Definisi
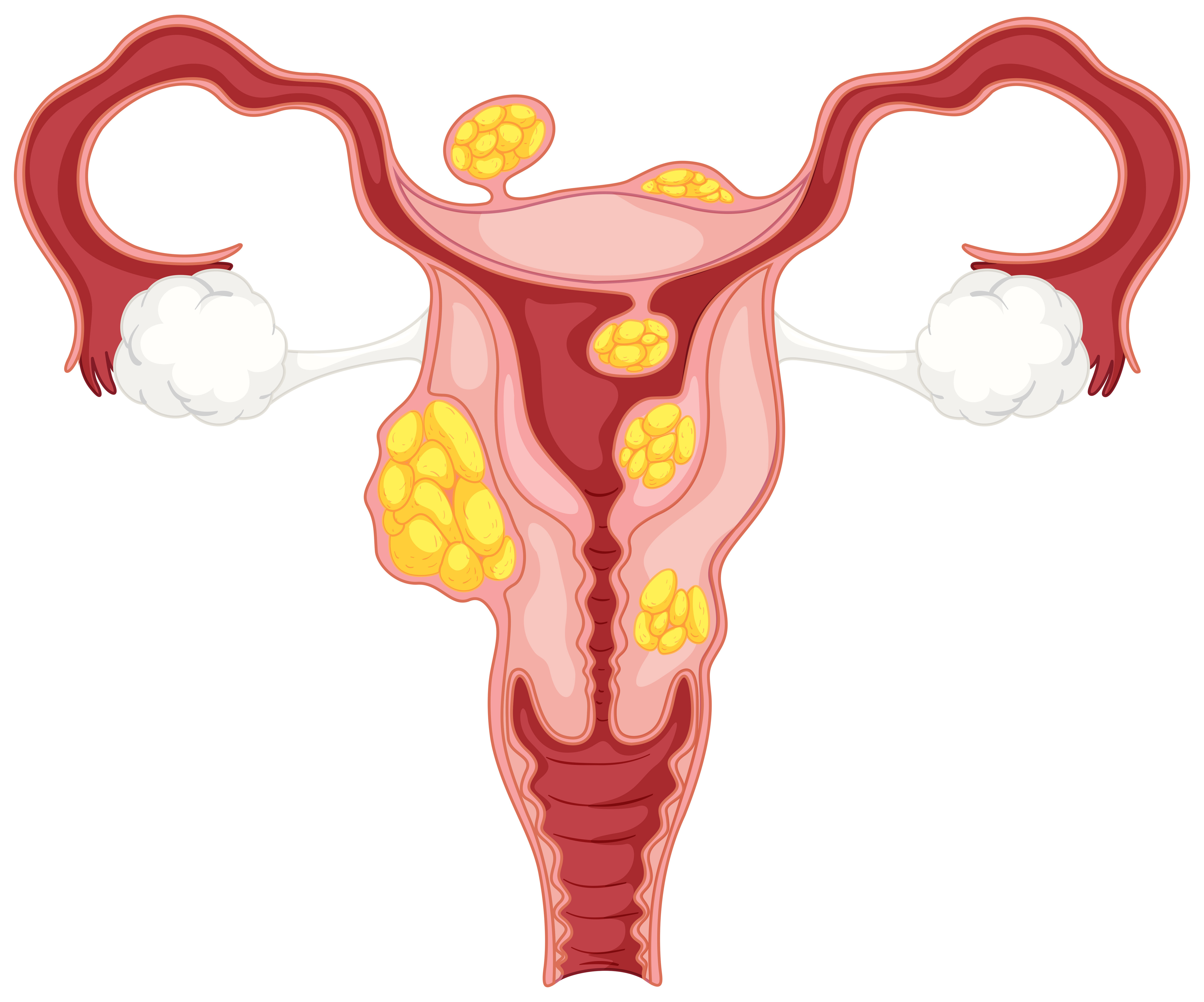
Mioma uteri, yang juga dikenal dengan nama leiomyoma atau fibroid rahim, adalah suatu pertumbuhan massa bersifat jinak yang muncul pada dinding rahim, dalam rahim atau di luar rahim. Mioma uteri berasal dari otot dan jaringan ikat rahim yang tumbuh secara abnormal. Penyakit ini tidak berhubungan dengan peningkatan risiko kanker rahim dan hampir tidak pernah berkembang menjadi kanker.
