Definition
Necrotizing enterocolitis (NEC) is a severe condition characterized by rapid damage and death of intestinal tissue, commonly occurring in preterm babies. In severe cases, NEC can lead to the formation of a hole in the intestinal wall, allowing normal bacteria from the intestine to enter the abdominal cavity, causing a widespread infection. This condition is a medical emergency and can be fatal if not promptly and adequately treated.
NEC can manifest in newborn babies during the first two weeks of life, but it is more common in preterm infants. Approximately 90% of NEC cases occur in preterm babies. In normal (non-preterm) babies, the incidence of NEC is 1 in 10,000.
Causes
The cause of NEC is not fully understood, but it is believed that factors such as a shortage of oxygen during difficult labor may contribute to the risk. The intestinal tissue becomes weaker when there is a shortage of oxygen and a lack of blood flow to the intestine. This weakened condition makes it easier for bacteria to grow, leading to damage to the intestinal tissue. The spread of infection and tissue damage is what causes NEC.
NEC is classified based on the time of onset and the cause. These types of NEC include:
- Classic: This is the most commonly found type, affecting preterm babies born before 28 weeks. Classic NEC typically occurs 3–6 weeks after birth. The baby is often relatively stable, and symptoms suddenly appear.
- Associated with Transfusion: Babies who require blood transfusions to address anemia may develop NEC. Approximately 1 in 3 preterm babies develop NEC after receiving blood.
- Atypical: This type is rare and occurs in the first week of life or before the baby has started feeding
- Full-term Baby: NEC in full-term babies is uncommon and is often associated with other congenital disorders such as congenital heart disease, gastroschisis (intestines outside the abdomen), or low oxygen levels at birth
Risk Factor
NEC is considered a rare disease, with an incidence of 1 in 2000–4000 births. This condition can occur in newborns and is more commonly found in preterm babies with a birth weight of less than 1500 grams. Other risk factors for NEC include:
- Preterm birth: Babies born prematurely have a higher risk due to a lower immune system, leading to digestion problems, increased susceptibility to infections, and suboptimal blood and oxygen circulation
- Oral intake of formula milk or feeding through a straw by preterm or high-risk babies
- Labor with complications or low oxygen levels
- Babies with elevated levels of red blood cells
- Babies with infections in the digestive system
- Severely ill babies receiving blood transfusions
Symptoms
The symptoms of NEC include:
- Bloated and swollen abdomen
- Changes in the color of the abdomen
- Bloody stool
- Diarrhea
- Green or yellowish vomit
- Loss of appetite or a desire to breastfeed, accompanied by weight loss
Babies with NEC may also exhibit signs of infection, including:
- Fever
- Weakness
- Respiratory distress
Diagnosis
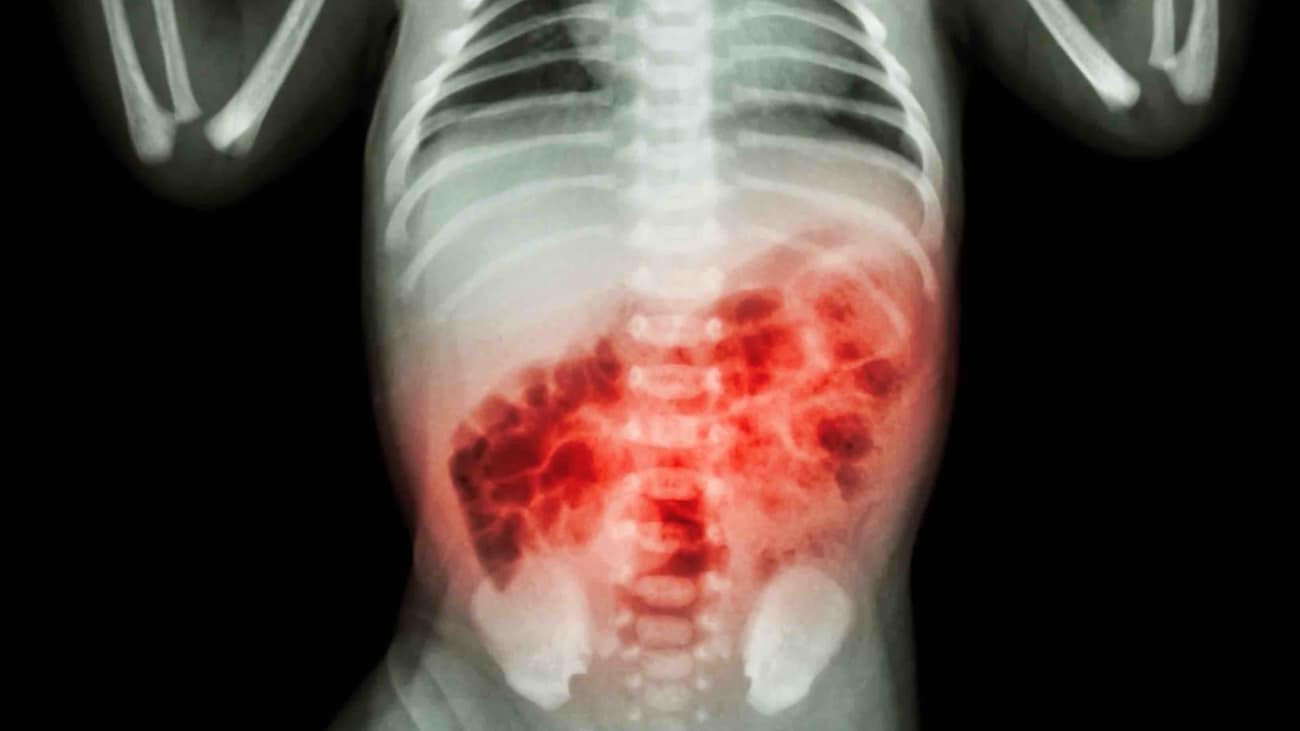
A doctor can diagnose NEC by conducting a physical examination and some additional tests. During the physical exam, the doctor will check the baby's abdomen to assess for signs of swelling and tenderness.
