Definisi
Epidermolisis bulosa merupakan suatu kelompok penyakit langka yang menyebabkan kulit mudah terluka. Pada kelompok penyakit ini, kulit mudah terluka sebagai respon dari cedera ringan, misalnya yang diakibatkan oleh panas, menggaruk dan menggosok kulit, atau plester. Sebagian besar epidermolisis bulosa diwariskan dari orang tua. Biasanya, kondisi ini muncul pada usia bayi atau anak. Namun, ada pula orang yang baru mengalami gejala pada usia remaja atau dewasa muda.
Penyebab
Epidermolisis bulosa pada umumnya merupakan penyakit yang diturunkan dari orang tua ke anaknya. Gen yang membawa penyakit ini dapat diwariskan dari salah satu orang tua yang menderita penyakit ini (disebut sebagai pewarisan autosomal dominan), dari kedua orang tua yang sama-sama memiliki gen pembawa penyakit namun belum tentu memiliki gejala (disebut sebagai pewarisan autosomal resesif), atau sebagai akibat dari mutasi genetik yang dapat diwariskan. Mutasi genetik merupakan perubahan struktur dari gen yang dapat terjadi akibat berbagai faktor. Perubahan struktur gen ini dapat menyebabkan masalah pada bagian tubuh tertentu, seperti kulit.
Kulit sendiri terdiri atas lapisan luar (epidermis) dan dalam (dermis). Pertemuan antara kedua lapisan ini disebut sebagai membran basal. Jenis epidermolisis bulosa biasanya ditentukan dari asal terbentuknya lenting.
Jenis-jenis epidermolisis bulosa adalah sebagai berikut:
- Epidermolisis bulosa simpleks. Jenis ini merupakan jenis yang paling sering terjadi. Pada jenis ini, luka sering terjadi pada epidermis dan biasanya terjadi pada tangan dan kaki. Luka ini biasanya dapat sembuh tanpa bekas
- Epidermolisis bulosa junctional. Jenis ini dapat terjadi parah, dan gejalanya dimulai pada saat bayi. Bayi dengan kondisi ini dapat memiliki suara tangisan serak akibat luka yang terjadi terus-menerus pada pita suara dan meninggalkan bekas luka
