types/cervical/diagnosis
Medscape. (2022). Cervical Cancer: Practice Essentials, Background, Pathophysiology. Retrieved 16 October 2022, from https://emedicine.medscape.com/article/253513-overview#a1
Mayo Clinic. (2021). Cervical cancer - Symptoms and causes. Retrieved 16 October 2022, from https://www.mayoclinic.org/diseases-conditions/cervical-cancer/symptoms-causes/syc-20352501
World Health Organization. (2021). WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention (2nd ed.). World Health Organization.
Centers for Disease Control and Prevention. Cervical Cancer. Retrieved 16 October 2022, from https://www.cdc.gov/cancer/cervical/