Definition
When your body lacks sufficient oxygen, you may experience hypoxemia or hypoxia. Both are dangerous conditions. Without oxygen, the brain, liver, and other organs can be damaged within minutes of oxygen deficiency.
Hypoxemia is a condition of low oxygen levels in the blood. Meanwhile, hypoxia is a condition of low oxygen levels in tissues or organs. Hypoxemia can cause hypoxia when the blood does not carry enough oxygen to tissues to meet the body's needs and functions.
Causes
Severe asthma attacks can cause hypoxia in adults and children. During an attack, the airways narrow, making getting air into the lungs difficult. The effort expended during coughing to clear the lungs uses more oxygen and can worsen symptoms.
Hypoxia can also occur due to lung damage from trauma or injury.
Other causes of hypoxia include:
- Lung diseases include chronic obstructive pulmonary disease (COPD), emphysema, bronchitis, pneumonia, and pulmonary edema (fluid accumulation in the lungs).
- Strong pain medications and other drugs with respiratory side effects.
- Heart problems.
- Anemia is a decrease in red blood cells carrying oxygen throughout the body.
- Cyanide poisoning. Cyanide is a chemical used to make plastic and other products.
Risk factor
Risk factors that increase the risk of hypoxia include:
- Heart and lung diseases.
- Sleep apnea (a sleep disorder that disrupts breathing).
- Being at high altitudes.
- Consumption of certain medications.
Symptoms
Although symptoms vary among individuals, the most common symptoms of hypoxia are:
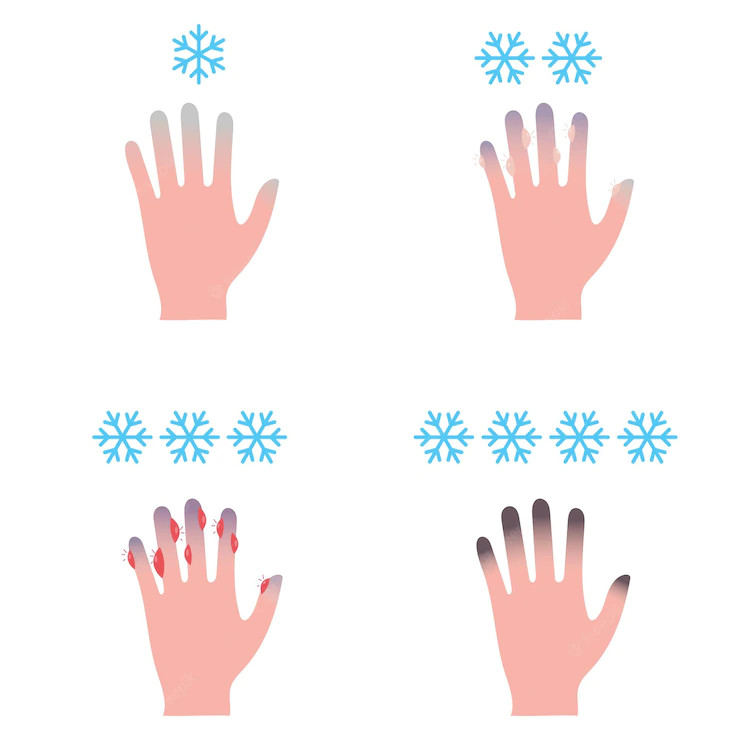
- Changes in skin color, ranging from blue to cherry red.
- Confusion.
- Coughing.
- Heart rate becomes fast or slows down.
- Increased breathing rate.
- Gasping for breath.
- Sweating.
- Wheezing or "panting" breath sounds.
Diagnosis
The doctor will inquire about the patient's complaints and medical history to diagnose hypoxia. After that, the doctor will perform a physical examination to check for signs of hypoxia, such as assessing consciousness levels, examining lip color and nail bed color, and checking blood pressure, respiratory rate, and heart rate.
While conducting the physical examination, the doctor will also provide initial treatment to stabilize the patient's condition.
The doctor will also perform several diagnostic tests, such as:
- Oximetry test, to assess oxygen levels in the blood.
- Complete blood count, to look for signs of anemia or infection.
- Lung function tests, to check if the lungs are functioning normally.
- Blood gas analysis, to assess metabolism and respiration, and the possibility of poisoning.
- Electrocardiogram (EKG) assesses signs of heart damage or irregular heartbeat.
- Chest X-ray or CT scan, to look for lung problems that can cause hypoxia such as pneumothorax or lung infection.
- CT scan or MRI of the head, to look for abnormalities in the brain, such as tumors, stroke, or bleeding.
- Cardiac echo or echocardiography, to assess heart structure and function.
