Definisi
Karsinoma pankreas adalah kanker yang berasa dari sel-sel pankreas. Pankreas sendiri merupakan organ pencernaan yang berfungsi untuk menghasilkan enzim-enzim pencernaan dan untuk mengatur gula darah. Organ pankreas terdiri atas kepala, badan, dan ekor. Enzim-enzim ini kemudian melewati saluran yang berada di dalam pankreas dan menyambung keluar, bergabung dengan saluran empedu. Setelah melewati saluran-saluran tersebut, enzim sampai di tujuannya yaitu usus 12 jari. Karsinoma pankreas merupakan salah satu kanker yang sering menyebabkan kematian.
Penyebab
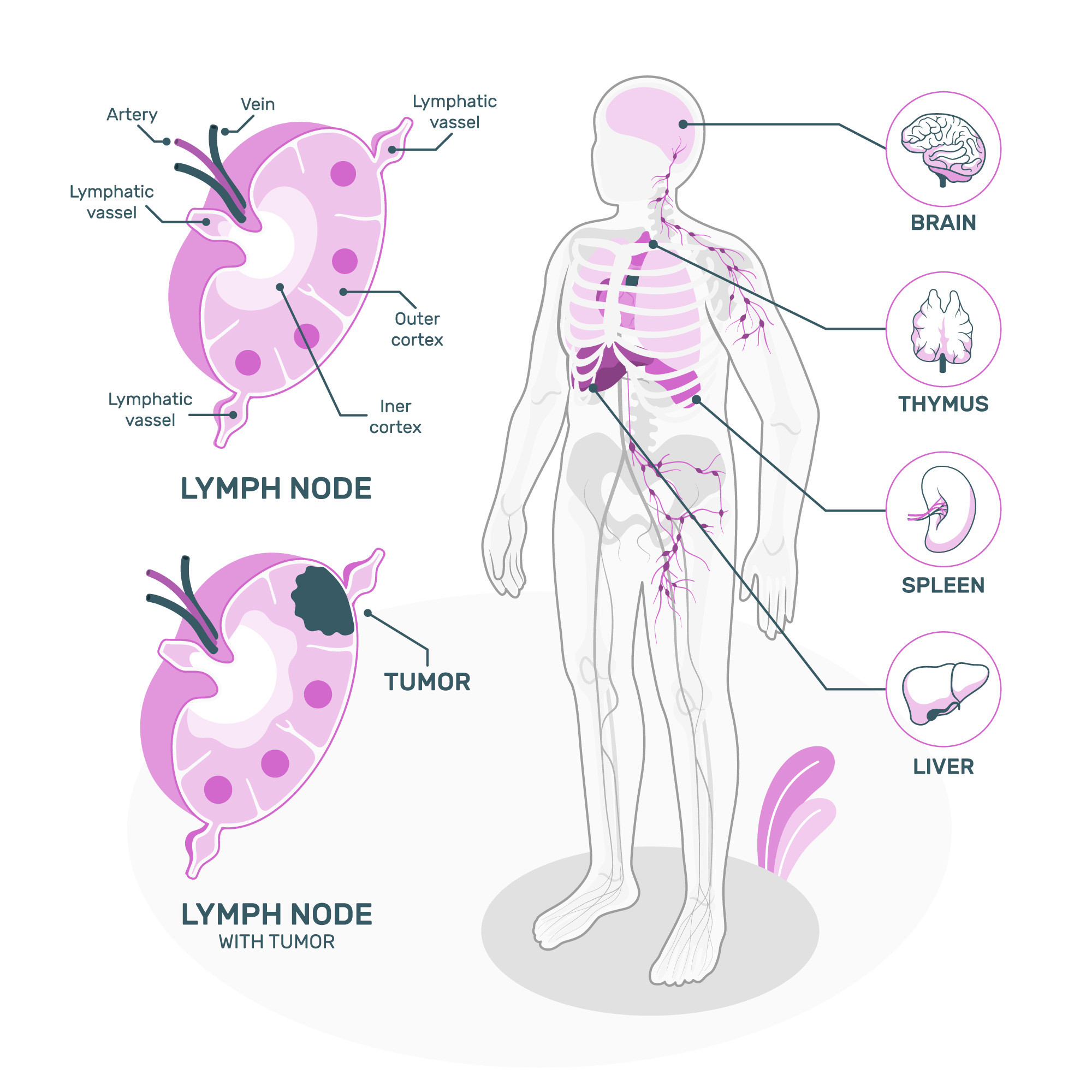
Karsinoma pankreas terjadi akibat berbagai faktor. Faktor-faktor ini membuat sel-sel pankreas mengalami mutasi atau perubahan susunan genetik. Gen berfungsi untuk memberikan instruksi kerja sel-sel tubuh, namun pada sel-sel yang mengalami kanker, gen-gen ini memberikan instruksi kepada sel untuk membelah diri secara cepat dan tidak terkontrol, serta untuk tetap hidup bahkan setelah sel-sel normal mati. Sel yang telah bermutasi tersebut lalu berkumpul dan membentuk tumor. Jika tidak segera ditangani, sel-sel ini dapat menyebar ke organ-organ lainnya melalui kontak langsung atau masuk ke aliran darah dan limfe.