Mioma uteri adalah salah satu tumor jinak yang paling umum dialami wanita usia subur. Biasanya penyakit ini terjadi pada usia 30-40 tahun, dan jarang terjadi sebelum perempuan memasuki pubertas. Pada banyak kasus, mioma uteri tidak menimbulkan gejala apapun sehingga wanita yang memilikinya tidak sadar akan hal ini. Namun pada 20-50% kasus, mioma uteri menyebabkan gejala dan mungkin memerlukan pengobatan.
Mioma uteri dapat tumbuh sebagai benjolan tunggal atau berkelompok. Ukurannya bervariasi, dengan diameter mulai dari 1 mm hingga 20 cm. Sebagai perbandingan, ukuran mioma dapat ditemukan seukuran biji hingga sebesar buah semangka.
Mioma uteri dibagi menjadi beberapa jenis berdasarkan lokasi dan perlekatannya, yaitu:
- Mioma yang tumbuh pada dinding rahim.
- Mioma yang berada di luar dinding rahim.
- Mioma yang tumbuh pada ruang dalam rahim tempat janin berada.
- Mioma yang berada di luar rahim dan terhubung dengan suatu tangkai tipis.
Karena ukuran, jumlah dan lokasinya bervariasi, gejala dan keparahan penyakit juga berbeda-beda pada setiap orang. Oleh karena itu, pengobatan juga akan disesuaikan dengan kondisi pasien.
Penyebab
Penyebab terjadinya mioma uteri tidak diketahui dengan pasti. Beberapa penelitian menduga bahwa penyakit ini mungkin terjadi karena adanya perletakan sel yang salah di tubuh selama masih dalam kandungan. Diperkirakan ada keterlibatan hormon estrogen dan progesteron terhadap pertumbuhan mioma uteri. Oleh karena itu, pada kondisi ketika hormon estrogen berkurang seperti setelah menopause atau persalinan, ukuran mioma uteri bisa menyusut bahkan menghilang.
Selain teori tersebut, terdapat beberapa faktor yang mungkin dapat menyebabkan mioma uteri, antara lain:
- Perubahaan Genetik
Pada banyak kasus, mioma yang tumbuh mengalami perubahan genetik, sehingga proses pembelahan sel menjadi berbeda dari sel-sel otot rahim normal.
- Hormon
Hormon estrogen dan progesteron, dua hormon yang menstimulasi penebalan dinding rahim pada setiap siklus menstruasi, diketahui dapat meningkatkan pertumbuhan mioma. Reseptor kedua hormon ini lebih banyak ditemukan dalam mioma dibandingkan pada sel otot rahim normal.
- Matriks Ekstrasel (ECM)
ECM adalah material biologis yang dibutuhkan agar sel dapat melekat satu sama lain. Kadar ECM meningkat pada mioma dan membuat massa menjadi lebih berserat. ECM juga dapat menyebabkan perubahan biologis pada sel.
Faktor Risiko
Terdapat beberapa faktor yang dapat meningkatkan risiko tumbuhnya mioma uteri, di antaranya:
- Obesitas atau berat badan berlebih.
- Menstruasi pertama terjadi di usia muda (<10 tahun).
- Usia >40 tahun (hingga terjadi menopause).
- Riwayat anggota keluarga dengan mioma uteri.
- Belum pernah melahirkan.
- Menopause di usia lebih lanjut.
- Kekurangan vitamin D.
- Pola makan yang tinggi konsumsi daging merah, minum alkohol, dan rendah konsumsi sayuran, buah-buahan serta susu.
Sebaliknya, terdapat beberapa faktor yang diketahui dapat menurunkan risiko mioma uteri, yakni:
- Usia menstruasi pertama >16 tahun.
- Telah melahirkan lebih dari satu kali.
