Definisi
Dermatitis stasis merupakan sebuah kondisi ketika terdapat masalah pada pembuluh darah balik, terutama pembuluh darah balik pada tungkai. Masalah ini menyebabkan darah sulit mengalir dan menumpuk hingga terjadi kebocoran ke kulit. Kondisi ini disebut pula sebagai eksim venosa. Kondisi ini biasanya terjadi dalam jangka waktu panjang dan dapat ditangani.
Penyebab
Dermatitis stasis disebabkan oleh tekanan darah tinggi pada pembuluh darah balik. Tekanan darah tinggi tersebut disebabkan oleh aliran darah yang berlawanan arah dengan arah sebenarnya. Kesalahan aliran darah ini terjadi karena masalah pada penutupan katup pembuluh darah balik, kerusakan katup, atau sumbatan pada pembuluh darah balik. Selanjutnya, darah yang mengumpul mengandung ion besi yang memicu peradangan.
Faktor Risiko
Beberapa faktor dapat meningkatkan risiko dermatitis stasis, di antaranya:
- Tekanan darah tinggi
- Varises atau pembuluh darah balik yang tampak menonjol pada kulit
- Berat badan berlebih hingga obesitas
- Penyakit jantung seperti gagal jantung kongestif, yang menyebabkan penumpukan cairan di berbagai bagian tubuh
- Gagal ginjal
- Adanya pembekuan darah, terutama pada kaki
- Hamil lebih dari 2 kali
- Riwayat operasi atau cedera pada bagian tubuh tertentu
- Berdiri atau duduk dalam jangka waktu lama
- Kurang berolahraga
Gejala
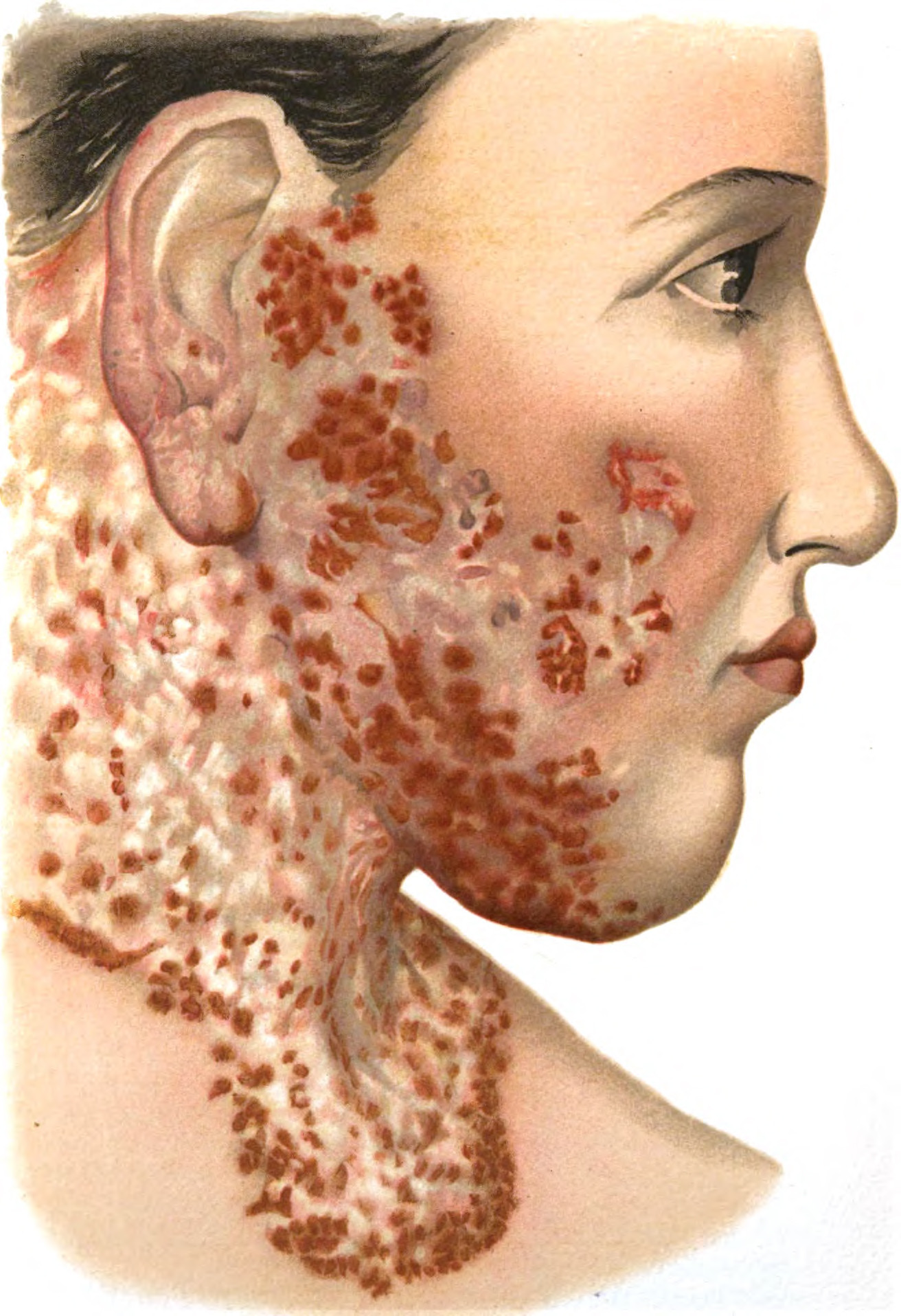
Seperti dermatitis atau peradangan kulit lainnya, dermatitis stasis membuat kulit menjadi gatal, bengkak, kering, bersisik, dan mengelupas. Pada kulit berwarna terang, dermatitis stasis tampak merah atau coklat. Sementara itu, pada kulit berwarna gelap, dermatitis stasis tampak berwarna ungu atau abu-abu, sehingga cukup sulit untuk dilihat.
Dermatitis stasis biasanya merupakan penyakit jangka panjang. Ada periode ketika gejala membaik, namun ada pula periode ketika gejala memburuk. Kaki Anda dapat terlihat bengkak, terutama pada malam hari atau setelah berdiri lama. Varises juga dapat terlihat pada kulit.
Gejala lainnya dapat berupa:
- Perubahan warna pada kulit yang terkena
- Perubahan tekstur kulit menjadi keras (lipodermatosklerosis)
- Bekas luka berwarna putih, berukuran kecil (atrophie blanche)
- Nyeri
- Eksim yang mempengaruhi bagian tubuh lainnya
Diagnosis