- Epidermolisis bulosa distrofik. Jenis ini terjadi akibat masalah pada gen yang menghasilkan kolagen, zat yang memberikan kekuatan pada dermis. Jika kolagen berkurang atau tidak terbentuk sama sekali, epidermis dan dermis tidak dapat menyatu dengan baik
Faktor Risiko
Faktor risiko epidermolisis bulosa adalah memiliki riwayat keluarga, baik orang tua, kakek-nenek, atau saudara yang memiliki penyakit serupa.
Gejala
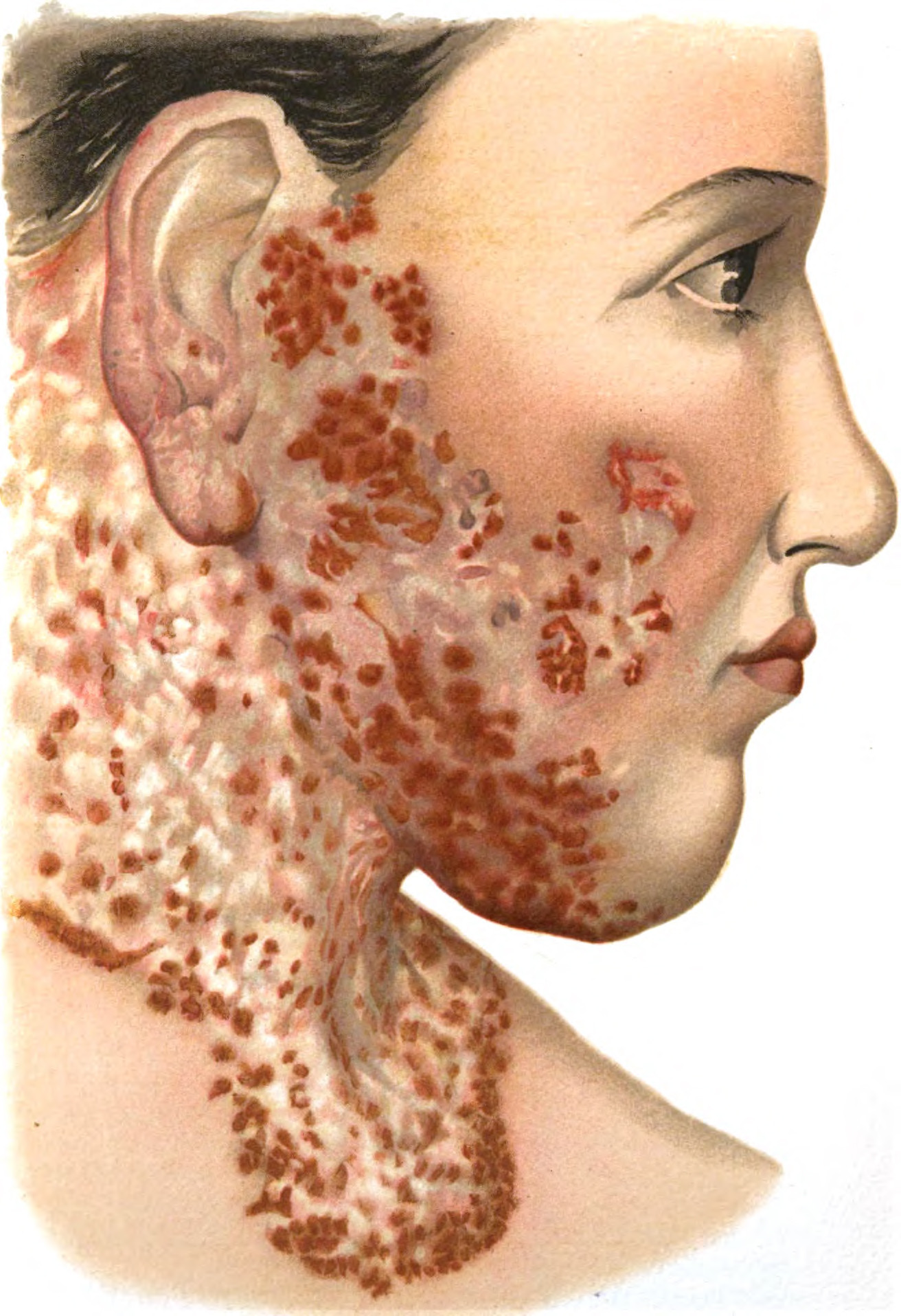
Gejala epidermolisis bulosa dapat bermacam-macam, tergantung jenisnya. Terlepas dari waktu mulainya, Anda dapat menyadari adanya lenting yang mudah pecah hingga menyebabkan luka.
Semua orang dengan epidermolisis bulosa memiliki kulit yang lemah. Kadang-kadang, kulit ini terlalu lemah sehingga sentuhan lembut atau perubahan suhu secara tiba-tiba saja dapat menyebabkan lenting yang nyeri dalam beberapa menit. Lenting ini dapat pecah dan meninggalkan luka yang nyeri. Selain itu, kulit yang lemah juga menyebabkan luka tersebut lambat sembuh. Beberapa luka dapat sembuh hingga berbulan-bulan atau bertahun-tahun. Luka yang parah bahkan mungkin tidak akan pernah sembuh.
Selain pada kulit, luka dapat terjadi pada jaringan yang melapisi bagian dalam mulut, mata, kerongkongan, usus, saluran kencing, atau bagian tubuh lainnya. Luka ini dapat terjadi dalam derajat ringan hingga mengancam nyawa.
Selain lenting yang mudah pecah, penyakit ini juga dicirikan dengan adanya nyeri. Nyeri ini terutama dirasakan oleh orang-orang dengan epidermolisis bulosa yang parah. Penyebab nyeri dapat berupa luka atau sentuhan pada kulit. Infeksi, mandi, penggantian perban, dan kulit kering juga dapat menyebabkan nyeri.
Apabila lenting dan luka terbentuk pada jaringan yang melapisi bagian dalam mulut, mata, dan bagian dalam tubuh lainnya, nyeri ini seringkali luar biasa.
