Definisi
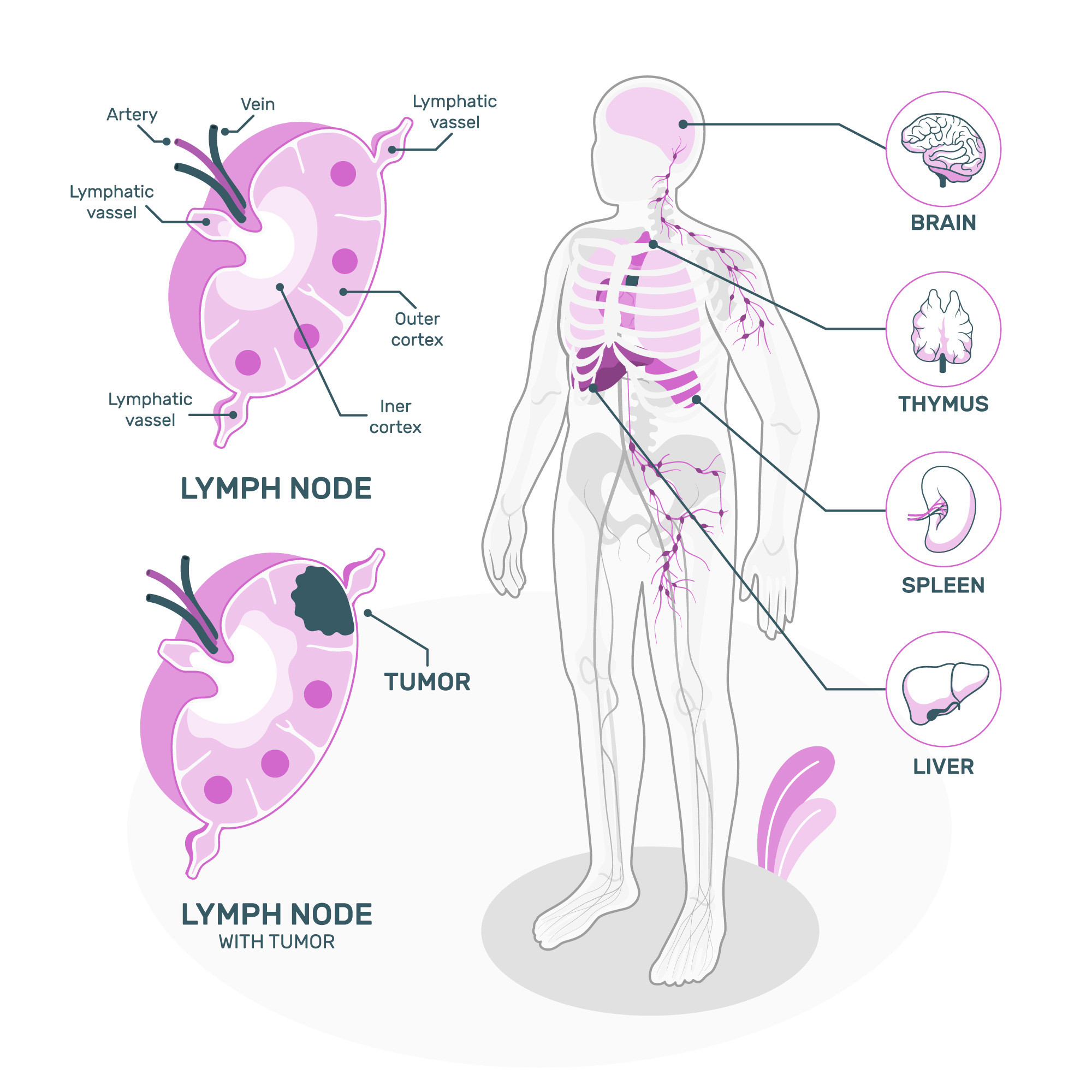
Timoma merupakan salah satu jenis tumor di kelenjar timus. Kelenjar timus adalah kelenjar yang berada di tengah rongga dada, pada bagian belakang tulang dada dan di antara paru - paru. Kelenjar timus berbentuk seperti tabung kecil dan terdiri dari dua bagian yang berukuran sama besar.
Seiring usia, ukuran dari kelenjar timus akan berubah. Kelenjar timus biasanya lebih aktif dan besar pada saat anak - anak dan remaja. Kelenjar timus akan mengecil saat usia lanjut ketika hampir seluruh jaringan akan tergantikan oleh jaringan lemak. Kelenjar ini merupakan bagian penting dari sistem limfatik atau sistem getah bening yang bertugas dalam memproduksi sel darah putih atau sel T. Sel T berfungsi dalam sistem kekebalan tubuh melawan sel kanker dan mikroorganisme penyebab infeksi.
Kelenjar timus terdiri dari 2 tipe sel, sel epitel dan limfosit. Keduanya dapat tumbuh secara tidak normal dan berubah menjadi kanker. Pada pertumbuhan sel epitel yang tidak normal akan menjadi timoma dan thymik karsinoma sedangkan pertumbuhan limfosit yang tidak normal akan menjadi hodgin atau non hodgin limfoma. Timoma sendiri bertumbuh lebih lambat dan jarang menyebar selain pada timus Anda, berbeda dengan thymik karsinoma yang berkembang lebih cepat dan menyebar ke bagian lainnya.