To support the diagnosis, the doctor may recommend abdominal X-ray imaging. This test provides a visual representation of the intestine, aiding the doctor in identifying signs of inflammation and tissue damage more easily.
Additionally, the baby's feces can be checked for the presence of blood. The doctor may also recommend blood tests to assess the levels of platelets and white blood cells. Platelets play a role in blood clotting, while white blood cells fight infections. Low platelet or white blood cell levels can be indicators of NEC.
Furthermore, the doctor may also assess the possibility of intestinal perforation. This examination involves inserting a needle into the abdominal space to check for the presence of intestinal fluid. The presence of such fluid is a sign of intestinal perforation.
Management
There are various methods to manage NEC, and the management plan is tailored based on factors such as:
- The severity of the disease
- The baby's age
- The overall health of the baby
In many cases, doctors may advise parents to discontinue breastfeeding. The baby will receive fluids and nutrition intravenously. Antibiotics are administered to help fight the infection. If the baby experiences difficulty breathing or abdominal swelling, the doctor may provide additional oxygen or assistance with breathing.
Surgery is required for severe cases of NEC, involving the removal of the damaged intestine. Throughout the treatment, the baby will be closely observed. The medical staff will periodically use imaging and blood tests to monitor the progression of the disease.
Approximately 8 out of 10 babies with NEC show improvement after treatment. However, the remaining 2 may experience long-term health problems.
Complications
Some complications of the NEC include:
- Abdominal infection: The damage to intestinal tissue can lead to the formation of holes or perforations in the intestinal wall. Perforations allow bacteria to enter the abdominal cavity, causing peritonitis. Peritonitis increases the risk of infection spreading through the blood, leading to life-threatening sepsis.
- Stricture or narrowing of the intestine: About 1 in 3 babies with NEC may develop intestinal stricture. This condition typically occurs a few months after healing from NEC, making digestion more challenging. Some children may require surgery to address this issue.
- Short-intestine syndrome: NEC-induced damage to a part of the small intestine can result in short-intestine syndrome. This condition hinders the body's ability to absorb fluids and nutrition, leading to malabsorption. Children with this syndrome require lifelong care to ensure proper nutrition, and some may need to be fed through a tube.
- Growth failure and developmental delay: Long-term complications include growth failure, impaired neurological growth, and developmental delays, especially in babies who have undergone surgery. These children need ongoing follow-up to monitor their growth and development.
- Liver problems: inability to tolerate feeding through a tube, necessitating intravenous feeding.
Prevention
If parents are at risk of preterm labor, they may receive corticosteroid injections to reduce the chances of the baby developing intestinal and lung problems.
Providing breast milk to the baby also reduces the likelihood of NEC. Some studies suggest that adding probiotics to breast milk or formula milk can further contribute to prevention.
When to see a doctor?
Consult a pediatrician or doctor if your baby exhibits any signs of the NEC mentioned above. Prompt management is crucial to avoid complications, especially growth and developmental problems.
- dr Nadia Opmalina
Holm G. (2021). Necrotizing enterocolitis. Retrieved 24 January 2022, from https://www.healthline.com/health/necrotizing-enterocolitis
What is necrotizing enterocolitis?. (2020). Retrieved 24 January 2022, from https://www.webmd.com/parenting/baby/what-is-necrotizing-enterocolitis#091e9c5e81507091-1-3
Necrotizing enterocolitis (NEC). (2021). Retrieved 24 January 2022, from http://https//my.clevelandclinic.org/health/diseases/10026-necrotizing-enterocolitis#prevention
Schwartz CI. (2021). Necrotizing enterocolitis. Retrieved 24 January 2022, from https://medlineplus.gov/ency/article/001148.htm