- Penggunaan obat kontrasepsi oral.
Gejala
Kebanyakan wanita yang memiliki mioma tidak merasakan gejala apapun, sehingga tidak memerlukan pengobatan selain observasi rutin oleh dokter. Namun, mioma uteri bisa menimbulkan keluhan pada sekitar 20-50% kasus, antara lain:
- Perdarahan yang berlebihan atau nyeri saat haid.
- Keluarnya darah di antara periode haid.
- Anemia bila darah yang keluar terlalu banyak.
- Sensasi perut bagian bawah yang terasa penuh/kembung.
- Frekuensi buang air kecil meningkat (bila mioma menekan kandung kemih).
- Nyeri saat berhubungan seksual.
- Nyeri punggung atau perut bagian bawah.
- Sulit BAB atau sembelit.
- Kram perut.
- Keluarnya cairan dari vagina.
- Ketidakmampuan mengosongkan kandung kemih secara total, ditandai dengan sensasi tidak lampias setelah buang air kecil.
- Perut dirasakan membesar, sehingga terlihat seperti sedang hamil.
Gejala mioma uteri biasanya akan menghilang setelah menopause atau kelahiran akibat terjadinya kadar hormon yang menurun.
Diagnosis
Dokter Anda akan menegakkan diagnosis mioma uteri berdasarkan wawancara medis dan serangkaian pemeriksaan. Deskripsi Anda mengenai gejala-gejala mioma uteri seperti nyeri dan perdarahan menstruasi yang hebat, serta keluhan buang air kecil, dapat menjadi pertimbangan dokter dalam menegakkan diagnosis mioma uteri. Anda juga mungkin ditanya mengenai usia, riwayat haid, riwayat melahirkan, dan riwayat mioma uteri di keluarga Anda.
Pada wanita yang aktif secara seksual, pemeriksaan bagian dalam vagina dan leher rahim wanita mungkin akan dilakukan dengan menggunakan alat spekulum.
Untuk mengonfirmasi keberadaan mioma serta menilai ukuran dan jumlahnya, diperlukan pemeriksaan lain yang dapat dilakukan, di antaranya:
- Ultrasound (USG) transvaginal
Pemeriksaan USG dilakukan dengan menggunakan gelombang suara untuk mendapatkan gambaran struktur bagian tubuh tertentu. Pemeriksaan ini merupakan standar baku untuk mendiagnosis mioma uteri. Stik Probe USG akan dimasukkan melalui vagina untuk mendapat gambaran radiologis dari struktur rahim dan mioma yang mungkin berada di dalamnya. Dari sini, ukuran dan jumlah mioma dapat dinilai. Untuk mendapatkan gambar yang lebih baik, dokter Anda mungkin akan memasukkan cairan zat kontras terlebih dahulu ke dalam rahim sebelum melakukan pemeriksaan USG.
- Histeroskopi
Pemeriksaan ini dilakukan menggunakan alat yang disebut histeroskop, berbentuk seperti teleskop kecil ini akan dimasukkan ke dalam vagina hingga menembus leher rahim (serviks), sehingga bagian dalam rahim dapat terlihat secara langsung.
- Laparoskopi
Pemeriksaan ini dilakukan dengan menggunakan alat yang disebut laparoskop. Dokter akan membuat sayatan di perut untuk memasukka alat ini ke dalam rongga perut. Laparoskop akan mengambil secara langsung gambar mioma yang berada di luar rahim.
Pemeriksaan lain seperti magnetic resonance imaging (MRI) dan computed tomography (CT) scan juga dapat dilakukan, namun jarang diperlukan.
Tata Laksana
Mioma uteri tidak membutuhkan pengobatan apapun jika tidak menyebabkan gejala. Mioma berukuran kecil dapat dibiarkan saja berada di tempatnya. Setelah menopause, pertumbuhan daging yang terjadi akan mengecil tanpa pengobatan. Pada kondisi ini, kunjungan rutin ke dokter spesialis obgyn mungkin akan direkomendasikan untuk mengobservasi ukuran dan gejala mioma uteri.
