Definition
Amblyopia, often known as lazy eye, decreases vision caused by visual development disorders during childhood. The incidence of amblyopia in the population is about 2%. It is also the primary cause of vision reduction in one eye in adults aged 20-70.
Causes
Amblyopia most commonly affects one eye. The causes vary, but they all disrupt visual development during childhood. The first common cause is a visual acuity disorder or a problem where the image does not fall precisely on the retina, the part of the eye that receives light. Refractive errors can include:
- Anisometropia (significant difference in refractive error between the two eyes)
- Myopia (nearsightedness)
- Hypermetropia (farsightedness)
These issues risk causing amblyopia if the difference in refractive errors is significant, leading the eye to focus more on the image on the healthier retina.
Other less common causes include obstructions in the eye, such as cloudy eye fluid, retinal diseases, optic nerve diseases, and so on. A frequently heard cause is strabismus (crossed eyes). In strabismus, a child struggles to maintain the position of both eyes, making it easier to control the position of only one eye, which will then be used more frequently.
These conditions can cause amblyopia during the developmental stage of vision. However, amblyopia can be resolved if treated during the subsequent development period. The visual development phase, improving visual acuity from blurry to clear, occurs from birth to about 3-5 years old. The highest amblyopia risk is within the first few months to 7-8 years old. However, amblyopia can be treated in the at-risk ages up to adolescence or young adulthood. This is because amblyopia is generally caused by an imbalance in the use of the optic nerve in both eyes, which becomes harder to correct the older the patient is when starting therapy.
Risk factor
Conditions that cause amblyopia are risk factors for amblyopia. A family history of strabismus, amblyopia, or cloudy eye fluid can increase a child's risk of developing amblyopia.
Additionally, children at higher risk for strabismus, anisometropia, and cloudy eye fluid (such as those with Down syndrome) have a high risk of developing amblyopia. These risk factors are less likely to cause amblyopia if they occur closer to the age of 8-10 years. The older the child is when the risk factors occur, the lower the risk of developing amblyopia; if amblyopia does occur, it tends to be less severe.
Symptoms
Symptoms of amblyopia that can be observed include one eye that tends to move inward or outward or does not move in coordination with the other eye. Additionally, children may squint or even close one eye when looking at something, as they find it more comfortable to see with only one eye. This tendency can lead to children stumbling easily. Other symptoms include tilting the head to one side when looking at something. Screening tests for children can also show abnormal results.
Diagnosis
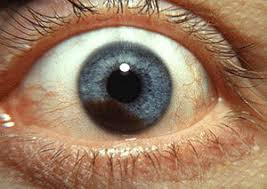
An eye specialist can diagnose amblyopia. The doctor typically performs a direct examination of the eyes, assessing the visual acuity of each eye separately and then together, the position of the eyeballs, eye movement, and the eye's reflex to light. Measuring visual acuity in both eyes is crucial because it can indicate amblyopia if one eye's visual acuity is much better. Moreover, visual acuity measurement is necessary to compare the vision in each eye. If there is a significant difference in acuity (anisometropia), the child is at high risk for amblyopia. The position of the eyeballs is examined to determine if the patient has strabismus. Eye movement is checked to see if both eyes move together in coordination. Light reflexes can be diminished in an eye with amblyopia.
Examinations will depend on the child's age. The test can utilize non-verbal children's ability to focus on moving objects. For verbal children, examinations can use pictures or letters, depending on whether they can read.
The doctor may also examine the inside of the eye using tools like a funduscope or slit lamp to look for cloudy eye fluid.
Typically, laboratory tests are not performed to diagnose amblyopia. However, brain imaging tests like MRI (magnetic resonance imaging) can be conducted to detect any brain abnormalities, especially if no eye abnormalities are found.
Management
The goal of amblyopia treatment is to address the underlying cause. If amblyopia is due to significant differences in visual acuity, the doctor may prescribe glasses to balance the visual acuity of the right and left eyes. If amblyopia is caused by strabismus, surgery may be performed to correct the position of the eyeball. However, strabismus can also be due to differences in visual acuity between the eyes, so glasses may be prescribed to correct the strabismus.
The doctor will also look for physical obstructions to vision, such as cataracts or tumors. If a baby has congenital cataracts, they should be corrected within the first two months of life.
Additionally, the doctor may encourage using the "lazy" eye through occlusion therapy. Occlusion therapy involves covering the "normal" eye to force the child to use the "lazy" eye. The normal eye can be covered with an eye patch or an opaque contact lens. The doctor may advise the child to cover one eye for several hours to a full day. If occlusion therapy is successful, the child can achieve equal visual acuity in both eyes. The patching will gradually reduce once visual acuity is stabilized between both eyes.
Besides occlusion therapy, the doctor can prescribe medications to reduce the work of the "normal" eye, thus forcing the use of the "lazy" eye. However, these medications can have side effects such as facial redness, increased heart rate, mood changes, and light sensitivity.
Amblyopia treatment is typically long-term and not resolved in one visit, so follow-up is necessary to monitor the child's progress after therapy. After amblyopia is treated, regular check-ups are required for several months due to the risk of recurrence.
Complications
Complications of amblyopia include irreversible vision loss in one eye. Therefore, amblyopia therapy should begin early. Other complications can arise from excessive amblyopia therapy, such as amblyopia or strabismus in the healthy eye. Using an eye patch can create unwanted social stigma, reducing compliance with the therapy. Eye patches can also irritate the skin and cause differences in skin color from the surrounding facial skin.
Prevention
Preventing amblyopia can be achieved through early childhood vision screening. Vision screening can be done from birth, before school (around age 3), and annually during elementary school. The goal is to monitor the child's visual development and manage conditions that can trigger amblyopia, such as significant differences in visual acuity between the eyes and strabismus.
Suppose a child has experienced an eye-related accident. In that case, you can examine the child to check for physical obstructions affecting vision, such as cataracts from trauma or bleeding inside the eye.
When to see a doctor?
If you have a baby (under 1 year old), observe whether one eye tends to move out of sync with the other. If this symptom is present, take the baby to the doctor for a vision examination. Eye examinations are also necessary if there is a family history of strabismus, childhood cataracts, or other childhood eye conditions.
Looking for more about other diseases? Click here!
- dr Ayu Munawaroh, MKK
- dr Hanifa Rahma
Bacal, D., Feldman, B., Miller, A., Plumb, R., Kozak, A., & Epley, K. (2021). Amblyopia - EyeWiki. Retrieved 29 October 2021, from https://eyewiki.aao.org/Amblyopia.
Lazy eye (amblyopia) - Symptoms and causes. (2021). Retrieved 29 October 2021, from https://www.mayoclinic.org/diseases-conditions/lazy-eye/symptoms-causes/syc-20352391.
Yen, K. (2018). Amblyopia: Practice Essentials, Background, Pathophysiology. Retrieved 29 October 2021, from https://emedicine.medscape.com/article/1214603-overview#showall.