Diagnosis dermatitis stasis ditegakkan berdasarkan riwayat dan hasil pemeriksaan. Dokter mungkin akan menanyakan kepada Anda apabila ada kondisi kesehatan seperti:
- Varises, pembesaran pembuluh darah balik di kaki yang tampak berkelok-kelok
- Trombosis vena dalam, penyumbatan pembuluh darah balik oleh bekuan darah
- Luka di kaki yang tidak kunjung sembuh
- Selulitis, infeksi jaringan ikat di bawah kulit
- Adanya riwayat operasi atau cedera pada kaki
Dokter juga dapat memeriksa ABI (ankle brachial index) dengan mengukur tekanan darah pada kedua tangan dan kedua kaki. Pemeriksaan ini dilakukan untuk mengetahui adanya masalah pada pembuluh darah nadi pada kaki, serta memastikan Anda dapat menggunakan stocking untuk terapi. Jika tekanan darah pada kaki berbeda jauh dengan tangan, Anda tidak dapat menggunakan stocking untuk membantu mengatasi dermatitis stasis.
Jika Anda memiliki riwayat trombosis vena, dokter akan melakukan pemeriksaan darah untuk mencari bila darah Anda terlalu mudah mengental sehingga mempermudah terjadinya sumbatan.
Anda dapat pula dirujuk ke dokter spesialis bedah, bedah toraks dan kardiovaskuler, bedah vaskuler, atau dokter kulit (tergantung ketersediaan dokter) untuk pemeriksaan lebih lanjut, atau apabila Anda mengalami varises, pengerasan kulit, tukak pada kaki. Anda juga dapat dirujuk apabila hasil pemeriksaan ABI menunjukkan perbedaan yang cukup jauh antara tekanan darah pada kaki dan tangan, atau apabila kondisi Anda tidak membaik dengan terapi yang sudah dilakukan.
Tata Laksana
Dermatitis stasis terjadi karena adanya sumbatan pada pembuluh darah, sehingga dokter dapat menyarankan operasi untuk memperbaiki pembuluh darah Anda. Beberapa cara lainnya dapat dilakukan untuk meningkatkan aliran darah balik ke jantung, yaitu:
- Gunakan stocking untuk membantu memperlancar aliran darah serta mengecilkan pembengkakan
- Jaga agar kaki tetap berada di atas jantung. Anda dapat melakukannya dengan berbaring, kemudian kaki ditaruh di atas bantal yang ditumpuk. Jika memungkinkan, Anda dapat melakukannya selama 15 menit setiap 2 jam sekali dan ketika tidur
- Jangan berdiri terlalu lama
Untuk mengatasi nyeri, merah, atau bengkak, dokter dapat memberikan Anda obat antiradang atau obat-obatan lainnya yang dapat dioleskan pada kaki Anda. Anda juga mungkin mendapatkan obat antigatal untuk mengatasi gatal.
