Definition
A soft tissue tumor (STT) is a tumor that develops from soft tissue, which provides support to the body's organs. Soft tissue consists of fibrous connective tissue, adipose tissue (fat), bone tissue, blood vessels or lymph vessels, and peripheral nerve tissue. STT can grow anywhere in the body, including muscles, ligaments (bone connectors), tendons (muscle-bone connectors), nerves, fat, and blood vessels.
STTs are classified based on several factors, including location, growth pattern, likelihood of recurrence, spread to other parts of the body, and age. STTs are also classified as benign or malignant (soft tissue sarcomas), though many cases cannot be assigned to either category.
Examples of common types of benign STT are:
- Lipoma
- Angiolipoma (a rare STT consisting of fatty tissue and blood vessels)
- Benign fibrous histiocytoma (sarcoma of soft tissue)
- Neurofibroma (tumor of nerve fibers)
- Schwannoma (tumor in the nerve sheath of the peripheral nervous system)
- Hemangioma (benign tumor of blood vessels)
- Giant cell tumor of the tendon sheath
- Myxoma (a rare benign tumor of connective tissue)
In general, benign STTs are ten times more common than malignant ones. The annual incidence of soft tissue sarcomas is 15 to 35 per 1 million. The rate continues to rise with age and is higher in men than women.
Causes
Some of the factors thought to be contributing to the onset of STT include:
- Genetic factors. Scientific evidence suggests that certain genetic disorders and gene mutations cause the development of both benign and malignant STTs. For example, the NF1 gene in neurofibromatosis causes multiple, potentially malignant neurofibromas (nerve fiber tumors)
- Radiation. Radiation can trigger genetic mutations that transform cells into tumors
- Chronic lymphatic flow disorder (lymphedema). This condition can be found in people with advanced breast cancer. Lymphedema causes a soft tissue sarcoma known as lymphangiosarcoma
- Environmental factors. There is an association between carcinogenic substances and an increased risk of STT. For example, liver angiosarcoma (cancer of the blood vessels) has been linked with exposure to arsenic, thorium dioxide, and vinyl chloride
- Infection. Some STTs, such as Kaposi's sarcoma, are caused by human herpesvirus type 8 infection in HIV patients. Epstein-Barr virus infection in immunocompromised people increases the likelihood of developing STTs
- Injury. Injury may trigger cells that have already undergone mutation actually to grow into a tumor
Risk factor
STT can occur in any segment of the population. However, sarcomas are more common in children and young adults, and in men when compared to women.
Age is a risk factor for specific types of STTs. For example, rhabdomyosarcoma (a rare type of connective tissue cancer) is more common in children and young adults. Synovial sarcoma (a rare cancer that affects the connective tissue in joints) is found in young adults. Malignant fibrous histiocytoma (sarcoma of the soft tissue) and liposarcoma (cancer of the fat tissue) are common in older adults.
Symptoms
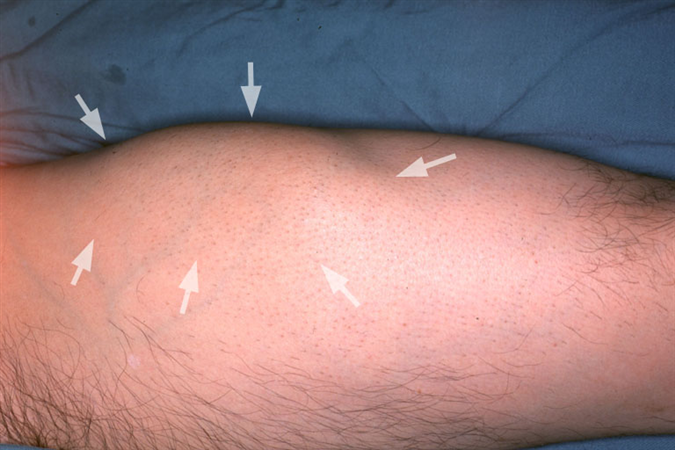
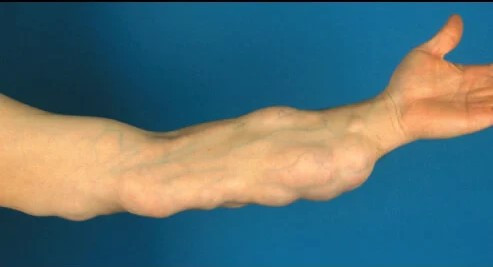
A lump is the most common sign of STT. Lumps are typically painless and do not cause functional impairments such as limb dysfunction. However, depending on its location, the tumor may cause nerve symptoms if it compresses or stretches nerves, irritates tissues, or presses on nearby sensitive structures. The shape and characteristics of STTs vary greatly depending on their type and location.