Diagnosis
Diagnosis epidermolisis bulosa biasanya ditegakkan pada usia bayi atau anak-anak, karena biasanya gejalanya sudah terlihat sejak usia bayi. Namun, beberapa tipe epidermolisis bulosa yang lebih ringan mungkin tidak dapat terdiagnosis hingga dewasa. Jika dokter menduga adanya kondisi ini pada seseorang, dokter dapat merujuk orang tersebut kepada dokter spesialis kulit. Dokter spesialis kulit dapat melakukan pemeriksaan lanjutan untuk menentukan tipe epidermolisis bulosa serta rencana tata laksana. Untuk menentukan tipe penyakit ini, dokter dapat mengambil sampel kecil jaringan kulit (biopsi) yang akan diamati di bawah mikroskop.
Pada beberapa kasus lainnya, Anda dapat mencari tahu adanya penyakit ini pada janin yang masih di dalam kandungan. Deteksi ini dapat dilakukan mulai dari minggu ke-11 kehamilan. Pemeriksaan ini dapat dilakukan dengan mengambil cairan ketuban (amniosentesis) atau pengambilan jaringan dari ari-ari (chorionic villus sampling). Namun, pemeriksaan-pemeriksaan ini biasanya dilakukan jika Anda atau pasangan Anda telah diketahui membawa gen dari penyakit ini, dan memiliki risiko melahirkan bayi dengan epidermolisis bulosa yang parah. Jika hasil pemeriksaan ini positif, dokter dapat memberikan saran dan konseling.
Tata Laksana
Epidermolisis bulosa merupakan kondisi yang tidak dapat disembuhkan karena diwariskan. Beberapa tenaga kesehatan yang dapat membantu Anda menangani kondisi ini adalah dokter anak, dokter kulit, dokter spesialis kulit konsultan anak, perawat, ahli gizi, serta psikolog dan psikiater. Tenaga kesehatan ini dapat membantu Anda untuk mengatasi berbagai masalah yang terjadi akibat epidermolisis bulosa.
Penanganan yang dibutuhkan oleh penderita epidermolisis bulosa biasanya berupa:
- Perawatan luka. Perawatan luka dapat dilakukan hingga satu jam atau lebih setiap harinya. Sebagian besar pasien harus menggunakan perban yang harus diganti setiap hari atau beberapa hari sekali. Jika gejala cukup parah, penderita mungkin akan membutuhkan bantuan perawat untuk merawat luka
- Penanganan nyeri. Epidermolisis bulosa dapat menyebabkan nyeri yang luar biasa yang dapat disebabkan oleh berbagai hal seperti luka, kulit kering, infeksi, menelan makanan, makan, kencing, pergerakan usus, atau bahkan bergerak biasa. Untuk mengatasi nyeri, penderita seringkali membutuhkan obat-obatan. Obat-obatan ini dapat berupa antidepresan, obat-obatan yang biasa digunakan untuk menangani epilepsi (kejang berulang), dan parasetamol. Jika nyeri luar biasa, obat-obatan seperti fentanil, morfin, atau ketamin juga dapat diresepkan
- Pencegahan luka. Pencegahan luka dapat dilakukan dengan penggunaan perban dengan alas serta menggunakan baju yang longgar. Dokter spesialis kulit dapat memberikan Anda saran lebih lanjut untuk mencegah luka
- Penanganan komplikasi. Lenting dan luka dapat menyebabkan masalah lainnya pada tubuh, sehingga penanganan akan dibutuhkan untuk masalah-masalah tersebut
Komplikasi
Komplikasi epidermolisis bulosa dapat berupa:
- Infeksi. Kulit yang luka lebih rentan terhadap infeksi
- Sepsis. Sepsis terjadi ketika bakteri yang menyebabkan infeksi berat masuk ke dalam aliran darah dan menyebar ke seluruh tubuh. Sepsis biasanya terjadi secara cepat dan mengancam nyawa, serta menyebabkan syok (kekurangan oksigen pada berbagai organ tubuh) dan gagal organ
- Perubahan pada jari dan sendi. Epidermolisis bulosa yang parah dapat menyebabkan jari-jari menggabung menjadi satu atau menyebabkan sendi bengkok secara tidak normal (kontraktur). Hal ini dapat menyebabkan masalah pada pergerakan jari, siku, dan lutut