Penyebab
Hingga saat ini masih belum diketahui dari penyebab timoma. Penelitian masih berlangsung dan memperkirakan adanya korelasi antara virus, keturunan dan kanker lainnya. Pada beberapa penelitian, kondisi imunitas tubuh seseorang dapat mempengaruhi perkembangan timoma.
Faktor Risiko
Beberapa kondisi yang diperkirakan dapat meningkatkan risiko timoma terkait dengan gangguan pada sistem imun tubuh, diantaranya :
- Hipogammaglobulinemia
- Lupus
- Myasthenia gravis
- Aplasia sel darah merah
- Rheumatoid arthritis
- Sarkoidosis
- Kolitis ulseratif
Gejala
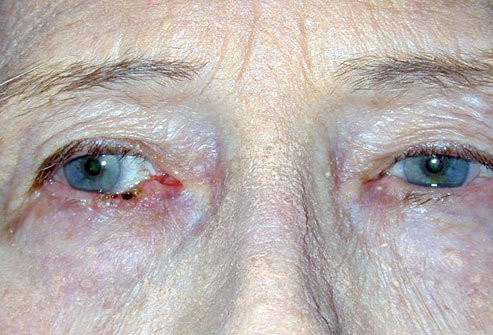
Kebanyakan pasien timoma tidak menunjukkan adanya gejala atau tanda ketika di diagnosa pertama. Lakukan pemeriksaan pada dokter Anda bila Anda memiliki gejala seperti batuk yang tidak kunjung hilang, kekurangan napas atau napas pendek, nyeri di dada, suara serak, pembengkakan pada wajah, leher, bagian atas tubuh atau lengan.
Bila Anda memiliki timoma, Anda akan menyadari adanya gejala dari salah satu sindrom paraneoplastik seperti pemandangan ganda, kelopak mata yang menutup, kelelahan dan kelemahan otot (myasthenia gravis), anemia, infeksi, diare, dan pembengkakan kelenjar limfa yang sering terjadi.
Diagnosis
Dokter dapat mendiagnosa Anda memiliki tumor setelah melakukan pemeriksaan lebih lanjut mengenai gejala yang dirasakan. Untuk melakukan diagnosa, dokter akan melakukan pemeriksaan fisik dan bertanya mengenai gejala dan riwayat medis. Anda mungkin akan diminta melakukan pemeriksaan tertentu untuk mendapatkan informasi lebih dalam dari tumor Anda seperti :
- Pemeriksaan X-ray dada
Pemeriksaan X-ray menunjukkan adanya gumpalan di dalam darah Anda dan menyediakan informasi penting untuk mendefinisikan bentuk dari tumor Anda. Tumor dengan bentuk yang jelas dan matang lebih mudah untuk diangkat pada saat operasi.
- CT Scan
Pemeriksaan CT scan dada merupakan pemeriksaan gambar yang tepat untuk memeriksa thymoma. Dokter akan menggunakan kontras atau pewarna ke dalam pembuluh darah Anda (disebut dengan kontras medium) untuk membuat tumor lebih nampak pada saat pemeriksaan. CT scan menjadi salah satu media pemeriksaan untuk mendeteksi timoma.
- MRI
MRI dapat menjelaskan gambaran detail mengenai tumor sehinggamembantu dokter untuk membedakan antara kemungkinan pertumbuhan tumor lainya. Sebagai contoh, dokter Anda akan menggunakan MRI untuk memahami lebih dalam apakah gambaran tersebut timoma atau thymik karsinoma.
- PET scan atau PET/CT
Pemeriksaan ini memasukkan gula radioaktif di dalam pembuluh darah Anda. Larutan ini memberikan pembeda disekitar sel yang menggunakan energi yang banyak seperti sel kanker.
- Biopsi
Pemeriksaan ini satu satunya cara untuk menegakkan diagnosa. Dokter akan mengangkat sel tumor dan menganalisa dengan bantuan mikroskop. Bila memungkinkan, dokter akan mengangkat seluruh tumor dan melakukan pemeriksaan pada sel. Bila dokter tidak dapat mengangkat seluruh tumor, dokter akan mengambil sampel untuk pemeriksaan.
Setelah melakukan pemeriksaan, dokter akan melakukan pengklasifikasian terkait dengan tingkat keseriusan Anda. Tingkat kanker akan membantu dokter dalam membantu pengobatan terapi. Timoma menggunakan sistem TNM yang mencakup termasuk (Tumor, Nodul dan Metastasis) :
- Tumor: Apakah terdapat tumor, seberapa besar tumornya, dan lokasi tumor
- Nodul: Apakah kanker telah menyebar pada nodul atau kelenjar limfa? Di bagian apa terdapat nodul? Berapa banyak?
- Metastasis: Apakah kanker sudah menyebar ke bagian tubuh lainnya selain timus? Bagian mana yang terkena?