Benign STTs are typically round, but can also be elliptical or sausage-shaped. Benign STTs are generally more painful to the touch. They are slower growing and mostly smaller than 5 cm in size.
If the lump increases in size rapidly, the presence of a malignant STT can be suspected. Malignant STTs are usually painless, and their surface is not as soft as that of benign STTs. According to the National Cancer Institute, approximately 43% of soft tissue sarcomas occur in the arms and legs, 34% in internal organs, 10% in the chest and back, and 13% in other locations.
Diagnosis
To diagnose STT, your doctor will first inquire about your medical history and symptoms. He will also conduct a physical examination to determine the location, size, rule out other potential causes of pain, and look for involvement of nearby lymph nodes.
Other than the biopsy, no other specific laboratory tests can be used to diagnose STT. Radiologic examinations (X-ray, CT scan, MRI, bone scintigraphy, and PET scan) are useful for managing STT but not for diagnosis. They are more focused on determining the tumor's location, spread, and involvement of other organs or tissues.
A biopsy is typically performed for STTs in patients with no prior history or for lumps that persist for more than 6 weeks after the injury. In addition, all STTs larger than 5 cm, as well as lumps that remain enlarged or symptomatic, should be biopsied. Lumps near the surface, small in size, and do not grow over time may only require observation rather than biopsy.
Early diagnosis of STT is essential for earlier therapy. The biopsy techniques that can be used are:
- FNAB (fine needle aspiration biopsy) is a useful examination for diagnosing palpable or touchable tumors. FNAB is performed using a syringe
- Core needle biopsy is a method of sampling tumor tissue with a hollow core needle. The needle in this examination is larger than that in the FNAB
- An incisional biopsy is a biopsy performed by making an incision in the tumor
- An excisional biopsy is a biopsy that involves the removal of tumor tissue
The choice of biopsy technique is based on the size and location of the lump. An excisional biopsy removes small, near-surface lumps (3-4 cm in diameter) with a low risk of malignancy.
Management
STT can be treated using chemotherapy drugs, radiotherapy, or surgery. Surgery is performed based on the location of the tumor. For most benign STTs, surgical tumor removal is sufficient, with minimal risk to surrounding blood vessels, nerves, muscles, and bones. However, for malignant and recurrent STTs, radiation therapy and chemotherapy may be performed in addition.
Because soft tissue sarcomas tend to recur and recurrence is more challenging to treat than the first occurrence, the tumor must be completely removed followed by radiation therapy. Radiation therapy lowers the chance of recurrence.
Treatment is also determined by the location of the tumor. Tumors that grow in certain locations such as the head and neck, are more likely to involve or be near important structures of the body, making them more difficult to remove.
Complications
Complications can be divided into two categories: those that occur before and after therapy.
Complications that can arise before therapy are:
- Wounds on the skin
- Blood abnormalities
- Bleeding
- Damage to surrounding tissue
- Fractures (if the tumor involves bone)
Complications that can arise after therapy are:
- Infected and non-healing surgical wounds
- Infections due to chemotherapy and radiotherapy that cause a decrease in the immune system
- Benign STT typically does not recur frequently. If they recur, they are usually non-destructive and can be treated by surgically removing the tumor. The pattern of recurrence is fairly predictable. Most tumors recur within 2-3 years. Additional radiation and chemotherapy will help to reduce the likelihood of recurrence. Recurrence is more common in malignant STT
- Tumor spread. Malignant STTs are prone to spread. The most common site of tumor spread is the lungs
Prevention
STT is challenging to prevent due to its various causes. Neurofibroma, for example, is a tumor that can be inherited. Meanwhile, because viral infections cause some types of tumors, exposure to viruses must also be avoided by avoiding physical contact with infected people.
When to see a doctor?
You should consult a doctor if you notice a lump on your body, especially one that grows quickly or measures more than 5 cm.
Looking for more information about other diseases? Click here!
- dr Nadia Opmalina
Benign and Malignant Soft-Tissue Tumors Treatment & Management: Approach Considerations, Medical Therapy, Surgical Therapy. Emedicine.medscape.com. (2022). Retrieved 6 June 2022, from https://emedicine.medscape.com/article/1253816-treatment#d1
Benign Soft Tissue Tumors; Symptoms & Treatment. Cleveland Clinic. (2022). Retrieved 6 June 2022, from https://my.clevelandclinic.org/health/diseases/16778-benign-soft-tissue-tumors
Soft Tissue Masses. Orthop.washington.edu. (2022). Retrieved 6 June 2022, from https://orthop.washington.edu/patient-care/articles/oncology/soft-tissue-masses.html