Karsinoma pankreas dapat terjadi pada dua jenis sel yaitu:
- Sel pada saluran pankreas yang berfungsi mengeluarkan enzim ke usus halus (adenokarsinoma), terdiri dari 93% karsinoma pankreas
- Sel pankreas yang menghasilkan hormon insulin, hormon yang berfungsi untuk mengatur gula darah, disebut sebagai tumor neuroendokrin pankreas
Faktor Risiko
Merokok
Faktor risiko tersering kanker pankreas adalah merokok. Sekitar 30% kasus karsinoma pankreas dipengaruhi oleh rokok. Seorang perokok memiliki risiko dua kali lipat lebih besar untuk mengalami karsinoma pankreas dibandingkan nonperokok. Sementara itu, orang-orang yang telah merokok selama lebih dari 40 tahun memiliki risiko karsinoma hingga lima kali lipat lebih besar.
Obesitas
Selain itu, faktor risiko lainnya adalah obesitas, baik yang terjadi pada masa kecil, dewasa muda, atau lanjut usia. Konsumsi daging merah berkaitan dengan kenaikan risiko kanker pankreas, namun unggas dan produk susu tidak memberikan efek serupa. Orang-orang yang rajin mengonsumsi sayuran dan buah-buahan, terutama yang mengandung folat, memiliki risiko lebih rendah.
Diabetes melitus
Faktor risiko lainnya adalah penyakit diabetes melitus. Penyakit ini berkaitan dengan produksi insulin pada pankreas. Penderita diabetes melitus selama minimal 5 tahun memiliki risiko dua kali lipat lebih besar untuk mengalami kondisi ini.
Pankreatitis kronik
Selain itu, faktor risiko lainnya dapat pula berupa pankreatitis atau peradangan pankreas kronik. Semakin lama penyakit ini terjadi, semakin meningkat pula risiko karsinoma pankreas.
Faktor Genetik
Faktor risiko lainnya adalah genetik, yang menyusun 5-10% kasus kanker pankreas. Faktor risiko genetik ini dapat menyebabkan seseorang menderita pankreatitis kronik terlebih dahulu atau langsung menyebabkan karsinoma pankreas.
Gejala
Tanda dan gejala karsinoma pankreas biasanya tidak akan muncul hingga stadium lanjut. Gejala penyakit ini dapat berupa:
- Nyeri perut yang menjalar ke punggung
- Kehilangan nafsu makan
- Penurunan berat badan drastis yang tidak diinginkan
- Kulit dan bola mata menjadi kuning
- BAB berwarna dempul
- Urine berwarna seperti teh
- Kulit mudah gatal
- Adanya diagnosis penyakit diabetes baru atau diabetes yang makin sulit terkontrol
- Gangguan pembekuan darah seperti munculnya lebam pada kulit atau titik-titik perdarahan
- Mudah lelah
Diagnosis
Diagnosis karsinoma pankreas dapat dilakukan setelah Anda menjalani berbagai pemeriksaan. Dokter akan menanyakan riwayat merokok, konsumsi alkohol, serta adanya anggota keluarga yang mengalami gejala serupa sebelumnya. Pemeriksaan dapat dilakukan secara langsung untuk meraba adanya massa di perut, baik dari sel-sel pankreas, atau penyebarannya ke hati dan ke dekat usus, serta pembesaran limpa akibat penekanan pembuluh darah oleh massa tumor.
Selain itu, pemeriksaan yang dapat dilakukan dapat berupa pemeriksaan laboratorium. Pemeriksaan laboratorium tidak dapat sepenuhnya membantu diagnosis karsinoma pankreas, namun dapat membantu dugaan diagnosis. Pemeriksaan laboratorium yang dapat dilakukan berupa pemeriksaan darah, bilirubin, enzim pankreas, dan enzim hati. Selain itu, pemeriksaan penanda tumor dapat pula dilakukan.
Pemeriksaan yang dapat membantu mengarahkan diagnosis karsinoma pankreas adalah pencitraan. Pencitraan yang dapat dilakukan berupa computed tomography scan (CT scan) yang relatif murah, cepat, dan akurat. Namun, jika fasilitas tidak terlalu memadai, ultrasonografi (USG) dapat dilakukan. Sayangnya, pada pemeriksaan ini, pankreas seringkali tertutup oleh udara dari lambung, usus halus, dan usus besar. Apabila fasilitas memadai, pemeriksaan USG lewat endoskopi (memasukkan selang lewat mulut) juga dapat dilakukan. Dengan alat ini, pengambilan jaringan pankreas dapat langsung dilakukan dengan jarum halus untuk menentukan jenis karsinoma. Endoskopi saja juga dapat dilakukan, berupa endoscopic retrograde cholangiopancreatography (ERCP). Pemeriksaan menggunakan magnetic resonance imaging (MRI) juga dapat dilakukan untuk membantu diagnosis.