- Masalah nutrisi. Luka yang terjadi di dalam mulut dapat mempersulit makan sehingga menyebabkan gizi buruk, anemia (kurangnya sel darah merah, misalnya akibat kekurangan zat besi), penyembuhan luka semakin lama dan masalah pertumbuhan
- Sembelit. Kesulitan BAB juga dapat terjadi akibat adanya luka pada daerah lubang bokong (anus). Hal ini juga dapat disebabkan oleh kurangnya konsumsi cairan atau makanan tinggi serat, seperti buah-buahan dan sayur-sayuran
- Masalah gigi seperti gigi keropos
- Kanker kulit. Orang remaja dan dewasa dengan penyakit ini memiliki risiko tinggi untuk mengalami kanker kulit berupa karsinoma sel skuamosa
- Kematian. Bayi dengan epidermolisis bulosa yang parah memiliki risiko tinggi infeksi dan kehilangan cairan tubuh akibat luka yang terjadi pada berbagai bagian tubuh, serta kesulitan makan dan bernapas. Bayi-bayi dengan jenis epidermolisis bulosa ini biasanya meninggal pada usia muda
Pencegahan
Epidermolisis bulosa tidak dapat dicegah karena sifatnya yang diwariskan. Namun, Anda dapat melakukan beberapa hal untuk mencegah luka dan infeksi, yaitu:
- Merawat anak Anda dengan lembut. Bayi atau anak Anda butuh dipeluk, namun secara lembut. Untuk menggendong anak Anda, Anda dapat menaruhnya pada kain yang halus (misalnya terbuat dari kapas), dan mengangkatnya pada bagian bokong dan belakang leher. Anda sangat tidak disarankan untuk mengangkat anak Anda dari bagian bawah lengan
- Memberikan perhatian khusus pada area popok. Jika anak Anda menggunakan popok, Anda perlu membuang karet dan menghindari cairan untuk mengelap bagian tersebut. Anda juga dapat melapisi popok dengan alas yang tidak melekat pada kulit
- Menjaga suhu rumah agar tetap sejuk dan konsisten
- Menjaga kelembapan kulit misalnya dengan gel petroleum
- Memakaikan baju yang lembut untuk anak Anda. Anda dapat memakaikan baju yang lembut dan mudah dilepas pada anak Anda. Selain itu, Anda dapat menggunting label dan memakai baju secara terbalik (bagian dengan jahitan di luar) untuk mencegah terjadinya luka. Anda juga dapat menjahitkan alas pada bagian siku, lutut, dan bagian tubuh yang sering tertekan lainnya
- Menjaga anak agar tetap aktif. Anda dapat mengajak anak untuk melakukan aktivitas yang tidak menyebabkan luka pada kulit, misalnya berenang. Pada anak dengan epidermolisis bulosa ringan, perlindungan kulit dapat dilakukan dengan menggunakan baju lengan panjang untuk kegiatan di luar ruangan
- Melapisi permukaan yang kasar. Anda dapat melakukannya dengan melapisi jok mobil dengan kain lembut atau bak mandi berendam dengan handuk tebal
Kapan harus ke dokter?
Segeralah ke dokter apabila anak Anda sering mengalami luka yang tidak diketahui penyebabnya. Pada bayi, luka yang parah dapat mengancam nyawa. Anda disarankan untuk langsung ke IGD apabila anak Anda kesulitan menelan, bernapas, atau menunjukkan tanda-tanda infeksi seperti kulit yang hangat, merah, nyeri, bengkak, atau bau tidak sedap dari luka, serta demam.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Nadia Opmalina
Epidermolysis bullosa - Symptoms and causes. Mayo Clinic. (2020). Retrieved 6 June 2022, from https://www.mayoclinic.org/diseases-conditions/epidermolysis-bullosa/symptoms-causes/syc-20361062.
Epidermolysis bullosa. nhs.uk. (2021). Retrieved 6 June 2022, from https://www.nhs.uk/conditions/epidermolysis-bullosa/.
Epidermolysis bullosa: Overview. Aad.org. Retrieved 6 June 2022, from https://www.aad.org/public/diseases/a-z/epidermolysis-bullosa-overview.