Jika pengobatan akan diberikan, dokter akan berdiskusi dengan Anda mengenai jenis pengobatan yang akan dipilih. Rencana pengobatan akan bergantung pada:
- Jumlah dan ukuran mioma.
- Lokasi tumbuhnya mioma.
- Gejala yang ditimbulkan.
- Keinginan Anda untuk hamil.
- Keinginan Anda untuk mempertahankan rahim.
Jika dokter Anda menyarankan untuk menggunakan obat-obatan dalam mengatasi mioma uteri, pengobatan akan diberikan untuk mengatasi keluhan yang dialami. Dokter bisa memberikan obat antinyeri, obat untuk menurunkan keluhan perdarahan, dan suplemen zat besi. Obat kontrasepsi dan terapi hormon juga menjadi pilihan pengobatan.
Pada banyak kasus, ukuran mioma akan mengecil setelah menopause dan gejala yang terjadi juga akan ikut menghilang.
Satu-satunya cara untuk mengobati mioma uteri secara pasti adalah operasi pengangkatan rahim (histerektomi). Dengan tidak adanya rahim, maka mioma uteri tidak akan dapat muncul kembali. Prosedur ini direkomendasikan jika mioma berukuran besar atau gejala perdarahan sangat parah. Jika Anda masih ingin hamil di masa depan atau ingin mempertahankan rahim, Anda dapat menjalani operasi myomectomi, dimana hanya mioma saja yang diangkat dari rahim. Namun, mioma memiliki kemungkinan kambuh dan muncul kembali pada 15-33 persen kasus.
Komplikasi
Meskipun tidak berbahaya, terdapat beberapa komplikasi yang dapat terjadi akibat mioma uteri, di antaranya:
- Anemia (kurang sel darah merah) karena keluarnya darah yang berlebihan dari kemaluan, hal ini dapat mengakibatkan timbulnya gejala seperti lemas, pusing, tidak bertenaga, sampai sesak napas.
- Mioma jarang menyebabkan kemandulan, namun jika terjadi, pengobatan dapat mengembalikan kemampuan untuk hamil.
- Mioma dapat meningkatkan risiko komplikasi kehamilan, seperti terpisahnya plasenta dari dinding rahim, terhambatnya pertumbuhan janin, dan persalinan prematur.
Pencegahan
Secara umum, Anda tidak dapat mencegah tumbuhnya mioma. Anda dapat mengurangi risiko dengan cara mempertahankan berat badan ideal, makan sayur dan buah-buahan serta secara rutin melakukan pemeriksaan ke dokter obgyn.
Kapan Harus ke Dokter?
Jika Anda memiliki keluhan siklus menstruasi dan buang air kecil, Anda bisa berkonsultasi dengan dokter untuk mencari tahu apakah hal tersebut normal atau perlu diperiksa lebih lanjut.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Hanifa Rahma
The American College of Obstetricians and Gynecologists. (2022). Uterine fibroids. Retrieved October 22, 2022, from https://www.acog.org/womens-health/faqs/uterine-fibroids.
Cleveland Clinic. (2020). Uterine fibroids: Symptoms, causes, risk factors & treatment. Retrieved October 22, 2022, from https://my.clevelandclinic.org/health/diseases/9130-uterine-fibroids.
Maria Syl D. De La Cruz, & Buchanan, E. (2017, January 15). Uterine fibroids: Diagnosis and treatment. Retrieved October 22, 2022, from https://www.aafp.org/pubs/afp/issues/2017/0115/p100.html.
Mayo Clinic. (2022, September 21). Uterine fibroids. Retrieved October 22, 2022, from https://www.mayoclinic.org/diseases-conditions/uterine-fibroids/diagnosis-treatment/drc-20354294.
National Health Service UK. (2022). Fibroids. Retrieved October 22, 2022, from https://www.nhs.uk/conditions/fibroids/.
Uterine leiomyomata - statpearls - NCBI bookshelf. (2022). Retrieved October 22, 2022, from https://www.ncbi.nlm.nih.gov/books/NBK546680/.