Tata Laksana
Perawatan pada timoma bergantung pada berbagai faktor, meliputi tipe kanker yang Anda miliki dan tingkat kanker yang dialami. Faktor lainnya meliputi kanker yang baru di diagnosa atau muncul kembali. Beberapa pengobatan yang dilakukan seperti :
- Operasi
Dokter spesialis akan melakukan operasi pada area dada yang disebut dengan operasi thoracic untuk mengangkat tumor. Dokter mungkin akan mengangkat nodus limfa, timus atau garis paru yang dapat menyebar. Operasi merupakan tindakan standar dalam pengobatan awal timoma. Bila tidak memungkinkan untuk mengangkat seluruh tumor seluruhnya, dokter akan mengangkat sebanyak mungkin jaringan yang terkena untuk membantu mengurangi gejala
- Radiasi
Onkologis radiasi dapat mengantarkan radiasi pada area kanker dengan menggunakan terapi paparan radiasi eksternal. Terapi ini menggunakan mesin hingga Xray langsung ke tumor untuk membunuh sel kanker. Anda mungkin menerima terapi radiasi sebagai terapi sendiri atau bersamaan dengan pengobatan lainnya seperti operasi dan kemoterapi
- Kemoterapi
Penderita akan menerima obat kemoterapi untuk membunuh sel kanker bila tumor tidak dapat dihilangkan dengan operasi. Hematologis atau Onkologis juga akan meresepkan kemoterapi untuk mengecilkan tumor Anda sebelum operasi atau untuk pengobatan kanker yang kambuh kembali
- Terapi dengan target
Penderita dapat menerima terapi dengan target bila sel kanker Anda memiliki mutasi genetik yang spesifik. Terapi ini dirancang untuk membunuh mutasi genetik dari sel kanker. Terapi ini menjadi opsi terapi apabila kemoterapi tidak dapat bekerja dengan maksimal
- Immunoterapi
Immunoterapi membantu meningkatkan sistem imun tubuh sehingga dapat mengidentifikasi dan menghancurkan sel kanker. Terapi ini menjadi opsi pilihan bila pengobatan kemoterapi tidak memberikan efek yang maksimal.
- Clinical Trial (Uji klinis)
Uji klinis merupakan penelitian untuk keamanan dan efektivitas dari pengobatan kanker yang baru atau berbeda. Bergantung pada tipe kanker yang dialami, Menajdi peserta uji klinis dapat dilakukan untuk pengobatan kanker. Tanyakan pada dokter Anda bila metode ini merupakan salah satu opsi.
Dokter Anda juga menyarankan Anda untuk bekerja dengan tim paliatif untuk mendukung Anda selama diagnosa dan pengobatan kanker. Perawatan paliatif oleh tenaga profesional seperti dokter, perawat dan dokter spesialis lain yang dapat menangani gejala kanker dan efek samping yang dapat terjadi. Perawatan paliatif merupakan cara yang baik dalam penanganan sel kanker atau hasil akhir dari pengobatan.
Komplikasi
Komplikasi dari timoma dapat muncul saat pengobatan kanker. Komplikasi tersebut meliputi radiasi perikarditis, pneumonitis dan fibrosis paru. Hal ini umumnya terjadi setelah terapi radioterapi dan dapat menyebabkan kematian pasien sehingga dokter perlu mempertimbangkan risiko dan keuntungan sebelum penggunaan terapi tersebut.
Pencegahan
Pencegahan dari timoma masih belum diketahui. Hal ini karena penyebab pasti dari timoma belum diketahui sehingga saat ini belum diketahui bagaimana pencegahan timoma.
Kapan Harus ke Dokter?
Bila memiliki gejala timoma, segera berdiskusi dengan dokter mengenai penanganan yang perlu dilakukan. Dokter mungkin akan melakukan pemeriksaan fisik dan pemeriksaan lebih lanjut sebelum menegakkan diagnosa. Pasien yang sudah di diagnosa timoma memerlukan pengawasan rutin dan perawatan lebih lanjut dengan dokter untuk mengetahui efektivitas dari obat yang diberikan.
Informasikan pada dokter terkait efek samping yang dirasakan setelah terapi sehingga dokter dapat mempertimbangkan kembali terapi yang diberikan. Lakukan pemeriksaan rutin untuk menghindari kekambuhan kembali dari timoma.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Hanifa Rahma
Thymoma. (2022). Retrieved 20 February 2023, from https://emedicine.medscape.com/article/193809-overview
Thymoma (Thymic Carcinoma). (2022). Retrieved 20 February 2023, from https://my.clevelandclinic.org/health/articles/6196-thymoma-and-thymic-carcinoma
Thymoma and Thymic Carcinoma Treatment. (2023). Retrieved 20 February 2023, from https://www.cancer.gov/types/thymoma/patient/thymoma-treatment-pdq
Thymoma. (2022). Retrieved 20 February 2023, from https://www.ncbi.nlm.nih.gov/books/NBK559291/
Thymoma. (2022). Retrieved 20 February 2023, from https://www.cancercenter.com/blood-cancers/thymomas
Thymus. (2018). Retrieved 20 February 2023, from https://www.healthline.com/human-body-maps/thymus#1