Anda juga kemungkinan perlu menutup daerah yang terkena dengan penutup khusus. Jika terjadi infeksi pada daerah tersebut, dokter dapat memberikan antibiotik, baik antibiotik minum ataupun suntik. Anda juga dapat mengoleskan pelembab agar kulit tetap lembab dan menjaga agar area yang terkena tetap lembut. Pelembab yang disarankan adalah pelembab tanpa aroma, cat, atau parfum, sehingga tidak menyebabkan iritasi pada kulit, contohnya petroleum jelly dan krim tebal.
Dermatitis stasis pada umumnya terjadi dalam jangka waktu panjang, sehingga terapinya pun juga membutuhkan waktu panjang. Oleh karena itu, komitmen sangat diperlukan untuk membantu terapi dermatitis stasis. Jika Anda merasa terganggu dengan perubahan warna kulit, Anda dapat memakai bedak untuk menutupinya.
Komplikasi
Komplikasi dermatitis stasis dapat berupa selulitis (infeksi jaringan ikat di bawah kulit) dan luka yang tidak kunjung sembuh. Akibat langsung dari dermatitis stasis adalah peningkatan risiko dermatitis kontak alergi (peradangan kulit yang disebabkan oleh kontak dengan benda-benda yang memicu alergi), pengerasan kulit, dan terjadinya eksim serupa pada kaki yang tadinya sehat.
Pencegahan
Beberapa hal dapat dilakukan untuk mencegah dermatitis stasis terjadi atau mencegah dermatitis stasis berkembang, yaitu:
1. Beristirahat
Jika pekerjaan Anda mengharuskan Anda untuk berdiri atau duduk terlalu lama, sediakan waktu untuk bergerak. Berjalan kakilah selama 10 menit untuk setiap jam.
2. Berolahraga
Pergerakan tubuh memperlancar aliran darah. Anda dapat berkonsultasi kepada dokter terkait berapa lama Anda sebaiknya berolahraga dan apa saja olahraga yang aman untuk Anda.
3. Menggunakan Pakaian yang Nyaman
Stocking kompresi adalah pilihan yang baik untuk kaki Anda, namun Anda sebaiknya memilih pakaian yang lebih longgar untuk bagian tubuh Anda yang lainnya. Kain yang ketat atau kasar dapat mengiritasi kulit dan mempengaruhi aliran darah.
4. Menjaga Kulit Anda
Kulit sangat mudah mengalami iritasi. Sebaiknya Anda menggunakan pembersih dan handuk yang lembut saat mandi, diikuti dengan pelembab kulit bebas parfum. Anda sebaiknya menghindari penggunaan produk pembersih, parfum, rumput, tanaman, rambut hewan, serta hal lainnya yang dapat merusak kulit Anda.
Kapan Harus ke Dokter?
Jika Anda merasakan adanya nyeri pada kaki disertai bengkak, sebaiknya Anda segera ke dokter. Apabila Anda mengalami hal tersebut didahului dengan riwayat trombosis vena, varises, hingga selulitis, Anda dapat mencari pengobatan ke dokter. Dermatitis stasis biasanya terjadi dalam jangka waktu panjang, sehingga apabila nyeri dan bengkak tersebut bersifat akut atau baru saja terjadi, hal ini dapat menunjukkan adanya trombosis vena, yang merupakan sebuah kegawatdaruratan medis. Trombosis vena yang tidak segera ditangani dapat menyebabkan sumbatan pembuluh darah di paru-paru yang dapat menyebabkan kematian.
Mau tahu informasi seputar penyakit lainnya, cek di sini ya!
- dr Hanifa Rahma
DiLonardo, M., & Ratini, M. (2022). What Is Venous Stasis Dermatitis?. Retrieved 28 March 2022, from https://www.webmd.com/skin-problems-and-treatments/eczema/venous-stasis-dermatitis
Flugman, S. (2020). Stasis Dermatitis: Background, Etiology, Epidemiology. Retrieved 28 March 2022, from https://emedicine.medscape.com/article/1084813-overview
Varicose eczema. (2019). Retrieved 28 March 2022, from https://www.nhs.uk/conditions/varicose-eczema/