Pemeriksaan baku emas untuk diagnosis karsinoma pankreas adalah pemeriksaan jaringan pankreas. Seperti telah dijelaskan sebelumnya, sel dapat diambil dengan bantuan endoskopi. Namun, apabila fasilitas kurang memadai, pengambilan jaringan dengan jarum halus dapat dilakukan dengan bantuan CT.
Tatalaksana
Tata laksana karsinoma sangat tergantung pada keparahan dan keadaan penderita. Pembedahan dapat dilakukan pada karsinoma stadium awal. Pembedahan tersebut dapat berupa prosedur Whipple, yang berfungsi untuk mengangkat jaringan tumor di kepala pankreas dan sebagian usus dua belas jari. Apabila karsinoma terjadi di badan atau ekor pankreas, pengangkatan dilakukan pada bagian ujung dan dapat melibatkan pengangkatan limpa. Selain itu, apabila ada pembuluh darah besar terlibat di dalam kanker, pembedahan dapat dilakukan untuk merekonstruksi atau membentuk ulang pembuluh darah, misalnya menggunakan cangkok jaringan.
Apabila karsinoma sudah mencapai stadium lanjut, pembedahan tidak akan menjadi pilihan terapi. Pada kondisi seperti ini, pilihan terapi biasanya melibatkan obat-obatan (kemoterapi) dan/atau terapi radiasi.
Tata laksana karsinoma pankreas, sama dengan kanker lainnya, juga melibatkan tata laksana paliatif. Tata laksana paliatif merupakan tata laksana yang bertujuan untuk mengurangi gejala dan meningkatkan kualitas hidup pada penyakit yang tidak dapat disembuhkan. Tata laksana paliatif ini dapat dilakukan dengan menangani rasa nyeri yang luar biasa akibat kerusakan saraf, melegakan sumbatan empedu untuk menurunkan gejala kuning, serta melegakan sumbatan pada usus halus.
Selain itu, diet juga menjadi sangat penting karena sel-sel pankreas berfungsi untuk menghasilkan enzim pencernaan. Akibat kerusakan sel-sel tersebut, pencernaan protein dan lemak dapat terganggu hingga menyebabkan malabsorpsi, atau ketidakmampuan tubuh menyerap makanan. Menghindari makanan tinggi lemak dan tinggi protein dapat menurunkan risiko malabsorpsi. Namun, terapi lainnya dapat berupa suplementasi atau penambahan enzim-enzim sehingga makanan tersebut dapat dicerna dan diserap oleh tubuh.
Komplikasi
Komplikasi karsinoma pankreas akan mengikuti seiring perjalanan penyakit. Komplikasi ini dapat berupa penurunan berat badan akibat sel-sel tumor yang mengambil energi untuk bagian tubuh lainnya, serta penurunan nafsu makan akibat rasa mual dan malabsorpsi, akibat penurunan jumlah enzim tubuh. Selain itu, tumor pada kanker pankreas dapat menekan saluran empedu sehingga terjadi sumbatan yang kemudian mengakibatkan kuning. Tumor ini juga dapat menekan saraf-saraf di perut, sehingga menyebabkan nyeri. Tidak hanya itu, tumor juga dapat menekan usus sehingga pencernaan makanan menjadi tidak efektif.
Pencegahan
Pencegahan karsinoma pankreas dapat dilakukan dengan berhenti merokok. Dibutuhkan waktu sekitar 5-10 tahun berhenti merokok untuk menurunkan risiko kanker pankreas pada seorang perokok hingga sama dengan nonperokok. Selain itu, pencegahan dapat dilakukan dengan menjaga berat badan ideal atau menurunkan berat badan hingga menjadi ideal. Jika Anda membutuhkan penurunan berat badan, target penurunan 0,5-1 kg per minggu cukup baik. Penurunan berat badan dapat dilakukan dengan kombinasi olahraga teratur dan konsumsi makanan yang kaya sayuran, buah-buahan, dan biji-bijian utuh dalam porsi kecil. Diet kaya sayuran, buah-buahan, dan biji-bijian utuh juga dapat mencegah penyakit ini.
Kapan harus ke dokter?
Jika Anda mengalami gejala seperti penurunan berat badan yang tidak diinginkan disertai kuning atau nyeri perut, ditambah dengan adanya riwayat keluarga dengan kanker pankreas, sebaiknya Anda berkonsultasi dengan dokter. Tata laksana dini dapat menghambat perkembangan kanker dan meningkatkan kualitas hidup Anda.
- dr Hanifa Rahma
-
Dragovich, T. (2021). Pancreatic Cancer: Practice Essentials, Background, Pathophysiology. Retrieved 24 January 2022, from https://emedicine.medscape.com/article/280605-overview
-
Pancreatic cancer - Symptoms and causes. (2021). Retrieved 24 January 2022, from https://www.mayoclinic.org/diseases-conditions/pancreatic-cancer/symptoms-causes/syc-20355421
-
Puckett, Y., & Garfield, K. (2022). Pancreatic Cancer. Retrieved 24 January 2022, from https://www.ncbi.nlm.nih.gov/books/NBK518996/