To assess chronic hypoxia (long-lasting), the following tests can be used:
- Pulmonary Functional Test (PFT) or lung function test. This test directly measures lung volume, bronchial response function (throat branch), and diffusion capacity, which can help establish a diagnosis and guide the treatment of lung disorders. As a complementary examination that complements the results of a health history interview and physical examination, this test can be used to differentiate obstructive (blockage) diseases of the respiratory tract, such as bronchial asthma, COPD, or upper respiratory tract obstruction, with restrictive lung diseases (reduced lung capacity to expand) such as interstitial lung disease or chest wall abnormalities. PFTs function to assess the severity of airway obstruction and response to therapy.
- Nocturnal oximetry. This test provides information about oxygen levels in the blood during a certain period, usually overnight. This test mainly assesses the sufficiency or need for oxygen supplementation at night.
- Six-Minute Walk Test. This test provides information about the response of blood oxygen levels to exercise and the total distance that can be traveled in 6 minutes. This information can be used to determine the amount of oxygen to be given and evaluate the response to therapy. This test is often used for lung evaluation before surgery, pulmonary hypertension treatment, and assessment of additional oxygen needs during exercise.
- Hemoglobin. Hemoglobin and red blood cell examinations can serve to see some diseases that cause chronic hypoxia, such as secondary polycythemia, namely an increase in the number of red blood cells.
Management
A person should seek medical attention if experiencing hypoxia to receive treatment and oxygen monitoring promptly.
The most important treatment is to provide sufficient oxygen to the body. Oxygen can be administered through a nasal cannula or oxygen mask. For most people, this treatment is sufficient to normalize oxygen levels.
If you suffer from an asthma attack, inhalers or inhaled asthma medications can make breathing easier. If these medications are not helpful, the doctor may try administering medication intravenously. You may also need steroid medications to reduce lung inflammation or antibiotics to treat accompanying infections.
Respiratory assistance may be necessary when a patient's condition worsens and becomes life-threatening.
Complications
Untreated hypoxia can develop into broader tissue hypoxia, including in the heart and brain. Oxygen deficiency in the brain causes brain tissue damage.
Brain tissue damage can cause patients to lose consciousness and experience organ dysfunction throughout the body. While damage to heart tissue can lead to heart attacks or cardiac arrest. These conditions can be life-threatening.
Excessive oxygen administration in managing hypoxia also carries the risk of complications, namely poisoning the body's tissues and causing cataracts, vertigo, behavioral changes, seizures, and even respiratory system disorders.
Hypoxia can also lead to hypercapnia, a condition where the lungs retain too much carbon dioxide due to difficulty breathing. Increased carbon dioxide in the blood can lead to death. Oxygen and carbon dioxide imbalance in the body often occurs in chronic obstructive pulmonary disease. Chronic hypoxia due to untreated chronic obstructive pulmonary disease can lead to complications:
- Depression and other mood disorders
- Fatigue
- Headache
- Confusion
- High blood pressure (hypertension)
- Pulmonary hypertension
- Increased heart rate
- Heart failure
- Acute respiratory failure
- Secondary polycythemia (increase in red blood cell count)
Prevention
Hypoxia is difficult to prevent because it can occur suddenly. However, some measures can reduce the risk of hypoxia:
- Controlling respiratory diseases, for example, by using asthma medication regularly.
- Practicing breathing exercises.
- Avoiding rapid ascent to certain altitudes to prevent altitude sickness, which is oxygen deficiency due to altitude. The same applies to diving activities. If you ascend to a high altitude or dive to the ocean floor, practice beforehand and use appropriate equipment, such as bringing oxygen tanks and masks while diving.
- Healthy lifestyles include regular exercise, drinking enough water, and quitting smoking.
- Routinely getting checked by a doctor if you have diseases that can increase the risk of hypoxia.
When to see a doctor?
As mentioned above, immediately consult a doctor if you experience symptoms or signs of hypoxia. Prompt examination and treatment are needed to prevent complications.
If you encounter someone who feels short of breath, struggling to breathe, weak, suddenly unable to speak, confused, or experiencing seizures, immediately take them to the emergency room.
- dr Nadia Opmalina
Hypoxia and hypoxemia. (2020). Retrieved 16 February 2022, from https://www.webmd.com/asthma/guide/hypoxia-hypoxemia
Bhutta BS, Alghoula F, Berim I. (2021). Hypoxia. StatPearls Publishing. Retrieved 20 February 2021, from https://www.ncbi.nlm.nih.gov/books/NBK482316/
Schulman JS. (2022). What is hypoxemia?. Retrieved 21 February 2022, from https://www.healthline.com/health/hypoxemia